To assess the epidemiology of acromegaly in the city of Guayaquil, Ecuador, and to compare our results to those reported in the literature.
Patients, material and methodsAn analysis was made of retrospective and prospective data from all patients with acromegaly attending endocrinology clinics at the 4 main hospitals of the public health network of Guayaquil from January 2000 to December 2014. Age at diagnosis, estimated delay in diagnosis, imaging studies of pituitary gland, basal growth hormone (GH) level, GH after an oral glucose tolerance test (OGTT-GH), and serum levels of insulin-like growth factor 1 (IGF-1) were recorded. Incidence and prevalence of the disease were estimated using information from the 2010 census of population and housing.
ResultsForty-eight cases were recorded in the study period in 17 males (35.4%) and 31 females (64.5%); M/F ratio=1.8:1. Mean age at diagnosis was 47.3±16.8 years (range 18–86). Delay in diagnosis was 7.3±6.3 years (range 1–30). Mean age at diagnosis was 47.9±18.2 years in males and 46.3±15.8 years in females. Delay in diagnosis was 10.2±7.9 and 5.7±3.9 years in males and females, respectively. Prevalence of acromegaly is 18.7 cases per million inhabitants, and incidence of acromegaly 1.3 cases per million people per year.
ConclusionsAcromegaly predominates in females, and is diagnosed in the fourth decade with a delay of approximately 8 years, usually even longer in males. Incidence and prevalence are lower than reported in international series. The disease is underdiagnosed and underreported in Ecuador.
Evaluar la epidemiología de la acromegalia en la ciudad de Guayaquil (Ecuador) y comparar nuestros resultados con los reportados en la literatura.
Pacientes, material y métodosEstudio de recolección de datos retrospectivos y prospectivos de todos los pacientes con acromegalia que acudieron a los consultorios de endocrinología de los 4 principales hospitales de la red pública de salud en la ciudad, desde enero de 2000 hasta diciembre de 2014. Se registró la edad al diagnóstico, tiempo estimado de retraso en el diagnóstico, estudios de imagen de hipófisis, nivel basal de la hormona de crecimiento (GH), GH después de la sobrecarga oral de glucosa (SOG-GH) y concentraciones séricas de factor de crecimiento insulínico 1 (IGF-1). Calculamos la incidencia y prevalencia de la enfermedad utilizando la información del censo de población y vivienda del año 2010.
ResultadosSe registraron 48 casos en el periodo de estudio, de los cuales 17 eran hombres (35,4%) y 31 mujeres (64,5%); relación M/H=1,8:1. El promedio global de edad al diagnóstico fue 47,3±16,8 años (rango 18 a 86). El tiempo de retraso en el diagnóstico fue 7,3±6,3 años (rango 1 a 30). En los hombres el promedio de edad al diagnóstico fue de 47,9±18,2 años y en las mujeres de 46,3±15,8 años. El tiempo de retraso en el diagnóstico fue de 10,2±7,9 y de 5,7±3,9 años en hombres y mujeres, respectivamente. La prevalencia de acromegalia es 18,7 casos/millón habitantes y la incidencia es de 1,3 casos/millón personas/año.
ConclusionesExiste predominio de la enfermedad en mujeres, se diagnostica en la cuarta década, con un retraso en el diagnóstico de alrededor de 8 años, que suele ser aún mayor en hombres. La incidencia y prevalencia son más bajas que las descritas en series internacionales. Existe subdiagnóstico y subregistro de la enfermedad en nuestro país.
Acromegaly is an uncommon disease, associated with significant morbidity and a high mortality rate, due to the prolonged hypersecretion of growth hormone (GH) and to excess production of insulin-like growth factor 1 (IGF-1), originating in the vast majority of cases in a GH-secreting adenoma.1–3
The international literature provides different figures on the epidemiology of acromegaly in populations from different regions and countries. At the end of the 1990s, national registries of acromegaly started to be created to establish the epidemiological characteristics of the disease and to design adequate diagnosis and treatment strategies. The best organized registries of cases of acromegaly are those of Spain, Belgium, and Germany.4–6
In Latin America, a similar initiative, the National Epidemiological Program of Acromegaly of Mexico, Epiacro, has already issued its first report on the epidemiology of the condition.7
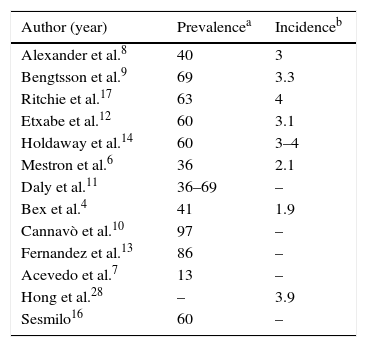
Most series report prevalence figures ranging from 40 to 95 cases per million population, with a mean estimated prevalence of approximately 69 cases per million population4,6–17 (Table 1). However, figures usually differ, depending on the region or country examined. For instance, the overall prevalence in Mexico is 13 cases per million population.7
Main series reporting the epidemiology of acromegaly.
| Author (year) | Prevalencea | Incidenceb |
|---|---|---|
| Alexander et al.8 | 40 | 3 |
| Bengtsson et al.9 | 69 | 3.3 |
| Ritchie et al.17 | 63 | 4 |
| Etxabe et al.12 | 60 | 3.1 |
| Holdaway et al.14 | 60 | 3–4 |
| Mestron et al.6 | 36 | 2.1 |
| Daly et al.11 | 36–69 | – |
| Bex et al.4 | 41 | 1.9 |
| Cannavò et al.10 | 97 | – |
| Fernandez et al.13 | 86 | – |
| Acevedo et al.7 | 13 | – |
| Hong et al.28 | – | 3.9 |
| Sesmilo16 | 60 | – |
Acromegaly is an uncommon disease in terms of new cases diagnosed, with an estimated incidence of approximately 3–4 cases per million population.14 Its incidence in Spain is around 2.5 cases per million population per year.6,12
Almost all series show a greater incidence in females, except the Belgian registry, where very similar proportions for the sexes were reported.4 In the Epiacro study, females accounted for 60% of cases.7 Patients are usually diagnosed between the fourth and sixth decades of life, and the estimated time delay from symptoms to clinical or biochemical diagnosis ranges from 9 to 35 years.3,16
In Ecuador there is no epidemiological registry of cases of acromegaly. This paper represents the first attempt to investigate the epidemiological characteristics of the disease in Ecuador. For this purpose, a regional search was made of patients diagnosed with acromegaly (ICD: E422) attending any of the main four hospitals of the public health network in the city of Guayaquil from January 2000 to December 2014.
This study was intended to assess the epidemiology of acromegaly in Guayaquil, the most populous city in Ecuador,18 and to compare our results to those reported in the international literature.
Participants, patients and methodsRetrospective and prospective data were collected from visits to the outpatient clinics of endocrinology departments of the participating hospitals during the study period (2000–2014). The patient data recorded included sex, age, age at diagnosis, time from symptom start to diagnosis, biochemical tests performed to confirm the clinical diagnosis, pituitary imaging studies, pathology and immunohistochemistry when available, treatments performed (medical or surgical), associated comorbidities, and the presence of recurrence or cure.
The laboratory data recorded (all at diagnosis) included baseline growth hormone (GH) level, IGF-1 and GH nadir after a 75-g oral glucose tolerance test (GH-OGTT). GH and IGF measurements were performed (by chemiluminescence) at each center and were reported as normal, high, or low based on local reference values.
A biochemical diagnosis of acromegaly was established when nadir GH after a 75g glucose load was greater than 1ng/mL and there was also an elevated IGF-1 level for age and sex. The cut-off point used to define controlled acromegaly was a GH reduction to <1ng/mL after GH-OGTT and normal IGF-1 levels for age and sex.19,20 Disease recurrence was defined as the detection of elevated random GH, elevated IGF-1 (for age and sex), and GH after OGTT>1ng/mL.21 Postoperative cure was defined as GH<1ng/mL after OGTT and/or normal IGF-1.20
The classification of a pituitary tumor as microadenoma or macrodenoma based on size and its local extension, the type of treatment used (medical, surgical, radiotherapy) and the availability of histopathology staining or otherwise were recorded. Study discontinuation due to follow-up losses or death was also recorded.
The comorbidities assessed included hypopituitarism, impaired carbohydrate metabolism, systemic hypertension, visual field defects, goiter, neoplasms, ischemic heart disease, biliary stones, osteoarthritis, and obstructive sleep apnea.
Records that did not include all the data required by the study design were only utilized for calculating prevalence and incidence, but not for the analysis of any other variables.
The ethics committee of the hospital of the National Police Guayaquil No. 2 gave its consent for case collection.
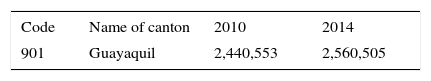
To calculate the incidence and prevalence of the disease, information from the 2010 population and housing census provided by the National Statistics and Census Institute (INEC) of Ecuador18 and the projected Ecuadorian population by calendar year and canton for 2014 were used (Table 2). According to these data, Guayaquil, with a surface area of 345km2, has a population of 2,560,505 inhabitants and accounts for 15.7% of the total population in Ecuador.22 The method reported by Greenberg et al.22 was used to estimate prevalence and incidence.
Projection of the Ecuadorian population by calendar year and canton.
| Code | Name of canton | 2010 | 2014 |
|---|---|---|---|
| 901 | Guayaquil | 2,440,553 | 2,560,505 |
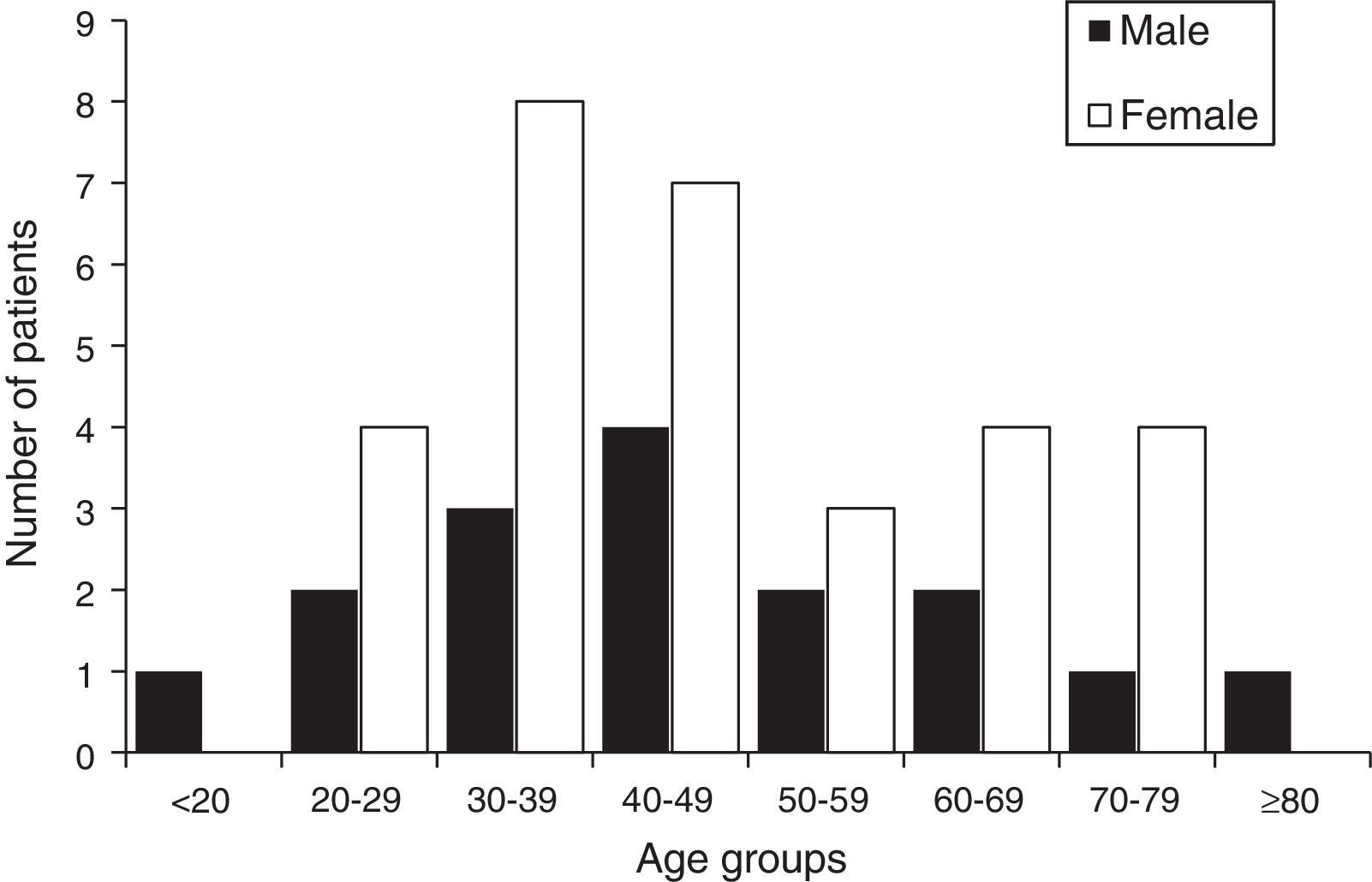
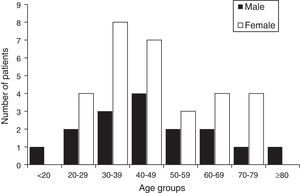
From January 2000 to December 2014, acromegaly was diagnosed in 48 patients in Guayaquil, 17 males (35.4%) and 31 females (64.5%), with a F/M ratio of 1.8:1. The mean age at diagnosis was 47.3±16.7 years (range, 18–86 years). Cases were categorized by age groups at diagnosis, by decade from <20 to >80 years, and by sex (Fig. 1). A majority of patients had an age at diagnosis ranging from 30 to 49 years. One patient at diagnosis was under 20 and another was more than 80 years old.
There were more females than males in all the age groups, but there were no females at either extreme of age.
The mean estimated time between symptoms and diagnosis was 7.3±6.3 years (range, 1–30 years). The mean age at diagnosis was 47.8±18.2 years in males (range, 18–86 years) and 46.3±15.8 years in females (range, 18–75). The mean delay in diagnosis was 10.2±7.9 years in males (range, 2–30) and 5.7±3.9 years in females (range, 1–17).
The estimated prevalence of acromegaly was 18.7 cases per million population, and its incidence was 1.3 cases per million population per year.
Biochemical diagnosis of the disease was performed in all patients by measuring levels of basal GH, GH after an oral glucose tolerance test, and IGF-1. The imaging test used in almost all cases (84%) was magnetic resonance imaging, which showed macroadenomas in 69% and microadenomas in 18% (the result of the imaging test was not reported in 4 patients).
Eighty-one percent of patients underwent surgery (using a frontotemporal or transsphenoidal approach), 12% received drug treatment (somatostatin analogs or dopamine agonists), and 39% combined treatment (surgery and drugs). One patient was given standard external radiotherapy, while the treatment administered was not recorded in two cases.
Persistent disease was reported in 19 out of 33 patients (a 57% postoperative persistence rate), one patient (with microadenoma) achieved postoperative cure (3%), while information was not available for 13 patients (39%). As data on the subsequent course were available for only 20 patients, persistence could have been as high as 95%. The mean follow-up time in patients with postoperative persistence was 8.7±10 months (range, 1–36 months).
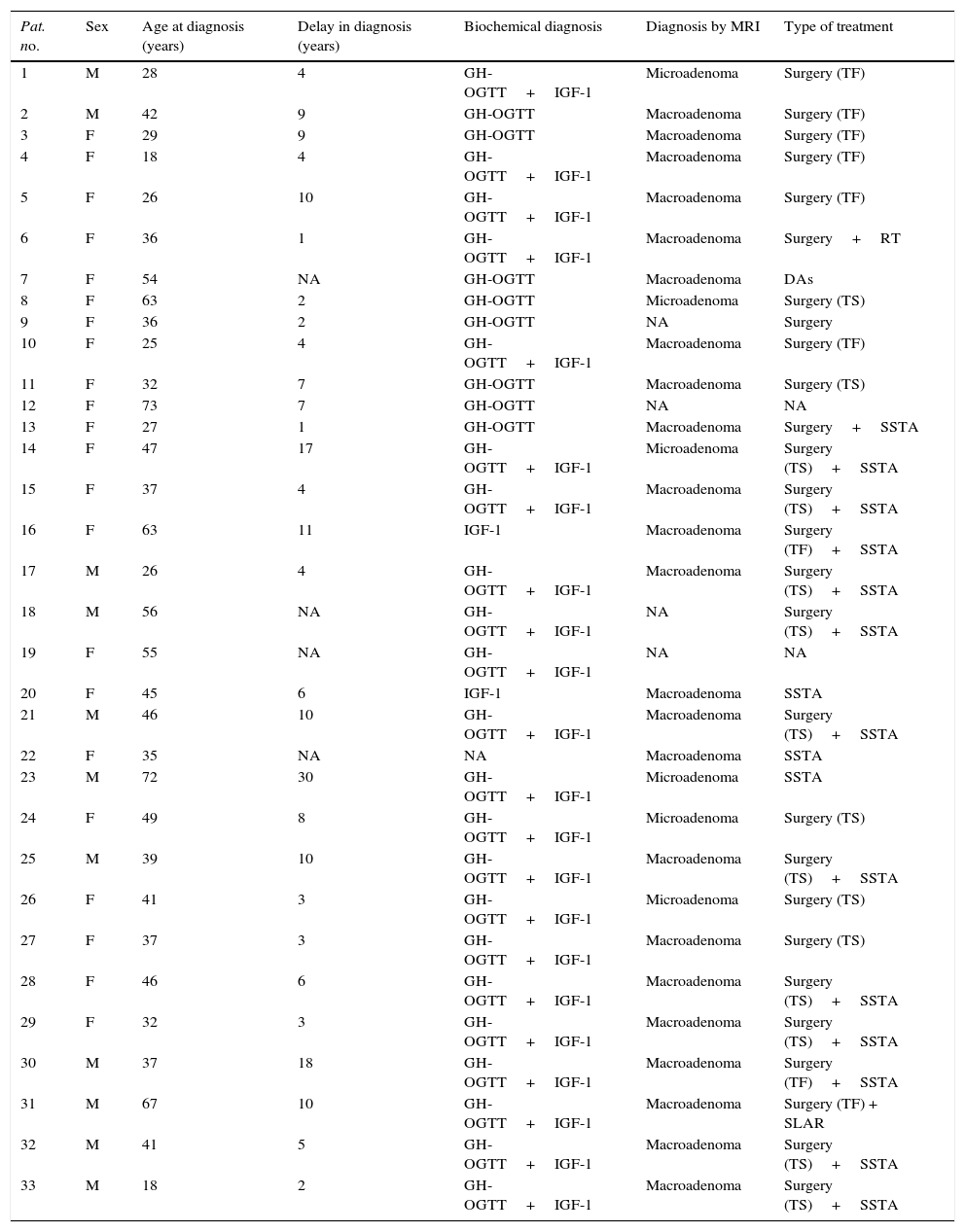
Table 3 shows the clinical, demographic, biochemical, and radiographic characteristics of 33 patients for whom complete information was available. Information on the imaging test and treatments performed could not be obtained for 15 patients.
Demographic, biochemical, and radiographic characteristics of the 33 patients with acromegaly for whom complete information was available.
| Pat. no. | Sex | Age at diagnosis (years) | Delay in diagnosis (years) | Biochemical diagnosis | Diagnosis by MRI | Type of treatment |
|---|---|---|---|---|---|---|
| 1 | M | 28 | 4 | GH-OGTT+IGF-1 | Microadenoma | Surgery (TF) |
| 2 | M | 42 | 9 | GH-OGTT | Macroadenoma | Surgery (TF) |
| 3 | F | 29 | 9 | GH-OGTT | Macroadenoma | Surgery (TF) |
| 4 | F | 18 | 4 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TF) |
| 5 | F | 26 | 10 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TF) |
| 6 | F | 36 | 1 | GH-OGTT+IGF-1 | Macroadenoma | Surgery+RT |
| 7 | F | 54 | NA | GH-OGTT | Macroadenoma | DAs |
| 8 | F | 63 | 2 | GH-OGTT | Microadenoma | Surgery (TS) |
| 9 | F | 36 | 2 | GH-OGTT | NA | Surgery |
| 10 | F | 25 | 4 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TF) |
| 11 | F | 32 | 7 | GH-OGTT | Macroadenoma | Surgery (TS) |
| 12 | F | 73 | 7 | GH-OGTT | NA | NA |
| 13 | F | 27 | 1 | GH-OGTT | Macroadenoma | Surgery+SSTA |
| 14 | F | 47 | 17 | GH-OGTT+IGF-1 | Microadenoma | Surgery (TS)+SSTA |
| 15 | F | 37 | 4 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TS)+SSTA |
| 16 | F | 63 | 11 | IGF-1 | Macroadenoma | Surgery (TF)+SSTA |
| 17 | M | 26 | 4 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TS)+SSTA |
| 18 | M | 56 | NA | GH-OGTT+IGF-1 | NA | Surgery (TS)+SSTA |
| 19 | F | 55 | NA | GH-OGTT+IGF-1 | NA | NA |
| 20 | F | 45 | 6 | IGF-1 | Macroadenoma | SSTA |
| 21 | M | 46 | 10 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TS)+SSTA |
| 22 | F | 35 | NA | NA | Macroadenoma | SSTA |
| 23 | M | 72 | 30 | GH-OGTT+IGF-1 | Microadenoma | SSTA |
| 24 | F | 49 | 8 | GH-OGTT+IGF-1 | Microadenoma | Surgery (TS) |
| 25 | M | 39 | 10 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TS)+SSTA |
| 26 | F | 41 | 3 | GH-OGTT+IGF-1 | Microadenoma | Surgery (TS) |
| 27 | F | 37 | 3 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TS) |
| 28 | F | 46 | 6 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TS)+SSTA |
| 29 | F | 32 | 3 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TS)+SSTA |
| 30 | M | 37 | 18 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TF)+SSTA |
| 31 | M | 67 | 10 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TF) + SLAR |
| 32 | M | 41 | 5 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TS)+SSTA |
| 33 | M | 18 | 2 | GH-OGTT+IGF-1 | Macroadenoma | Surgery (TS)+SSTA |
DAs, dopamine agonists; SSTA, somatostatin analog; F, female; IGF-1, insulin-like growth factor-1; M, male; RT, radiotherapy; GH-OGTT, GH after oral glucose tolerance test. TS, transsphenoidal approach; TF, transfrontal approach.
In Ecuador there is no epidemiological registry of cases of acromegaly. To our knowledge, this is the first series reported in a population sample from Ecuador. This article summarizes the most important epidemiological data regarding the incidence, prevalence, sex distribution, age at diagnosis, and delay time to diagnosis of acromegaly in Guayaquil.
Acromegaly is an uncommon disease, as reported in most of the main series published in the international literature. In Europe, for example, its prevalence ranges from 40 to 95 cases per million population with an estimated mean incidence of approximately 3–4 cases per million population.3,9,12,14,17 The prevalence reported in this study (18 cases per million inhabitants) is lower than the prevalence reported internationally, which suggests the existence of substantial underdiagnosis and that the disease is probably underestimated, not only because of undiagnosed cases, but also because not all patients with acromegaly seen at the different hospitals of the city (and the country) are included.
The disease has been shown to predominate in females in all the series reported,23 accounting for 51–61% of all cases6,16,24–27; only the Belgian registry found a similar proportion of cases in males and females (51%/49%).4 Acromegaly is diagnosed most commonly in middle-aged people, and there is a considerable time delay from the occurrence of the first symptoms to diagnosis.2,3 In Spain, the mean age at diagnosis is 45 years,16 with an estimated time from symptom occurrence to diagnosis of 6±6 years; the mean age at diagnosis in Mexico is 41.7 years.7 Our series confirms the predominance of acromegaly in females (64.5%), with a similar mean age at diagnosis (47 years) and a similar estimated time with symptoms before diagnosis (7.29±6.32 years). As regards incidence, it is usually higher in international series (3–4 cases/million)4,6–9,12,14,15,17,28 than the rate of 1.3 cases per million population per year found in our study.
Transsphenoidal surgery is recognized as the primary treatment for acromegaly.3,15,29 The main treatment in our series was transsphenoidal surgery (in 81% of patients), followed (and sometimes preceded) by somatostatin analogs (sustained-release octreotide). Overall, the surgical cure rate was much lower (3%) than those of surgical series reported by other reference hospitals, ranging from 21% to 95%.20,23–25 According to the Spanish REA study, the cure rate was 38.4% over the previous decade.6 We found a persistence rate of 57%, which could be much higher because of high patient loss. These data reflect the fact that the records are taken both from patients attending hospitals experienced in treating this disease and from other centers less familiar with it.
This first analysis of the epidemiological data on acromegaly in Ecuador provides figures very similar to those reported in other series as regards age at diagnosis, sex distribution, and delay in diagnosis, as well as the proportion of microadenomas and macroadenomas. By contrast, the incidence and prevalence rates reported in the literature are higher than those found in our series.
This study has some strengths and several limitations. Its strengths include the fact that this is the first study to collect epidemiological information on acromegaly in Ecuador. The study was conducted in the most populous city of Ecuador (15.7% of the total population of the country) and in four hospitals of the public health network which are reference centers for patients throughout Ecuador. It therefore provides the best approximation to the epidemiological situation of acromegaly in our country. In addition, it was possible to perform magnetic resonance imaging and the relevant biochemical measurements in all the participating hospitals, so ensuring the reliability of the data collected to confirm diagnosis.
The limitations and weakness of this study include the fact that not every private hospital and clinic of the city agreed to participate in it, which may have prevented the discovery of an additional number of cases. We estimate, however, that more than 90% of patients with acromegaly are seen at public hospitals, so that our coverage must have been almost complete.
It should also be noted that patient data records were incomplete in some cases, which was partly due to the lack of a good filing system at each hospital. Because of this, the mortality rate could not be ascertained due to difficulties in patient follow-up. In addition, immunohistochemical confirmation of the tumor was not available for all patients (there was no pathological report in some cases). Finally, comorbidities were not recorded in all cases. It is hoped that study extension and follow-up will allow us to fill these information gaps in our series.
Acromegaly is an underdiagnosed disease in Guayaquil. The incidence and prevalence found are low as compared to those reported in international series. We therefore assume that acromegaly is underdiagnosed and underreported in Ecuador. We think that a national registry system for patients diagnosed with acromegaly should be implemented in order to facilitate the design of adequate health care strategies for both its early diagnosis and for specialized treatment.
Conflicts of interestThere are no financial or personal conflicts of interest with other people or organizations that could have influenced the conduct of this study.
Please cite this article as: López Gavilanez E, Guerrero Franco K, Solórzano Zambrano N, Navarro Chávez M, López Estrella C, Vaca Burbano L, et al. Epidemiología de la acromegalia en Ecuador. Endocrinol Nutr. 2016;63:333–338.