Parenteral nutrition (PN) is an integral part of medical management of patients who do not have a functioning or accessible gastrointestinal tract. This paper discusses the clinical characteristics of patients receiving PN in a 420-bed hospital from 2009 to 2011. In addition, nutritional parameters were assessed at the start and end of PN and associated complications were analyzed.
Material and methodsRetrospective, observational study of PN episodes in adults conducted at the Nutrition Unit of Hospital Universitario de Guadalajara. Variables collected included epidemiological and clinical data, number and type of routes used, anthropometric data, analytical data, number of days on PN, reason for withdrawal, caloric provision, prevalence of phlebitis, metabolic complications (hypertriglyceridemia, abnormal liver function tests, hyperglycemia, and refeeding syndrome), and prevalence of bacteremia associated with central venous catheter (BAC).
ResultsThere were 312 episodes of PN. The immediate indication was postoperative ileus in 53.8% of the episodes. There was a statistically significant improvement in all analytical parameters assessed (albumin, prealbumin, retinol binding protein, transferrin, cholesterol, and lymphocytes). Caloric provision (kcal per kg) was 25.1±6.6. No metabolic complication occurred in 16.3% of the episodes, and hyperglycemia was the most common complication (79.8%). There were 10 cases of phlebitis (32.2%) and 30 episodes of BAC (8.7%). Bacteremia rate was 8.1 per 1000 days of PN.
DiscussionAlthough PN is an effective nutritional support technique, it is associated with complications of varying severity. Use of PN should therefore comply with the instructions accepted in the main clinical practice guidelines and requires careful monitoring by experienced professionals.
La nutrición parenteral (NP) es una parte integral del tratamiento médico de aquellos pacientes que no tienen un tracto gastrointestinal funcionante o accesible. En este trabajo se describen las características clínicas de los pacientes que han recibido NP en un hospital de 420 camas desde 2009 hasta 2011. Además, se evaluaron los parámetros nutricionales al inicio y fin de la NP, y se analizaron las complicaciones asociadas.
Material y métodosEstudio observacional retrospectivo de los episodios de NP en mayores de 18 años seguidos por la Unidad de Nutrición del Hospital Universitario de Guadalajara. Se recogieron: datos epidemiológicos y clínicos, número y tipo de vías empleadas, datos antropométricos, datos analíticos, número de días con NP, causa de la retirada, aporte calórico, prevalencia de flebitis, complicaciones metabólicas (hipertrigliceridemia, alteraciones en las pruebas de función hepática, hiperglucemia y síndrome de realimentación) y prevalencia de bacteriemia asociada a catéter venoso central (BAC).
ResultadosSe registraron 312 episodios de NP. La indicación inmediata fue íleo posquirúrgico en el 53,8% de los episodios. Se produjo una mejoría estadísticamente significativa de todos los parámetros analíticos que se evaluaron (albúmina, prealbúmina, proteína transportadora de retinol, transferrina, colesterol y linfocitos). El aporte calórico (Kcal por kg de peso) fue de 25,1±6,6. En el 16,3% de los episodios no se registró ninguna complicación metabólica y la hiperglucemia fue la complicación más frecuente (79,8%). Se registraron 10 casos de flebitis (32,2%) y 30 episodios de BAC (8,7%). La tasa de BAC fue de 8,1 casos por 1.000 días de utilización de catéter para NP.
DiscusiónAunque la NP es una técnica de soporte nutricional eficaz, se asocia a complicaciones de distinta gravedad. Por ello, su empleo debe ajustarse a las indicaciones aceptadas en las principales guías de práctica clínica y requiere de una monitorización exhaustiva por parte de profesionales expertos.
Hospital malnutrition is a highly prevalent public health problem which affects 30%-50% of patients of all ages admitted for medical and surgical reasons, and increases the longer the hospital stay.1–3 The PREDYCES study recently demonstrated, using the Nutritional Risk Screening Test (NRS-2002®), a 23.7% prevalence of hospital malnutrition in Spain, and also that the main factors associated with it were age (older than 70 years), female sex, oncological disease, associated diabetes mellitus and dysphagia, and the use of multiple drugs.4
In simple words, malnutrition may be defined as a clinical situation caused by nutrient deficiency due to either inadequate intake, increased losses, or increased requirements. There are however no simple parameters for defining malnutrition, and identification of at least two of the following clinical parameters is therefore recommended for its diagnosis5: inadequate energy intake, weight loss, muscle mass loss, loss of subcutaneous cell tissue, the occurrence of edema that may mask an associated weight loss, and function impairment measured by loss of handshake strength.
The causes of hospital malnutrition are multiple, including anorexia caused by the underlying condition, gastrointestinal symptoms, therapeutic procedures, drug treatments, and often a lack of interest by healthcare staff in assessing the nutritional status of admitted patients,6 despite the fact that hospital malnutrition is associated with increased morbidity and mortality, mean hospital stay, and healthcare costs.7
Parenteral nutrition (PN) consists of the direct administration of nutrients into the bloodstream. This nutritional support (NS) procedure was initially used in patients with gastrointestinal fistulas, but its use has gradually been extended to many indications such as short bowel syndrome, intestinal obstruction, abdominal surgery, inflammatory bowel disease, etc.,8 so that it is currently highly relevant in hospital care for many diseases and an integral part of medical treatment in patients who do not have a functional or accessible gastrointestinal tract, or in those in whom an adequate nutritional status cannot be maintained with natural and enteral nutrition.
This nutritional support modality requires multidisciplinary teams consisting of clinicians, pharmacists, and nurses to guarantee treatment success. It should not be forgotten that it is an artificial feeding technique that may induce many complications of varying severity (infectious, metabolic, thromboembolic and mechanical associated with central catheter insertion).9 An adequate selection of patients who will actually benefit from this type of NS is therefore required.
The purpose of this study was to evaluate the clinical characteristics of patients receiving NS with total or partial PN at Hospital Universitario de Guadalajara (420 beds) during 2009, 2010, and 2011, and to assess the change over time in nutritional parameters and to analyze the occurrence of associated metabolic and infectious complications.
Patients and methodsA retrospective, observational study of PN episodes in patients over 18 years of age fully monitored by the nutrition unit or partly monitored by this unit and other hospital departments (mainly subjects requiring at some time admission to the intensive care unit) of Hospital Universitario de Guadalajara during 2009–2011. Episodes not meeting the above criteria (which occurred in one patient younger than 18 years and in two other patients in whom NS was continued with home PN) were excluded from the study. In all cases, NS with PN started within 24h of its prescription. Energy requirements were calculated in all patients using the Harris-Benedict equation multiplied by Long correction factors. In patients with obesity, defined as a body mass index (BMI) ≥30kg/m2, adjusted weight was used instead of actual weight (ideal weight+0.25 [actual weight-ideal weight]). To calculate ideal weight, the following formula was used: men: 22×height2 (in meters); women: 21×height2 (in meters).
Patient data analyzed during monitoring by the nutrition unit included:
- 1.
Epidemiological and clinical data: age, sex, the requesting department, the underlying condition, and the immediate indication of NS with PN.
- 2.
The number and type of lines used.
- 3.
Anthropometric data: weight and BMI at the start and end of NS with PN. These data were collected for all episodes in the 24h prior or the 48h following the start and end of NS with PN. Patient weight was measured using a precision scale in all cases. Height was measured with the patients standing with their back leaning against the stadiometer of the same scale. In no cases were formulas used to estimate weight and height. BMI was calculated as weight (kg)/height (m) squared. In patients in whom these data could not be obtained, the weight and height reported by the patients themselves were used to calculate energy requirements.
- 4.
Laboratory data: albumin, prealbumin, retinol binding protein (RBP), transferrin, total cholesterol, and WBCs at the start and end of NS with PN were measured. Similarly to anthropometric parameters, these data were collected for all episodes in the 24h prior or the 48h following the start and end of NS with PN. During monitoring, however, these laboratory parameters were also measured weekly for the regular evaluation of patients on PN. Levels of triglycerides, alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (AP), gamma glutamyltransferase (GGT), and total bilirubin were also measured at least weekly, although the timing was modified based on patient condition and course.
- 5.
The number of days of NS with PN monitored by the nutrition unit: the number of PN episodes <5 days was also analyzed.
- 6.
The reason for PN withdrawal.
- 7.
Calorie provision: this was expressed as total kcal per day and as total kcal by kg of weight. Weight at the start of NS with PN was used to calculate calorie provision.
- 8.
The prevalence of phlebitis in patients receiving PN through a peripheral venous catheter (PVC): phlebitis was defined as the presence of induration or erythema with heat and pain at the entry site and sometimes visible in the course of the catheter.
- 9.
Metabolic complications: the nutrition unit controlled the occurrence of hypertriglyceridemia, abnormal liver function tests, hyperglycemia, and refeeding syndrome (RS) during monitoring.
Hypertriglyceridemia was defined as plasma triglyceride levels ≥250mg/dL after the start of NS with PN.
Abnormal liver function tests were defined as twofold elevations above the upper normal limit in at least two of the following parameters: ALT (0–53U/L), AST (10–40U/L), AP (25–180U/L), GGT (10–36U/L), or total bilirubin (0.1–1.2mg/dL after the start of NS with PN.
Hyperglycemia was defined as any capillary blood glucose level ≥140mg/dL after NS with PN was started in subjects without diabetes mellitus (DM) and ≥180mg/dL in those with DM. DM was defined as the documented presence of DM and/or treatment with insulin or oral antidiabetics before admission. To diagnose hyperglycemia, capillary blood glucose was measured every 6h in all patients receiving NS with PN.
RF was suspected in patients with severe hypophosphatemia, hypokalemia, hypomagnesemia, associated edema, and impaired carbohydrate metabolism after the start of NS with PN.
- 10.
The prevalence of catheter-associated bacteremia (CAB) in patients receiving PN through a venous central catheter (CVC) during monitoring by the nutrition unit. CAB was defined as follows10:
- –
After catheter removal: the isolation of the same microorganism in a blood culture taken from a peripheral vein and in a quantitative or semiquantitative culture of a catheter segment in a patient with symptoms of bacteremia and no other apparent infection site.
- –
Without catheter removal: a septic episode with no other apparent site in which the same microorganism was isolated in quantitative simultaneous cultures with a 5:1 or higher ratio between samples taken through the catheter and those obtained by vein puncture.
- –
The CAB rate was calculated as the number of episodes per 1000/total days of catheter use for PN.
This study did not collect other types of complications associated with the use of CVC such as thrombosis, pneumothorax, accidental loss, or malposition.
Statistical analysisData were statistically analyzed using software SPSS 15.0 for Windows. Quantitative variables were given as mean±standard deviation, and qualitative variables as percentages. A Student's t test for paired samples and a Student's t test for independent samples were used to compare quantitative variables. An ANOVA test was used to compare multiple variables between the groups of patients with and without CAB. A value of p<0.05 was considered statistically significant.
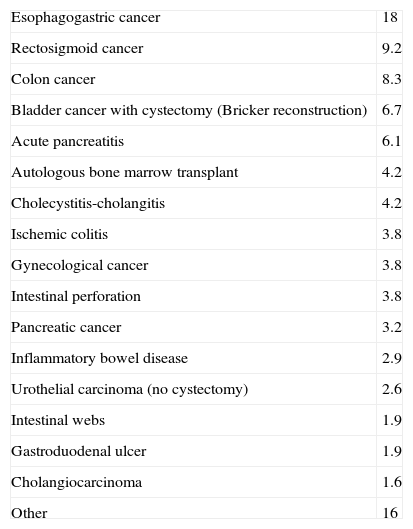
ResultsA total of 312 episodes were analyzed, 133 in 2009 (42.6%), 114 in 2010 (36.5%), and 65 in 2011 (20.8%). Mean age was 66.3±16.2 years, and 60.6% of patients were male. The underlying diseases in patients who required NS with PN were gastrointestinal tumors in 41.6% of episodes (proximal 23.7%; distal 17.9%), non-oncological abdominal disease in 36.9%, non-gastrointestinal oncological disease in 18.6%, and other conditions in 2.9% (Table 1). The acute indication leading to NS with PN was postoperative ileus in 53.8% of episodes, intestinal obstruction in 14.1%, non-surgical ileus in 12.5%, intestinal fistula in 4.8%, severe mucositis or intolerance of enteral nutrition (EN) in 3.8%, gastrointestinal bleeding (upper and lower) in 2.8%, and other indications in 8.2%. The requesting departments were general surgery in 58% of episodes, gastroenterology in 9.9%, urology in 9.1%, internal medicine in 5.1%, oncology in 4.8%, hematology in 4.2%, and other departments in 8.9% of cases.
Specific underlying disease (%) of patients requiring NS with PN during 2009–2011 at Hospital Universitario de Guadalajara.
| Esophagogastric cancer | 18 |
| Rectosigmoid cancer | 9.2 |
| Colon cancer | 8.3 |
| Bladder cancer with cystectomy (Bricker reconstruction) | 6.7 |
| Acute pancreatitis | 6.1 |
| Autologous bone marrow transplant | 4.2 |
| Cholecystitis-cholangitis | 4.2 |
| Ischemic colitis | 3.8 |
| Gynecological cancer | 3.8 |
| Intestinal perforation | 3.8 |
| Pancreatic cancer | 3.2 |
| Inflammatory bowel disease | 2.9 |
| Urothelial carcinoma (no cystectomy) | 2.6 |
| Intestinal webs | 1.9 |
| Gastroduodenal ulcer | 1.9 |
| Cholangiocarcinoma | 1.6 |
| Other | 16 |
A total of 376 lines were required. More than one line was required for PN administration in 55 episodes (17.6%). CVCs were used in 91.7% of patients (jugular 41.4%, subclavian 39.7%; Port-a-cath 4.3%, Hickman 3.7%, peripherally inserted CVC [PICC] 2.1%, and femoral 0.5%). PVCs were used in 8.2%.
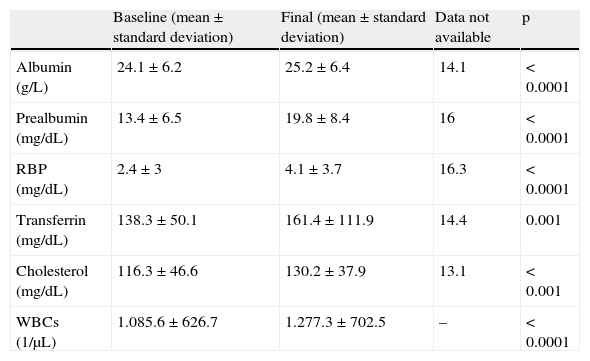
Baseline and final weights (kg) were, respectively, 67.8±14.7 vs 67.6±13. On the other hand, baseline and final BMI values (kg/m2) were, respectively, 25.9±5.3 vs 25.8±5.4. For both parameters, data were missing in 35.6% of episodes and no statistically significant differences were found. Table 2 compares the values of the main nutritional parameters at the start and end of NS with PN.
Change over time in laboratory test results (mean±standard deviation) in patients requiring NS with PN during 2009–2011 at Hospital Universitario de Guadalajara.
| Baseline (mean±standard deviation) | Final (mean±standard deviation) | Data not available | p | |
| Albumin (g/L) | 24.1±6.2 | 25.2±6.4 | 14.1 | <0.0001 |
| Prealbumin (mg/dL) | 13.4±6.5 | 19.8±8.4 | 16 | <0.0001 |
| RBP (mg/dL) | 2.4±3 | 4.1±3.7 | 16.3 | <0.0001 |
| Transferrin (mg/dL) | 138.3±50.1 | 161.4±111.9 | 14.4 | 0.001 |
| Cholesterol (mg/dL) | 116.3±46.6 | 130.2±37.9 | 13.1 | <0.001 |
| WBCs (1/μL) | 1.085.6±626.7 | 1.277.3±702.5 | – | <0.0001 |
RBP: retinol binding protein.
The number of days of NS with PN was 11.9±12.1, and total days of NS were 3711. NS duration was longer than five days in 86.2% of episodes. The reason for the withdrawal of NS with PN was intolerance to either oral administration, occurring in 79.1% of episodes, or to EN, in 8%. Other more uncommon reasons for NS withdrawal were the discontinuation of therapeutic measures in 7.4% of episodes, death in 4.5%, and transfer to other centers in 1% of episodes.
Calorie provision was 1652±213l1 total kcal daily and 25.1±6.6 total kcal by kg of weight.
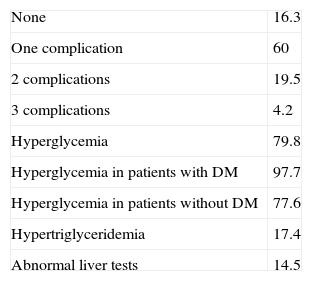
As regards metabolic complications (Table 3), none occurred in 16.3% of episodes. The most common complication was hyperglycemia, which was found in 79.8% of episodes. 19.6% of patients had DM, and 97.7% of them experienced hyperglycemia. Among patients without DM (80.4%), 77.6% also experienced hyperglycemia during NS with PN. Calorie provision in episodes where no hyperglycemia occurred was 26.8±7.1kcal/kg, as compared to 24.9±6.5kcal/kg in those where this complication occurred (with and without associated DM) (p>0.05). Hypertriglyceridemia occurred in 17.4% of episodes, while abnormal liver tests were less common and were found in 14.5% of cases. Calorie provision in episodes where hypertriglyceridemia did not occur was 25±6.5kcal/kg, as compared to 25.5±7.2kcal/kg in those where this complication occurred (p>0.05). Finally, calorie provision in episodes where abnormal liver function tests were found was 25±6.4kcal/kg, as compared to 25.9±8.1kcal/kg in those where this complication occurred (p>0.05). RS was not suspected in any episode. More than one associated complication was recorded in 23.7% of episodes.
Metabolic complications (%) of patients requiring NS with PN during 2009–2011 at Hospital Universitario de Guadalajara.
| None | 16.3 |
| One complication | 60 |
| 2 complications | 19.5 |
| 3 complications | 4.2 |
| Hyperglycemia | 79.8 |
| Hyperglycemia in patients with DM | 97.7 |
| Hyperglycemia in patients without DM | 77.6 |
| Hypertriglyceridemia | 17.4 |
| Abnormal liver tests | 14.5 |
As regards infectious complications, phlebitis occurred in 10 of the episodes (32.2%) in which a PVC was used. 21 (6.1%) caused by Gram-positive germs, 8 (2.3%) by yeasts (Candida spp.), and one (0.3%) due to Gram-negative germs (Pseudomonas aeruginosa). The Gram-positive germs involved were Staphylococcus epidermidis (3.5%), Staphylococcus hominis (0.9%), Enterococcus faecalis (0.9%), Enterococcus faecium (0.6%), and Staphylococcus aureus (0.3%). The CAB rate was 8.1 cases per 1000 days of catheter use for PN. Statistically, the number of days of NS with PN was the only factor associated with CAB increase (days of PN in episodes without CAB 11.3±11.5 vs days of PN in episodes with CAB, 17.3±15.7; p=0.009). No statistically significant relationship was seen with type of CVC, baseline nutritional parameters, the underlying disease, the occurrence of hyperglycemia, calorie provision, or the hospital department to which the patients were admitted. CAB episodes were related to the use of subclavian (4.9%), jugular (3.2%), Port-a-cath (0.3%), and Hickman (0.3%) lines.
DiscussionHospital clinical nutrition is a relatively young medical discipline responsible for integral care related to the prevention of malnutrition and NS to malnourished patients. The nutrition unit of Hospital Universitario de Guadalajara was created in 2006, and has since then been able to monitor most adult patients requiring NS with PN during hospital admission (except for those admitted to the intensive care unit). It should be noted that episodes of NP have decreased during the three years of data collection. This was probably due to EN development with the advent of new formulas and routes, which has promoted its use in conditions traditionally managed with gastrointestinal rest and PN.
The general indication of PN is the impossibility of administering nutrients by the oral or enteral routes for longer than 7–10 days in patients with no evidence of malnutrition, or for 5–7 days if the patient is malnourished. Thus, PN is indicated when feeding by the gastrointestinal route is not possible, rather than because of the presence of associated malnutrition. The American Society for Parenteral and Enteral Nutrition (ASPEN) clinical practice guidelines11 propose indications for PN in many diseases. In our series, oncological disease in the proximal gastrointestinal tract (esophagogastroduodenal) was the most common reason for both preoperative and postoperative PN.
One of the essential objectives of PN is to adapt the calorie requirements of patients to their actual needs at each moment. An adequate estimation of the energy needs of patients is therefore extremely important. Indirect calorimetry and the use of labeled isotopes are the most accurate methods,12 but were not used in our case due to the unavailability of both the method and trained staff. The Harris-Benedict equation, multiplied by Long correction factors, was used in the study because it is a widely used procedure in standard clinical practice, while bearing in mind that it is not completely accurate and may overestimate the calorie needs of patients.
In our study, statistically significant improvements occurred in all the laboratory parameters assessed (Table 2). The high proportion of missing data, greater than 15% for prealbumin and RBP levels, is noteworthy. The reason for this is that in patients where NS with PN was withdrawn due to the discontinuation of therapeutic measures, transfer to other hospital, or patient death, these parameters were not tested at the end of NS.
As regards associated metabolic complications, hyperglycemia was most common, as mentioned above (79.8%). In the studies reviewed,13,14 its incidence was highly variable, ranging from 26.7% to 79.7% depending on the capillary glucose level from which hyperglycemia was defined. Like hypertriglyceridemia and abnormal liver function tests, hyperglycemia is a complication related to calorie provision and the composition of PN. This latter parameter was not analyzed in our series, which is therefore a study limitation. It should be noted, however, that hyperglycemia is also related to other factors such as the prior impairment in carbohydrate metabolism, the underlying disease, and the degree of metabolic stress. In addition, the use of other concomitant drugs such as glucocorticoids, thiazide and loop diuretics, anticonvulsants, beta-2 adrenergic agonists, and xanthine-derived bronchodilators is associated with the occurrence of hyperglycemia.15 On the other hand, the insulin requirements and treatment schemes used (insulin subcutaneous administration, intravenous administration in PN, or the use of a continuous infusion) were also not analyzed in our series.
Hypertriglyceridemia is another complication related to NS with PN whose incidence ranges from 6% to 38% depending on the study.16,17 In our series, hypertriglyceridemia was found in 17.4% of the episodes. In subjects receiving PN, hypertriglyceridemia is due to impaired plasma clearance of lipids due to either decreased lipoprotein lipase activity or excess provision.18 Renal failure, sepsis, pancreatitis, and glucocorticoid administration are associated risk factors.19 As regards liver involvement associated with PN, changes in liver function tests have been reported in 20–90% of patients receiving this type of NS.20,21 In our series, abnormal liver function test results were found in 14.5% of patients receiving PN (its incidence was probably lower because of the definition used, which required increases in at least two parameters). There is therefore a great variability depending on the definition used, although it would appear to be clear that liver involvement is more common in children than in adults and also increases with long-term NS with PN. In the first weeks of using PN, the markers of cholestasis which increase first are GGT and AP, which also appear to be the most specific in adult patients.22 This elevation usually occurs at the start of the second week, while transaminases increase later. The chance of liver function impairment is higher if associated sepsis and malnutrition exist,23 and also in certain clinical conditions, such as inflammatory bowel disease.24
On the other hand, the most severe complication related to NS with PN is CAB, which has a substantial impact on morbidity and mortality (attributable mortality, 20–35%), hospital stay prolongation, and healthcare costs.25,26 Because of its importance, a protocol for CVC management in patients on PN which involved healthcare staff was implemented in 2009 in Hospital Universitario de Guadalajara and is currently under review.
CAB incidence reported in the literature ranges from 2.9 to 11.3 cases per 1000 days of CVC use,27 but it should be noted that PN markedly increases this risk.28,29 In studies conducted in other Spanish hospitals, the CAB rate was 25 cases per 1000 days of catheter use for PN30 and 13.1 cases per 1000 days of CVC use.31 In a study conducted in seriously ill patients admitted to intensive care units,32 the CAB rate was 0.44 cases per 100 days of CVC use. In our series, the CAB rate was 8.1 cases per 1000 days of CVC use for PN. The rate would probably have been lower if the data had been analyzed based on the total number of days of CVC use, as is done in many studies, rather than being based on the total number of days of NS with PN, as was done in our study. As in other series, Gram-positive germs were the main causative agents of CAB,33,34 although our study found a predominance of CAB induced by Candida spp. over Gram-negative germs. This may be explained by the fact that the use of PN is a risk factor for the development of candidemia.35 As in other reviewed articles,36,37 the risk of infection increased with the number of days of NS with PN, although our study did not find a statistically significant relationship with the type of CVC used, unlike in other series where a greater infection risk was seen with the femoral and jugular lines.
To sum up, PN is associated with complications of varying severity. The use of PN should therefore be adjusted to the indications accepted in the main clinical practice guidelines and requires regular assessment of patients by staff trained to minimize such complications as much as possible.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Herranz Antolín S, et al.. Soporte nutricional con nutrición parenteral. Evolución y complicaciones asociadas. Endocrinol Nutr. 2013;60:287–93.