CIPA (Control of Food Intake, Protein, and Anthropometry) nutritional screening is positive when one of the following conditions is met: Control of Food Intake for 48−72h <50%; Albumin <3g/dL, Body Mass Index <18.5kg/m2 or Arm Circumference ≤22.5cm. Following its validation in non-surgical inpatients, the same process was performed with surgical inpatients.
ObjectivesValidity of the CIPA screening tool in surgical inpatients by comparison with Subjective Global Assessment (SGA) and analysis of clinical outcomes
Material and methodsA prospective study of hospitalized surgical patients, evaluating the prevalence or risk of malnutrition through CIPA and SGA. Analysis of hospital malnutrition according to CIPA screening and association with the clinical outcomes of median length of stay, mortality and early readmission. Concordance between both screening methods by Kappa Index (κ), sensitivity (S) and specificity (SP).
ResultsA total of 226 patients were analysed. The prevalence of malnutrition or risk of malnutrition was identified by CIPA in 35.40% and by SGA in 30.08%. CIPA is capable of detecting patients at a greater risk of mortality during hospitalization (5% vs 0%, p=0.006), unlike the SGA (2.94% vs 1.27%, p=0.385). CIPA also detected patients with higher median length of stay (21 days, IQR 14–34 days vs 14.5 days, IQR 9–27 days, p=0.002) and rate of early readmissions (25.3% vs 8.2%, p<0.001). S and SP of CIPA vs SGA was 70.59% and 79.75% respectively; Kappa index was 0.479 (p<0.001).
ConclusionsUsing CIPA nutritional screening, the prevalence and risk of malnutrition in surgical patients is high, and they present poorer clinical outcomes, making CIPA valid and effective in this type of patients.
El cribado nutricional CIPA (Control de Ingestas, Proteínas, Antropometría) es positivo cumpliendo al menos una de las siguientes condiciones: Control de Ingestas en 48−72h <50%; Albúmina <3g/dl, Índice de Masa Corporal <18,5kg/m2 o Circunferencia del Brazo ≤22,5cm. Tras su validación en pacientes hospitalizados con patologías no quirúrgicas, se realiza el mismo proceso en pacientes quirúrgicos.
Objetivosvalidación del cribado CIPA en pacientes hospitalizados quirúrgicos mediante comparación con Valoración Global Subjetiva (VGS) y analizando el pronóstico clínico de los pacientes.
Material y métodosestudio prospectivo de pacientes quirúrgicos hospitalizados, valorando la prevalencia o riesgo de desnutrición a través de CIPA y Valoración Global Subjetiva (VGS). Análisis de desnutrición hospitalaria a través de la asociación con las variables clínicas pronósticas estancia mediana, mortalidad y reingreso precoz. Concordancia entre ambos métodos de cribado mediante índice Kappa (κ), sensibilidad (S) y especificidad (E).
ResultadosSe analizan 226 pacientes. CIPA identifica una prevalencia de desnutrición o riesgo de padecerla del 35,40%, y VGS 30,08%. CIPA es capaz de detectar al paciente con mayor mortalidad hospitalaria (5% vs 0%, p=0,006), a diferencia de la VGS (2,94% vs 1,27%, p=0,385). CIPA también detectó aquellos con mayor estancia mediana (21 días, RIC 14-34 días vs 14,5 días, RIC 9-27 días, p=0,002) y reingresos precoces (25,3% vs 8,2%, p<0,001). S y E de CIPA vs VGS: 70,59% y 79,75% respectivamente; κ=0,479 (p<0,001).
ConclusionesMediante el cribado nutricional CIPA la prevalencia de desnutrición o riesgo de padecerla en pacientes quirúrgicos es elevada, y estos cursan con peor evolución clínica, siendo válido y efectivo en este tipo de pacientes.
The high prevalence of malnutrition in hospitals has become a public health problem, with a strong impact regardless of the country or health system involved.1,2 An estimated 20 million people are affected in Europe, with an annual cost of 120,000 million euros.3 When subjected to surgical procedures, such patients are in a greater state of stress derived from surgery and its associated catabolic response. In addition, they may experience other metabolic and physiological changes, with altered gastrointestinal function, symptoms such as nausea, vomiting or postoperative pain, paralytic ileus, perioperative fasting periods, and immobilization. Impaired patient nutritional status has a clear prognostic impact upon complications, recovery and postoperative mortality,4–6 and is associated with direct increments in healthcare costs. Nutritional support is indicated for both the prevention and treatment of catabolism-malnutrition, and there is evidence that improved nutritional status contributes to the prevention of postoperative complications and helps functional recovery.4
Despite the evidence, malnutrition in hospitals is often unrecognized and therefore untreated.2,7 In recent years, enhanced awareness among healthcare professionals has led to the widespread use of nutritional screening for the early detection of patients at risk. There is no consensus as to which is the best method in clinical practice, though the Subjective Global Assessment (SGA) score is advised as a comparison tool for the validation of new screenings.8
The Spanish national CIPA (Control of Food Intake, Protein and Anthropometry [Control de Ingestas, Proteínas, Antropometría]) is a nutritional screening tool designed at Hospital Universitario Nuestra Señora de la Candelaria (HUNSC)(Santa Cruz de Tenerife, Spain), with the premise of utilizing the resources available in daily clinical practice.6,8 The screening score is positive when any of the following conditions are met: control of 48−72h intake below 50%; serum albumin <3g/dl; a body mass index (BMI) <18.5kg/m2 or alternatively arm circumference (AC) ≤22.5cm in those cases where patient body weight or height cannot be measured. In the case of negative screening scores, the tests are repeated every 10 days until hospital discharge, while the positive cases are treated, based on a therapeutic protocol associated with diet and oral nutritional supplements (ONS) according to the criterion of the professionals in charge. Screening based on the CIPA has been validated in patients with medical disorders,9 and the tool has been subjected to optimization processes in order to perfect its use in hospital practice.10 Its cost-effectiveness has also recently been demonstrated in surgical patients.11,12 The present study was designed to complete validation of the tool in surgical patients, with a view to allowing for its global application in hospitals with heterogeneous activities.
Material and methodsA prospective longitudinal study was conducted on the prevalence of malnutrition in patients admitted to surgical wards of the HUNSC between July 2016 and December 2018. The study included patients of legal age of either gender with both emergency and scheduled admissions of over 72h, and with nutritional screening performed and validated through electronic (digital) support. The study was approved by the Ethics Committee of the HUNSC, and patient data collection and inclusion complied with the hospital protocol for access to cases histories and the signing of informed consent by patients.
Variables specific to the CIPA screening procedure (control of food intake, albumin, weight, height and the BMI or alternatively AC) and SGA were recorded in 226 patients, together with epidemiological data (age, gender, admission date, hospital discharge date, type of admission, surgery) and prognostic variables (median stay, mortality and early readmission). Albumin was determined during hospital admission on the occasion of the first blood sampling of the patients on their arrival at the hospital ward. The prevalence of hospital malnutrition or risk of malnutrition was assessed, based on CIPA versus SGA upon hospital admission, with evaluation of the agreement between both tools (kappa coefficient). The sensitivity (Se) and specificity (Sp) of CIPA with respect to SGA was analyzed, taking the latter as the gold standard for validation purposes. We examined the relationship between the CIPA and SGA screening outcomes and the prognostic parameters: early readmission (in the first 31 days after hospital discharge), mortality (both in hospital and in the first 3 months after discharge), and median stay (given its high dispersion and non-normal distribution). After checking normal data distribution with the Kolmogorov-Smirnov test, a bivariate analysis was performed based on the Student t-test or Mann-Whitney U test in the case of nonparametric contrasting. The chi-squared test was used to compare categorical variables. Results for quantitative variables were reported as the mean±standard deviation (SD) or as the median and interquartile range (IQR), while qualitative variables were reported as frequencies and percentages. A significance level of 5% was used in all hypothesis tests. The SPSS version 24.0 statistical package was used throughout.
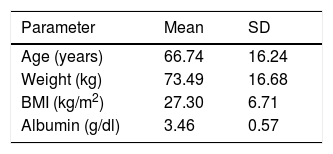
ResultsTable 1 shows the basal characteristics of the 226 patients included in the study. With regard to gender distribution, females slightly predominated, with no relation to CIPA screening positivity (33.7% of the males had a positive result versus 36.6% of the females). The prevalence of malnutrition risk according to the CIPA was 35.4% (95% confidence interval [95%CI]: 29.12–41.68), versus 30% according to the SGA score (95%CI: 24.06–36.11).
Baseline characteristics of the study sample.
| Parameter | Mean | SD |
|---|---|---|
| Age (years) | 66.74 | 16.24 |
| Weight (kg) | 73.49 | 16.68 |
| BMI (kg/m2) | 27.30 | 6.71 |
| Albumin (g/dl) | 3.46 | 0.57 |
| N | % | |
|---|---|---|
| No. subjects | 226 | 100 |
| Gender | ||
| Males | 92 | 40.7 |
| Females | 134 | 59.3 |
| Type of admission | ||
| Urgent | 182 | 82.4 |
| Scheduled | 39 | 17.6 |
| Surgical treatment | ||
| Yes | 193 | 87.3 |
| No | 28 | 12.7 |
| Department and disease | ||
| General surgery | 73 | 32.30 |
| Tumor | 23 | 31.51 |
| Biliary disease | 16 | 21.92 |
| Diverticulitis | 9 | 12.33 |
| Others | 25 | 34.24 |
| Traumatology | 96 | 42.9 |
| Hip fracture | 50 | 51.55 |
| Other fractures | 27 | 27.83 |
| Other conditions | 20 | 20.61 |
| Neurosurgery-ENT | 16 | 7.1 |
| Tumor | 9 | 56.25 |
| Others | 7 | 43.75 |
| Vascular surgery | 33 | 14.7 |
| Limb ischemia | 14 | 42.42 |
| Diabetic foot | 13 | 39.40 |
| Others | 6 | 18.18 |
| Plastic surgery- Maxillofacial surgery | 7 | 3.1 |
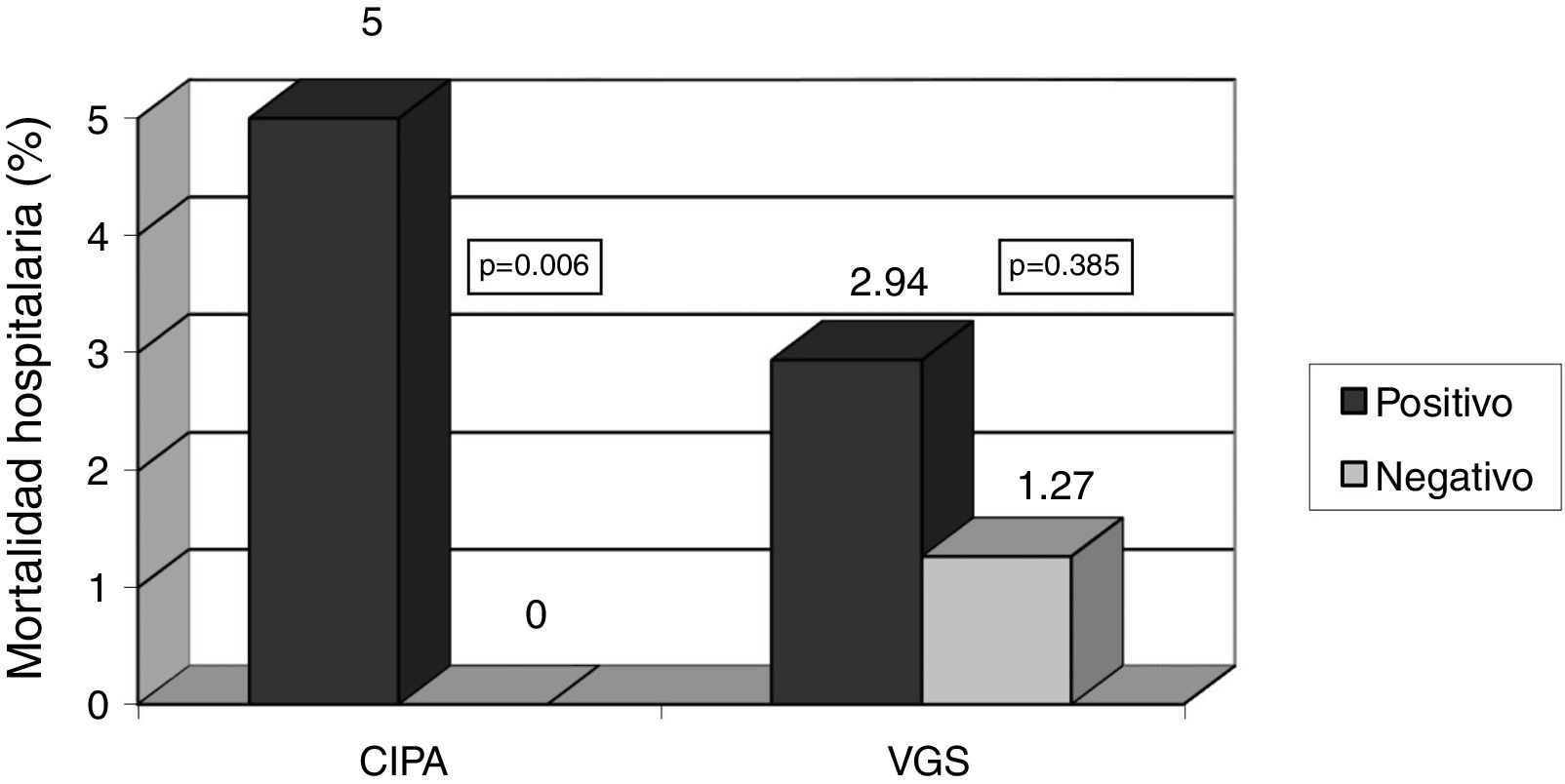
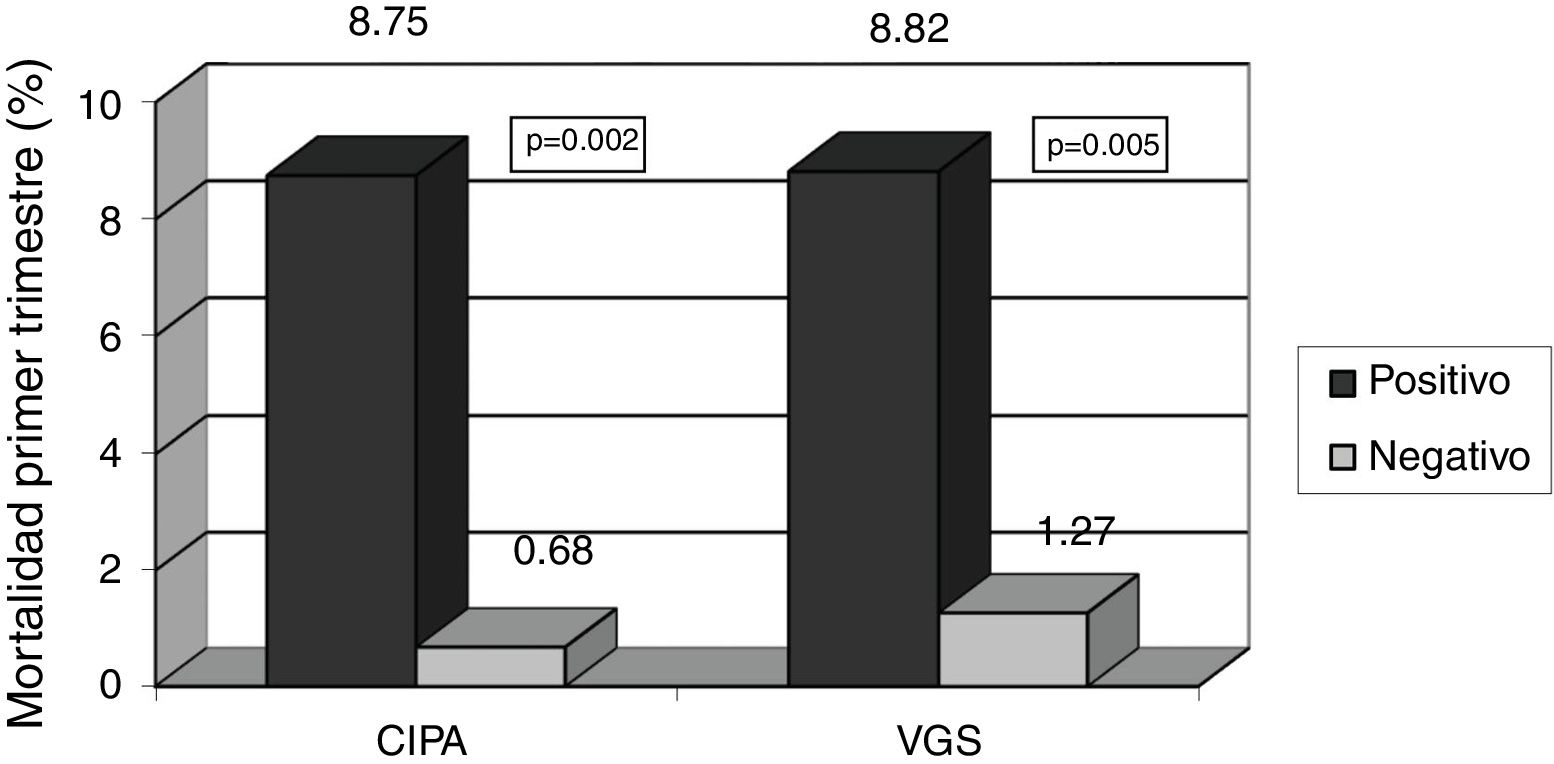
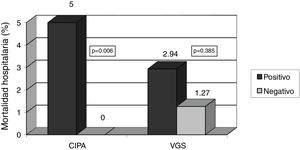
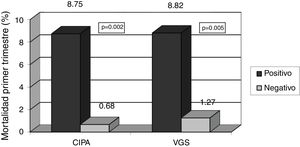
With regard to the prognostic clinical variables, the CIPA was able to detect patients with increased mortality risk during hospital admission (5% vs. 0%, p=0.006), in contrast to SGA (2.9% vs. 1.3%; p=0.385). In relation to deaths occurring in the first months after hospital discharge, the CIPA was able to detect mortality (8.7% vs. 0.7%; p=0.002) as effectively as SGA (8.8% vs. 1.3%; p=0.005) (Figs. 1 and 2).
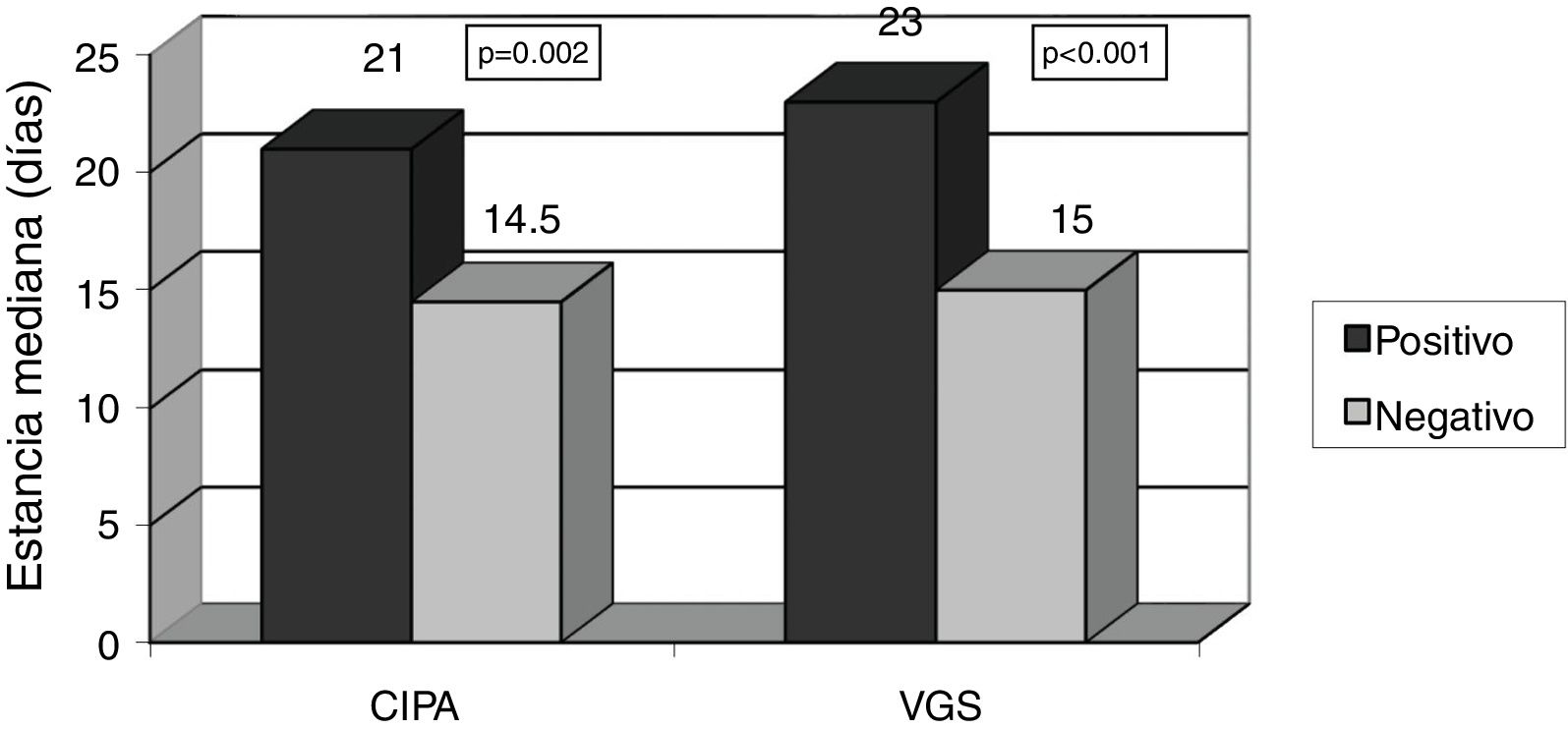
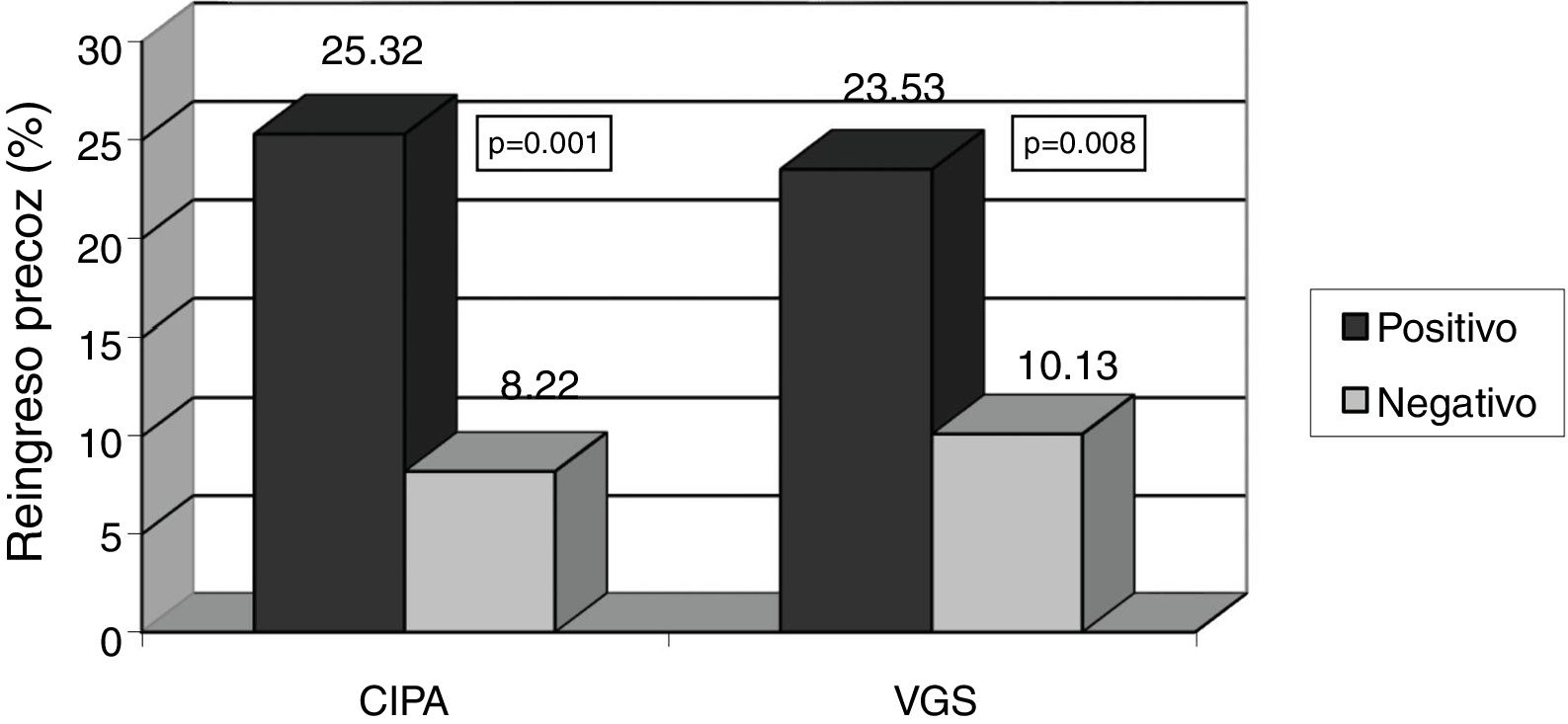
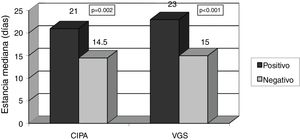
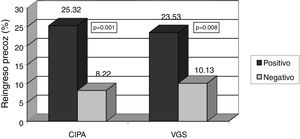
Patients with positive CIPA screening remained in hospital for longer, with a median stay of 21 days (IQR 14–34 days) versus 14.5 days in CIPA negative cases (IQR 9–27 days) (p=0.002). Similar results were obtained using SGA, with a median stay of 23 days (IQR 14.25–37.25) versus 15 days (IQR 9–25) (p<0.001) (Fig. 3). The CIPA tool was also able to detect patients at greater risk of early readmission (25.3% vs. 8.2% in the case of a negative CIPA) (p<0.001). Likewise, SGA found the risk of readmission to be 23.5% versus 10.1% in those with a negative screening test (p=0.008) (Fig. 4).
Agreement between the two screening tools, based on the kappa coefficient, was 0.479 (95%CI: 0.357−0.601; p=0.001). Taking SGA as the reference method for validation purposes, the CIPA tool yielded sensitivity and specificity values of 70.6% and 79.7%, respectively. With regard to CIPA positivity, 21.2% of the total sample analyzed had pathological albumin levels, 13.3% had decreased food intake, and 11.9% had a BMI and/or AC below normal. Of the patients with hypoalbuminemia, 48.9% corresponded to values recorded during hospital admission and before surgery. In the case of diminished albumin levels after surgery, measurement was made an average of 3.45 days (SD 2.26) after surgery. Considering the type of admission, 15% of all positive screenings corresponded to scheduled patient admissions.
DiscussionNutritional status in hospitalized patients is directly associated with resolution of the disease and its potential complications. The need for surgery adds a further stress factor requiring all healthcare professionals to assess and detect the malnutrition risk early. The incidence of malnutrition in hospitals has reached 50%, worsening the patient prognosis and increasing healthcare expenditures.1–3,10 Accordingly, current European policies recognize malnutrition as a major health problem, and recommend the development and validation of detection tools that are easy to apply and rapid.3,13,14
The prevalence of malnutrition as shown by the CIPA screening tool was found to be 35.7% in the case of nonsurgical disease,10 this figure being practically identical to that recorded in our own study. Considering the mean age of the patients, the prevalence of malnutrition was similar to that recorded in the Predyces study2 (37% in hospitalized patients over 70 years of age). Taking SGA as reference 8, the CIPA tool yields sensitivity and specificity values that grant it the validity required for screening.7,14 In addition, the items used are simple, and this favors the tool’s applicability. Furthermore, the parameters included are consistent with the criteria recently proposed by the Global Leadership Initiative on Malnutrition (GLIM) working group for the diagnosis of malnutrition.15 These data reflect the capacity of the new screening tool to detect the risk of malnutrition in hospitalized patients regardless of the reason for admission, defining the CIPA as an ideal tool for use in large hospitals that deal with a broad range of disease conditions.
Surgery implies aggression, with increased stress hormone levels and a systemic inflammatory response regardless of the disease for which surgery is indicated or the baseline condition of the patient.16 The metabolic response is characterized by increased catabolism of both glycogen and fatty acids and proteins. Protein catabolism is regarded as a key element in the functional recovery of the patient, given the possible and early loss of muscle tissue that can persist over the long term.4,16,17 Preoperative serum albumin is a good predictor of both postoperative morbidity and nutritional status.4 In our study, hypoalbuminemia was the most common factor in positive CIPA screenings, and preoperative measurement was performed in half of the cases. Recent studies have interpreted postoperative albumin as an indicator of adverse effects and not as a cause of such effects, and the recovery of albumin levels is, moreover, noted in the first 5 days after surgery.17–19 Based on these results and on the physiology of albumin, it may be affirmed that although the relationship between preoperative albumin concentration and patient prognosis is clear, further studies are needed to define the role of hypoalbuminemia after surgery.
After albumin, the control of food intake was the parameter with the strongest association with positive screening, with approximately 13% of the study sample presenting an intake below 50%. This control of intake quantifies the amount of food consumed by the patient in each dish of the four meals dispensed in the hospital (<25%; 25–50%, 50–75%, >75%) during the first 48−72hours of arrival at the hospital ward. It only proved evaluable if the patient presented a diet of over 1000kcal a day, with the inclusion of proteins. At present, with the protocols for the early reintroduction of oral feeding after surgery4,20 and the inclusion of food intake as a criterion for malnutrition by the GLIM group,15 the use of this parameter in hospital malnutrition screening affords quality and increased safety in healthcare.
The CIPA screening tool is not limited to detecting the risk of malnutrition, but can also predict those surgical patients with a poor clinical prognosis. In our study, the CIPA identified patients at increased mortality risk during hospital admission, in contrast to SGA. In recent years there has been an increase in the use of risk predictors of in-hospital mortality as an indicator of quality and for assessing the risk-benefit ratio of surgical procedures.21,22 The CIPA also detects mortality in the first months after hospital discharge and the risk of early readmission, this suggesting the ability to assess and treat patients with greater morbidity and its associated complications. The CIPA tool predicts surgical patients presenting a median23 of one additional week of admission, with the associated costs involved. The early introduction of nutritional support helps prevent complications and improves the clinical prognosis.4 The detection capacity of the CIPA screening tool is completed by combining it with a nutritional support protocol, representing an early detection and intervention method with an improvement of the clinical parameters of these patients at risk.
Surgery in itself is regarded as a risk factor for the development of complications, contributing to the proinflammatory state in a way similar to any chronic disease condition.4,16 In addition, many studies show a worsening of nutritional status during admission. In this regard, the detection of malnutrition risk throughout the hospitalization process is of crucial importance.1,2,8 In our study, most patients had an acute condition requiring emergency admission and/or surgery, but it should be noted that 15% of the cases with a positive screening result corresponded to non-emergency admissions. These results suggest the importance of the nutritional screening of all patients admitted to hospital and the need for additional studies and tools to prevent the risk of malnutrition.
The CIPA is currently the reference nutritional screening tool in hospital centers in the Canary Islands.24 Various studies have demonstrated its cost-effectiveness, specifically in patients admitted to General and Digestive Surgery.12,25 The clinical prognostic factors in a group of patients subjected to CIPA screening versus a control group (the diagnosis of malnutrition being established through standard clinical practice, without screening) were also evaluated. Although the patients at risk of malnutrition detected early by means of the CIPA had a higher Charlson index score upon admission and underwent a greater number of cancer surgeries, they exhibited a better prognosis than the controls. The study showed that CIPA screened patients had lower mortality rates, fewer transfers to critical care, and a shorter mean stay (though statistical significance was not reached).26 Although this study was conducted in a single surgical specialty, the CIPA is seen to be a tool for both risk detection and the early intervention and clinical improvement of these patients.
Malnutrition is a serious global health problem with high costs, and requires efforts and attention from both public bodies and healthcare professionals.1,2,24 This study provides further evidence on the CIPA nutritional screening tool as a useful option for detecting the risk of malnutrition in patients, regardless of the disease involved or its management, and has been validated in surgical patients. Thus, CIPA screening can detect patients with a poorer clinical prognosis using nutritional markers in a simple and effective manner.
AuthorshipJ.P. Suárez and A. Mora designed the study. The field work was supervised by J.P. Suárez and I. Llorente, and was carried out by A. Mora and A. Sánchez. C. Lorenzo and Y. Zambrano actively collaborated in the organization and updating of the data for analysis. A. Sánchez, C. Lorenzo and Y. Zambrano participated in the statistical analysis and interpretation of the results. The initial draft of the article was prepared by A. Mora and P. Suárez. All the authors contributed to the interpretation of the results and subsequent modifications. All the authors provided their critical viewpoint during preparation of the article, along with their review and approval of the final manuscript version.
Conflicts of interestThe authors declare that they have no conflicts of interest or financial ties in relation to the contents of the article.
Thanks are due to all the staff members who collaborated in the development of the CIPA screening tool, and particularly to colleagues from the Department of Endocrinology and Nutrition and the Clinical Nutrition and Dietetics Unit of Hospital Universitario Nuestra Señora de la Candelaria.
Please cite this article as: Mora Mendoza A, Suárez Llanos JP, Sánchez Morales A, Lorenzo González C, Zambrano Huerta Y, Llorente Gómez de Segura I. Validación del cribado nutricional CIPA mediante variables clínicas pronósticas en pacientes quirúrgicos hospitalizados. Endocrinol Diabetes Nutr. 2020;67:304–309.