The clinical course of type 1 diabetes mellitus (T1DM) has changed in recent decades. The aim of our study was to assess the long-term (>20 years) clinical status of a patient cohort with T1DM under a specific treatment and follow-up program.
Patients and methodsA single center, observational, cross-sectional study was conducted of a patient cohort diagnosed with T1DM in the 1986–1994 period at our tertiary university hospital. Clinical characteristics, metabolic parameters, and occurrence of chronic complications and comorbidities after >20 years of follow-up were collected. All subjects entered our specific program for patients with newly diagnosed T1D and were followed up using the same clinical protocol. Data are shown as mean (standard deviation) or as number of patients and percentage. The appropriate test was used to compare quantitative and qualitative data. A P value<0.05 was considered statistically significant.
ResultsA total of 279 patients were recorded, of whom 153 (53.6% women; mean age 46.6±8.6 years; age at onset 23.3±8.8 years; disease duration, 23.3±2.6 years) continued to attend our diabetes unit at the time of the analysis. Of these patients, 24.8% were administered continuous subcutaneous insulin infusion (CSII). Mean HbA1c in the past 5 years and in the last year were7.8±0.9% and 7.7±1.1% respectively (7.3±1.5% in those given CSII). Smoking was reported by 19.6% of patients, while 15.7% had high blood pressure and 37.9% dyslipidemia. Diabetic retinopathy was diagnosed in 20.4%, and 11.3% of the total cohort had nephropathy. Only 1.3% of our patients had a history of CVD.
ConclusionsData collected from a cohort of patients with T1DM for more than 2 decades regularly followed up with a specific program in a tertiary university hospital suggest a remarkably low prevalence of diabetic complications.
El curso clínico de la diabetes tipo 1 (DT1) ha cambiado en las últimas décadas. Nos propusimos describir las características de una población con DT1 de más de 20 años de evolución bajo el mismo programa de seguimiento desde el inicio.
Pacientes y métodoEstudio observacional de corte transversal en el que incluimos los pacientes del registro de inicios de DT1 entre 1986 y 1994 de nuestra Unidad de Diabetes. Desde 1986 todos siguen el mismo protocolo de seguimiento y tratamiento. Recogimos la presencia de complicaciones micro- y macrovasculares, factores de riesgo cardiovascular, control metabólico y tratamiento. Los datos se obtuvieron de la historia clínica informatizada. La comparación entre variables cuantitativas y cualitativas se realizó con el test apropiado en cada caso. Se consideró estadísticamente significativa una p<0,05.
ResultadosDe 279 pacientes del registro, 153 continuaban en nuestro centro (edad media±desviación estándar: 46,6±8,6 años) con una duración media de la DT1 de 23,3±2,6 años. De estos, un 53,6% eran mujeres. El 24,8% estaba en tratamiento con infusión subcutánea continua de insulina (ISCI). La media de HbA1c en el último año fue de 7,7±1,1% (7,3±1,5% en el grupo de ISCI) y de 7,8±0,9% en los últimos 5 años. Un 19,6% fumaban, 15,7% tenían hipertensión arterial y 37,9% dislipidemia. Un 20,4% presentaban retinopatía diabética y el 11,3% nefropatía. Únicamente un 1,3% presentaba antecedentes de enfermedad cardiovascular.
ConclusionesTras más de 2 décadas de evolución de la DT1, consideramos que la prevalencia de complicaciones micro- y macrovasculares en nuestros pacientes con DT1 en un programa específico de seguimiento desde el inicio de la enfermedad es baja o, en algún caso, sustancialmente inferior a la esperada.
The clinical course of type 1 diabetes mellitus (T1DM) has changed in recent decades due to multiple factors. After the Diabetes Control and Complications Trial (DCCT) and the Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) studies showed a reduction in microvascular and macrovascular complications with intensive insulin therapy, this has become the standard treatment for all patients with TDM.1,2 Intensive insulin therapy has changed over time with the advent of rapid- and slow-acting insulin analogs, the incorporation of capillary blood glucose monitoring into treatment and specific therapeutic education schemes, the use of continuous subcutaneous insulin infusion (CSII) and, more recently, the possibility of using interstitial glucose monitoring.3,4 All these factors, together with the improved prevention and management of all other cardiovascular risk factors, have had an impact on the prognosis of patients with T1DM.
Despite all these advances, metabolic control is still suboptimal in a majority of patients, as shown by the update of the Exchange registry, where only 30% of adults with T1DM over 30 years of age achieved glycosylated hemoglobin (HbA1c) levels <7%.5 In the same study, the rates of diabetic ketoacidosis and severe hypoglycemia in the previous three months in this patient group were approximately 3% and 6% respectively.5 Moreover, data have been reported in recent months regarding the prevalence of macrovascular complications and mortality in this population. Thus, cardiovascular events are the most common cause of death, especially in patients in whom the disease was diagnosed in childhood, and even in those with no nephropathy. It is estimated that the life expectancy of a 20-year-old patient with T1DM decreases by approximately eight years as a result of the disease.6,7 In clear contradiction with the above, some studies have reported that the mortality of patients with T1DM who have no renal disease is similar to that of a control population.8
The data available on the degree of metabolic control and the prevalence of microvascular and macrovascular complications in patients with long-standing T1DM in our environment are still very sparse.9,10 Based on the foregoing, we decided to assess the general clinical condition of a population of patients with T1DM who had undergone the same monitoring program since disease onset 20 years before and who attended a specialized, reference diabetes unit.
Patients and methodsThis was an observational, cross-sectional study that enrolled all patients with a recent diagnosis of T1DM who had attended at disease onset (over 15 years of age), between 1986 and 1994, the diabetes unit of the department of endocrinology and nutrition of Hospital Clínic i Universitari in Barcelona. From 1990, all patients were over 18 years of age at disease onset.
From 1986, all patients with a recent diagnosis of T1DM have been included in our unit in an intensive treatment schedule with multiple dose insulin (MDI), using the insulins available. All the patients attend a structured program of therapeutic education in diabetes and are instructed on the management of a portion control diet adjusted to age, weight, and physical activity. The blood glucose goals are a preprandial level of 90–130mg/dL and a postprandial level <180mg/dL. Patients are seen every two weeks for the first three months and monthly thereafter until one year from the start. After one year, medical visits are made every four months, with visits to reinforce therapeutic education according to individual requirements.
All the patients follow the same treatment escalation protocol, including treatment optimization with MDI (using the rapid- and slow-acting insulin analogs available at any particular time) and the use of CSII as indicated by the diabetes advisory council of Catalonia (Consell Asesor per a la Diabetes a Catalunya) and the Catalan Health Service.11 Antihypertensive and lipid-lowering treatment is also started in all patients with blood pressure and plasma lipid levels not complying with the goals of the specific national guidelines at any time.
Screening for chronic complications is also performed during the program. For diabetic retinopathy, an initial assessment is done by an ophthalmologist, along with annual non-mydriatic retinography from the fifth year after diagnosis (evaluated by an endocrinologist). All patients with images suggesting retinopathy are referred to an ophthalmologist for diagnosis and monitoring. The screening of diabetic nephropathy is based on the annual measurement of oligoalbuminuria in 24-h urine and the oligoalbuminuria/creatinine ratio in recent urine, depending on the evaluation date. The presence of diabetic neuropathy is assessed on the basis of the clinical history and on a specific physical examination for signs and symptoms, along with any supplemental examinations as required (i.e.an electromyogram). Finally, macrovascular complications are assessed based on both the clinical history and on a specific physical examination for symptoms and signs consistent with cardiovascular disease (CVD) in any of its forms. Supplemental examinations are done as required, as well as evaluations by specialists in cardiology, neurology, and cardiovascular surgery as appropriate.
Patient data were collected from the electronic clinical records of Hospital Clinic i Universitari and from the shared clinical records of the Catalan Health Service. Data collected for patients monitored at our center at the time of this study included age, sex, year of T1DM onset, time since disease onset, type of treatment (MDI, CSII, treatment with antihypertensive drugs, and lipid-lowering treatment with statins). Information was collected regarding any history of severe hypoglycemia (any episode of documented hypoglycemia that required the assistance of a third party for resolution) and hypoglycemia unawareness (score>3 in the Clarke Questionnaire12), the degree of blood glucose control (mean HbA1c over the previous 5 years and in the past year), and the presence of other cardiovascular risk factors such as smoking, high blood pressure (defined as repeated systolic blood pressure levels≥140mmHg and diastolic blood pressure levels≥90mmHg, or the use of antihypertensive treatment), and dyslipidemia (defined as the use of lipid-lowering treatment).
The presence of diabetic nephropathy was considered positive if there was any degree of this complication (including oligoalbuminuria in repeat measurements and the use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers in the absence of any history of high blood pressure or CVD). Diabetic retinopathy was classified as proliferative or non-proliferative based on ophthalmological reports in the clinical history. The presence of diabetic polyneuropathy was not assessed due to the lack of reliable data. The history of CVD included ischemic heart disease (any form, including revascularization), cerebrovascular disease (a history of transient ischemic attack or stroke), and peripheral artery disease such as a history of intermittent claudication, foot ulcers, amputation or revascularization surgery. Only episodes for which the relevant specialist report was available were taken into account.
HbA1c was measured using a Tosoh G8 Automated HPLC (high performance liquid chromatography) Analyzer (Tosoh Biosience Inc., South San Francisco, CA, USA, with DCCT standards and a normal range of 4–6%).
Statistical analysisData are given as mean±standard deviation (SD) or the number of patients and percentage. The normal distribution of continuous variables was verified using a Kolmogorov–Smirnov test. Quantitative variables were compared using parametric tests (Student's t test) or non-parametric tests (Mann–Whitney U or Wilcoxon tests) depending on their distribution. Qualitative variables were compared using a Chi-square test. A value of p<0.05 was considered statistically significant. Statistical analysis was performed using Statistical Package for Social Science (SPSS) version 22.0 software (Chicago, IL, USA).
ResultsFrom 1986 to 1994, 279 patients were entered in the registry of T1DM onsets of Hospital Clinic i Universitari. Of these, 153 (54.8%) were still attending our center more than 20 years after their diagnosis. Of the remaining 126 patients, 13 (4.7%) had died, 52 (18.6%) were being monitored at other centers, and 12 (4.3%) had moved to another region or country. No data were available for 49 (17.6%) patients.
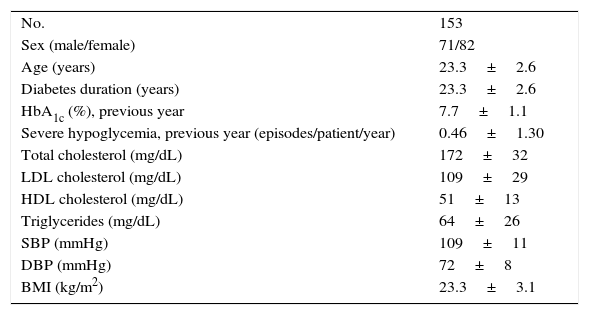
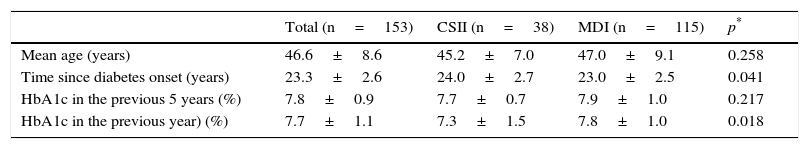
Of the 153 patients who continued to be monitored at our center, 53.6% (n=82) were females with a mean age±SD of 46.6±8.6 years (age at onset 23.3±8.8 years) and a mean T1DM duration of 23.3±2.6 years (Table 1). A quarter of the patients (24.8%) were being treated with CSII. The mean diabetes duration in this group was significantly longer as compared to the MDI group (24±2.6 vs 23±2.5 years, p=0.041). The remaining 115 patients were being treated with MDI (Table 2).
Clinical and laboratory characteristics of the patient cohort enrolled into the study.
| No. | 153 |
| Sex (male/female) | 71/82 |
| Age (years) | 23.3±2.6 |
| Diabetes duration (years) | 23.3±2.6 |
| HbA1c (%), previous year | 7.7±1.1 |
| Severe hypoglycemia, previous year (episodes/patient/year) | 0.46±1.30 |
| Total cholesterol (mg/dL) | 172±32 |
| LDL cholesterol (mg/dL) | 109±29 |
| HDL cholesterol (mg/dL) | 51±13 |
| Triglycerides (mg/dL) | 64±26 |
| SBP (mmHg) | 109±11 |
| DBP (mmHg) | 72±8 |
| BMI (kg/m2) | 23.3±3.1 |
Data given as n or mean±standard deviation.
BMI: body mass index; DBP: diastolic blood pressure; SBP: systolic blood pressure.
Characteristics of the overall group of patients and patients treated with CSII or MDI.
| Total (n=153) | CSII (n=38) | MDI (n=115) | p* | |
|---|---|---|---|---|
| Mean age (years) | 46.6±8.6 | 45.2±7.0 | 47.0±9.1 | 0.258 |
| Time since diabetes onset (years) | 23.3±2.6 | 24.0±2.7 | 23.0±2.5 | 0.041 |
| HbA1c in the previous 5 years (%) | 7.8±0.9 | 7.7±0.7 | 7.9±1.0 | 0.217 |
| HbA1c in the previous year) (%) | 7.7±1.1 | 7.3±1.5 | 7.8±1.0 | 0.018 |
Data are given as mean±standard deviation.
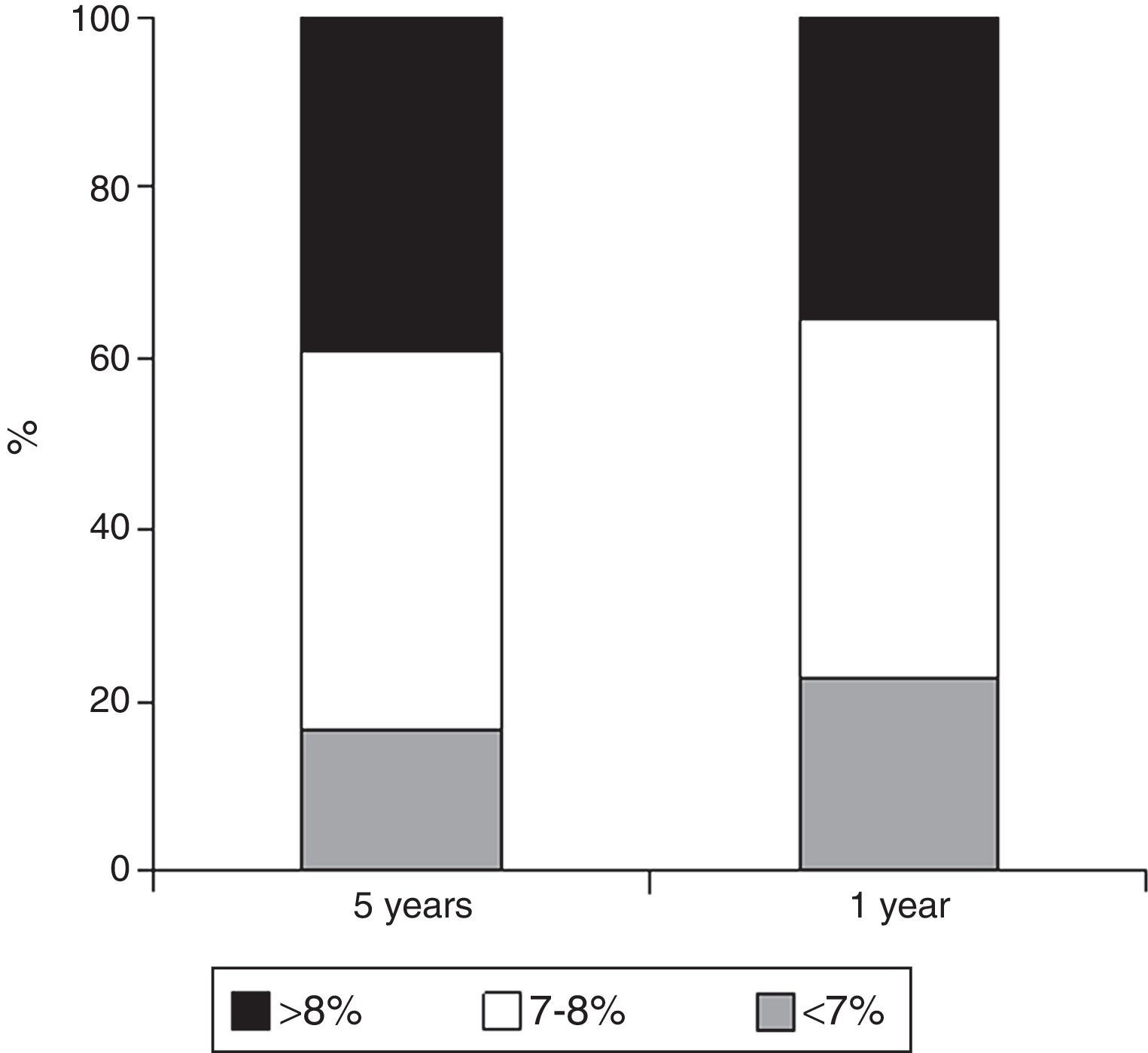
The mean HbA1c value in the previous year was 7.7%±1.1% and 7.8±0.9 in the previous five years; one fifth of patients had HbA1c levels<7%, and two-thirds had HbA1c values<8% (Fig. 1). A comparison of HbA1c values of patients treated with MDI and with CSII showed the latter to have had a significantly better blood glucose control over the previous year (7.3%±1.5% vs 7.8%±1%; p=0.018) and a numerically better control over the previous five years (7.7%±0.7% vs 7.9%±1%; p=0.217, Table 2). A history of severe hypoglycemia was found in 22.2% of patients (n=34), while a history of hypoglycemia unawareness was found in 16% (n=25).
As regards cardiovascular risk factors, 30 patients (19.6%) smoked or had smoked, 24 (15.7%) had been diagnosed with high blood pressure, and 58 (37.9%) had dyslipidemia. Fifty of these latter patients were on statin treatment. The prevalence of smoking, dyslipidemia, and statin treatment was significantly greater in patients with some kind of chronic complication as compared to those with no complications (smoking 32.4% vs 16%, p=0.033; dyslipidemia 53.8% vs 33.6%, p=0.026; statin-treated dyslipidemia 52.5% vs 26.4%, p=0.003). No significant differences were found in the high blood pressure rate (23.1 vs 13.6%; p=0.168). In patients treated with CSII, a trend was seen to lower smoking and high blood pressure rates as compared to patients on MDI (13.2% vs 23.4% and 10.5% vs 17.5%; p=0.182 and p=0.304 respectively).
Some grade of diabetic retinopathy was seen in 20.4% of patients (n=31) (only six of these, 3.9%, had proliferative retinopathy), and 11.3% (n=17) had diabetic nephropathy. One patient underwent a kidney and pancreas transplant. The CSII showed a non-significant trend to a lower prevalence of retinopathy (13.2% vs 20.4%; p=0.201) and nephropathy (8.1 vs 11.3%; p=0.485).
Only 1.3% (n=2) of the patients had a history of any CVD after suffering T1DM for more than 20 years. Both had a stroke. The first of these patients was a 41-year-old male with a disease duration of 23 years, a smoker with diabetic retinopathy and a mean HbA1c value of 8.4% over the previous five years. The second patient was a 55-year-old female with a disease duration of 28 years who also had high blood pressure, dyslipidemia, retinopathy, and diabetic neuropathy. Her mean HbA1c value over the previous five years was 8.1%. There was no difference in blood glucose control between patients with and without chronic (microvascular and macrovascular) complications.
DiscussionOur sample of patients with T1DM monitored since disease onset and with diabetes duration longer than 20 years showed a low prevalence of chronic complications, with a 20% rate of retinopathy (4% of proliferative retinopathy) and nephropathy and CVD rates of 11% and 1% respectively. These data demonstrate that the implementation of a specific treatment and monitoring scheme for patients with T1DM from disease onset may lead to most these patients remaining free of chronic complications for many years after diagnosis.
Soedamah-Muthu et al. recently reported the results of a model for predicting complications in T1DM developed using data from the EURODIAB Prospective Complications Study (PCS, 1973 patients with T1DM duration of 11.5 years recruited in the 1989–1991 period). The model was validated in three prospective cohorts of patients with T1DM with no complications at the start of several studies: the Epidemiology of Diabetes Complications (EDC, 878 patients recruited in 1988–1990 and 1996–1998 with T1DM duration ranging from 18.6 to 22.4 years), Finnish Diabetic Nephropathy (FinnDiane, 2999 patients recruited between 1994 and 2009 with a mean T1DM duration of 19 years), and Coronary Artery Calcification in Type 1 Diabetes studies (CACTI, 580 patients recruited between 2000 and 2002 with a T1DM duration of 22.7 years).13 In the selected populations of these studies, CVD rate ranged from 1.9% in the EURODIAB PCS study (T1DM duration, 11.5 years) to 11.1% in the EDC study (26.4 years), with increasing CVD prevalence with longer T1DM duration. In the other studies, the prevalence of CVD was 6.3% in the original EDC (18.6 years), 5.3% in the FinnDiane, and 3.2% in the CACTI study. CVD prevalence in our study was markedly lower as compared to the above studies. It was also lower as compared to a cohort of 1382 patients from the Catalan public registry of patients starting CSII (5.1%, 16 years of T1DM duration).11 In our region (Catalonia), a study with characteristics similar to the one reported here (although it recorded annually, from disease diagnosis, data on blood glucose control, risk factors, and the development of complications) but including a little less than half the number of patients has recently been published. The above mentioned study shows data for a subgroup (n=77) of all patients with T1DM monitored continuously from diagnosis in the period 1985–1994 (n=130) and who agreed to participate in it at the endocrinology department of a tertiary care university hospital specializing in T1DM care (mean age, 47 years; mean disease duration, 22 years). The prevalence of CVD in this study was 3.9% (n=3), somewhat greater than that found in our study. These differences may be explained, at least partly, by the higher prevalence rates of other cardiovascular risk factors in patients from that study: 35.1% of smoking, 28.6% of high blood pressure, and 46.8% of dyslipidemia.9 Both prevalence rates are much lower than those seen in the intensive treatment group of the DCCT/EDIC study (18.5 years from the onset of T1DM, a 9% prevalence of CVD).14 However, because of the characteristics of both studies (this one and ours) and the low number of CVD events, these results should be regarded with caution.
As regards the presence of microvascular complications, no significant differences were seen in the prevalence of retinopathy and diabetic nephropathy as compared to the Colom et al. study (20.4% and 11.3% in our study and 20.4% and 10.4% in the prior study respectively).9 Although this was not an objective of our study, no relationship was seen between HbA1c over the previous five years and chronic complications. By contrast, the prior study found metabolic control in the first five years and during overall monitoring to be related to microangiopathic complications.9 These prevalence rates agree with those seen in the cohort of the intensive treatment group from the start of the DCCT/EDIC study (retinopathy 21% and nephropathy 9%).12 It should be noted that in the Cantón et al. study published in 2004, which analyzed the prevalence of complications in a representative sample of the Catalan population with T1DM 10 years after disease onset, the prevalence rates of retinopathy and nephropathy were 7.6% and 10% respectively.15
As regards blood glucose control, HbA1c in the previous year (approximately 7.6%) and the proportion of patients over the previous five years with HbA1c<7% (20–25%) were similar in both studies. In our case, using CSII therapy in a proportion of patients similar to that found in neighboring European countries, somewhat better HbA1c values were achieved despite the fact that this therapy is started in patients who do not achieve blood glucose goals with MDI and who have longer mean disease duration. Unfortunately, no data are available regarding the use of CSII therapy in the Colom et al. study.9 Finally, it should be noted that, as in other studies, the proportion of patients with T1DM and long-standing disease with an impaired awareness of hypoglycemia was close to 20%. All these data together illustrate both the difficulties encountered and the room for improvement in the long-term maintenance of control in patients with T1DM, even in health care centers highly specialized in the management of this disease.
We are aware of the significant limitations of our study. This was an observational, cross-sectional, and retrospective study where data were collected from computer records completed by physicians in standard clinical practice, with the resultant possibility of errors in event and data recording. Unfortunately, no information is available regarding those patients who discontinued monitoring at our unit (almost 50%). Data collected from computer records did not allow us to obtain reliable data regarding the incidence of non-severe hypoglycemia in our cohort, weight change over time, the specific drugs used during the monitoring period, or changes in the specific therapeutic education program during monitoring. Finally, this study was conducted at a specialized unit in a university hospital and included no pediatric patients, and its results cannot therefore be extrapolated.
To sum up, more than two decades since T1DM onset, the prevalence of microvascular and macrovascular complications in our patients with T1DM in a specific follow-up and control program since disease onset may be considered to be low or, in some cases, markedly lower than expected. However, the results as regards glucose control demonstrate the failure to achieve strict glycemic goals in a high proportion of patients.
Conflicts of interestThe authors state that they have no conflicts of interest with regard to this manuscript.
Please cite this article as: Amor AJ, Cabrer M, Giménez M, Vinagre I, Ortega E, Conget I. Situación clínica de una cohorte de pacientes con diabetes tipo 1 más de 2 décadas después del inicio. Resultados de un programa específico de seguimiento en una unidad de referencia. Endocrinol Nutr. 2016;63:339–344.