Dropout is a highly prevalent and serious problem in assessing the effectiveness of weight loss studies and a major cause of treatment failure in the management of morbidly obese patients.
ObjectivesTo determine which tests used for the psychometric evaluation of morbidly obese patients are more predictive of success/dropout in a weight loss program.
MethodsSixty patients aged 18–65 attending the Outpatient Obesity Clinic between 2009 and 2011, were recruited for an intensive life style weight loss program. We compared the results obtained in Hamilton Depression scale, Hamilton Anxiety scale, Golombok Rust Inventory of Sexual Satisfaction, Eating Disorders Inventory-2, SF-36 Health Survey and Plutchik's Impulsivity questionnaire between patients who completed the intervention with those obtained in patients who did not complete it.
ResultsThe rate of decline in the patients attending our program was 41.6% in the first year. Our results suggest that the Plutchik Impulsivity questionnaire, could be used as a predictive tool for success/attrition in intensive life style weight loss program.
ConclusionsOur results suggest that the Plutchik Impulsivity questionnaire, could be used as a predictive tool for success/attrition in intensive life style weight loss program. The screening of patients prior to inclusion in these programs should help to optimize its efficacy and efficiency.
Los abandonos son un problema muy frecuente y serio cuando se valora la eficacia de los estudios sobre la pérdida de peso y una causa importante de fracaso del tratamiento en los pacientes con obesidad mórbida.
ObjetivosDeterminar qué pruebas empleadas en la evaluación psicométrica de obesos mórbidos predicen mejor el éxito o el abandono de un programa de pérdida de peso. Métodos Se reclutó a 60 pacientes de 18–65 años de edad que acudían a la consulta externa de obesidad entre 2009 y 2011 para un programa intensivo de pérdida de peso basado en el modo de vida. Se compararon los resultados obtenidos en la escala de depresión de Hamilton, la escala de ansiedad de Hamilton, el Golombok Rust Inventory of Sexual Satisfaction, el Eating Disorders Inventory-2, la encuesta de salud SF-36 y el Plutchik's Impulsivity Questionnaire de los pacientes que completaron y no completaron la intervención.
ResultadosLa tasa de descenso en los pacientes que acudían a nuestro programa fue del 41,6% en el primer año. Nuestros resultados sugieren que el Plutchik Impulsivity Questionnaire podría ser una herramienta útil para identificar a los sujetos predispuestos a abandonar el programa.
ConclusionesNuestros resultados indican que el Plutchik Impulsivity Questionnaire puede utilizarse como herramienta pronóstica del éxito o deserción de un programa intensivo de pérdida de peso basado en el modo de vida. La selección de los pacientes antes de su inclusión en estos programas debe ayudar a optimizar su eficacia y eficiencia.
Dropout is a highly prevalent and serious problem in assessing the effectiveness of weight loss studies and a major cause of failure in the management of morbidly obese patients. The rate of dropout in supervised weight loss programs and/or clinical trials is between 10 and 80%,1 underlying the need for new strategies to improve the retention and outcomes of long-term non-surgical interventions.2,3
In order to provide new data to the limited set of existing scientific literature on this area, we analyzed psychometric and quality of life questionnaires (that are part of the battery of tests we use in an intensive life style weight loss program) with the main objective to find out, if any of these tests could be predictive of success/dropout in our group therapy.
MethodsThis study was conducted at the Research Unit of University Hospital of Son Espases, Palma de Mallorca, Spain.
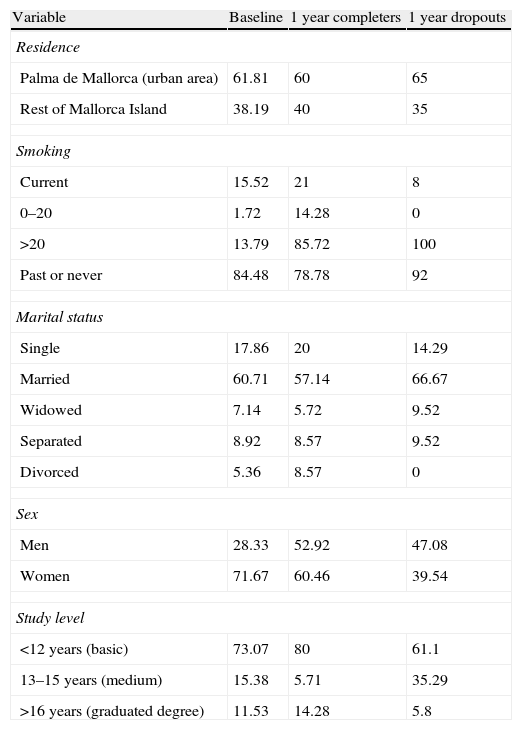
SubjectsThe present study was designed as a prospective survey, carried out on subjects attending our Obesity Outpatient Clinic between 2009 and 2011. Sixty patients aged 18–65 were recruited for a weight loss education program, including weekly and biweekly group sessions. Exclusion criteria included: pregnancy, endocrinal diseases or cancer (which might induce weight variation), severe mental illness and inclusion in bariatric surgery waiting list. All these patients underwent a physical examination during the first clinical visit. Educational attainment was measured in years of schooling: <12 years (basic), 13–15 years (medium) or >16 years (graduate degree) (Table 1). Marital status was reported as single, married, separated, divorced or widowed. Cigarette smoking was defined as current, past or never. Current smokers were defined as participants, who reported smoking >1 cigarette/s for at least the past year, they were asked for the number of cigarettes per day: 0–20 or >20.
Baseline characteristics: total population and completers vs. dropouts in 1 year. Data showed in %.
| Variable | Baseline | 1 year completers | 1 year dropouts |
| Residence | |||
| Palma de Mallorca (urban area) | 61.81 | 60 | 65 |
| Rest of Mallorca Island | 38.19 | 40 | 35 |
| Smoking | |||
| Current | 15.52 | 21 | 8 |
| 0–20 | 1.72 | 14.28 | 0 |
| >20 | 13.79 | 85.72 | 100 |
| Past or never | 84.48 | 78.78 | 92 |
| Marital status | |||
| Single | 17.86 | 20 | 14.29 |
| Married | 60.71 | 57.14 | 66.67 |
| Widowed | 7.14 | 5.72 | 9.52 |
| Separated | 8.92 | 8.57 | 9.52 |
| Divorced | 5.36 | 8.57 | 0 |
| Sex | |||
| Men | 28.33 | 52.92 | 47.08 |
| Women | 71.67 | 60.46 | 39.54 |
| Study level | |||
| <12 years (basic) | 73.07 | 80 | 61.1 |
| 13–15 years (medium) | 15.38 | 5.71 | 35.29 |
| >16 years (graduated degree) | 11.53 | 14.28 | 5.8 |
Height and weight were measured with the subjects barefooted and lightly dressed, with a Tanita's WB-3000 digital beam scale with a mechanical height rod, allowing patients’ height to be taken at the same time as weight during the first visit. Height was taken at head level to the nearest centimeter, with feet joined together and following the plane of Frankfurt. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. Circumferences were measured to the nearest centimeter by using a flexible tape with the subject standing. The abdominal circumferences (waist) were measured at the end of expiration by wrapping the tape at the level of the umbilicus. Weight was measured weekly for the first three months and biweekly for 21 months.
Dietary assessmentThe study was focused on the qualitative aspects of the dietary habits, as the distribution of energy intake, frequency of consumption and food choices. We provided information on the benefits of Mediterranean Diet and encouraged our patients to follow this diet. We encouraged our patients to eat five meals per day and there were no restrictions in calorie intake. Dietary lectures were provided by a Registered Nurse, a Specialist in Nutrition (MSc). This approach provided a good opportunity to review dietary preferences and patient's dietary habits.
Physical activityIn order to develop a personalized physical activity program, a physician (sport medicine specialist), assessed these morbidly obese adults, at baseline and there-after every 3 months. The initial goal was to determine their physical condition and identify any potential anatomic limitations, which these patients may suffer. In subsequent visits the physician with the support of a physical therapist, developed a personalized specific physical activity program for each patient, taking into account their general health status, physical condition and physical activity preferences. The goal was to slowly initiate these patients into a more active life style.
Psychometric and quality of life testsWe analyzed the following battery of psychometric and quality of life tests: Hamilton Depression scale.4,5 Hamilton Anxiety scale.6 Golombok Rust Inventory of Sexual Satisfaction.7,8 Eating Disorders Inventory-29 (EDI-2). SF-36 Health Survey10 and Plutchik's Impulsivity Questionnaire.11
Data analysisWe took advantage of data mining12 analysis to process the large set of data obtained through the different questionnaires mentioned above, in an effort to identify specific answering patterns which could potentially be helpful to more accurate predict which patients would dropout from this type of life style interventions. We carried out an analysis of the data to extract adequate models and patterns by using WEKA data mining software. We established a Classification by J48 Graph functionality (creating decision and predictive training tree models). J48 is an open source java implementation of the C4.5 algorithm,13 which builds decision trees from a set of data, by using the concept of information entropy.
The same process was used to analyze each test provided to patients. We selected two kinds of tests: dimensional tests (e.g. Sf-36) and test with atomic testing questions (e.g. Plutchik). We also selected questions/dimensions of different test where differences seen were more than 10 percentage points on an average, between the answers of completers vs. dropouts. These questions/dimensions were analyzed together by using the WEKA software. The tests that provided dimensional results were used to perform principal components (dimensions) analysis by using the R-project software and the package Data Analysis functions to analyze Ecological and Environmental data in the framework of Euclidean Exploratory methods (ade4)14–17 for multivariate descriptive statistical analysis. To assess whether the rate of weight loss is different between each group we used ANCOVA analysis.
ResultsWe included 60 patients (43 women), 61.81% lived in Palma, 15.52% were smokers and 60.71% were married. Educational attainment was measured in years of schooling: <12 years (basic), 13-15 years (medium) or >16 years (graduate degree). Most of them (the large majority) had basic studies (Table 1). Table 2 shows the anthropometric baseline data of all the patients included in the life style intervention weight loss program.
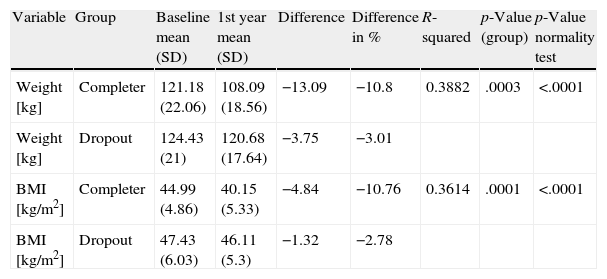
Changes in weight and BMI: completers vs. dropout after 1 year of intervention.
| Variable | Group | Baseline mean (SD) | 1st year mean (SD) | Difference | Difference in % | R-squared | p-Value (group) | p-Value normality test |
| Weight [kg] | Completer | 121.18 (22.06) | 108.09 (18.56) | −13.09 | −10.8 | 0.3882 | .0003 | <.0001 |
| Weight [kg] | Dropout | 124.43 (21) | 120.68 (17.64) | −3.75 | −3.01 | |||
| BMI [kg/m2] | Completer | 44.99 (4.86) | 40.15 (5.33) | −4.84 | −10.76 | 0.3614 | .0001 | <.0001 |
| BMI [kg/m2] | Dropout | 47.43 (6.03) | 46.11 (5.3) | −1.32 | −2.78 |
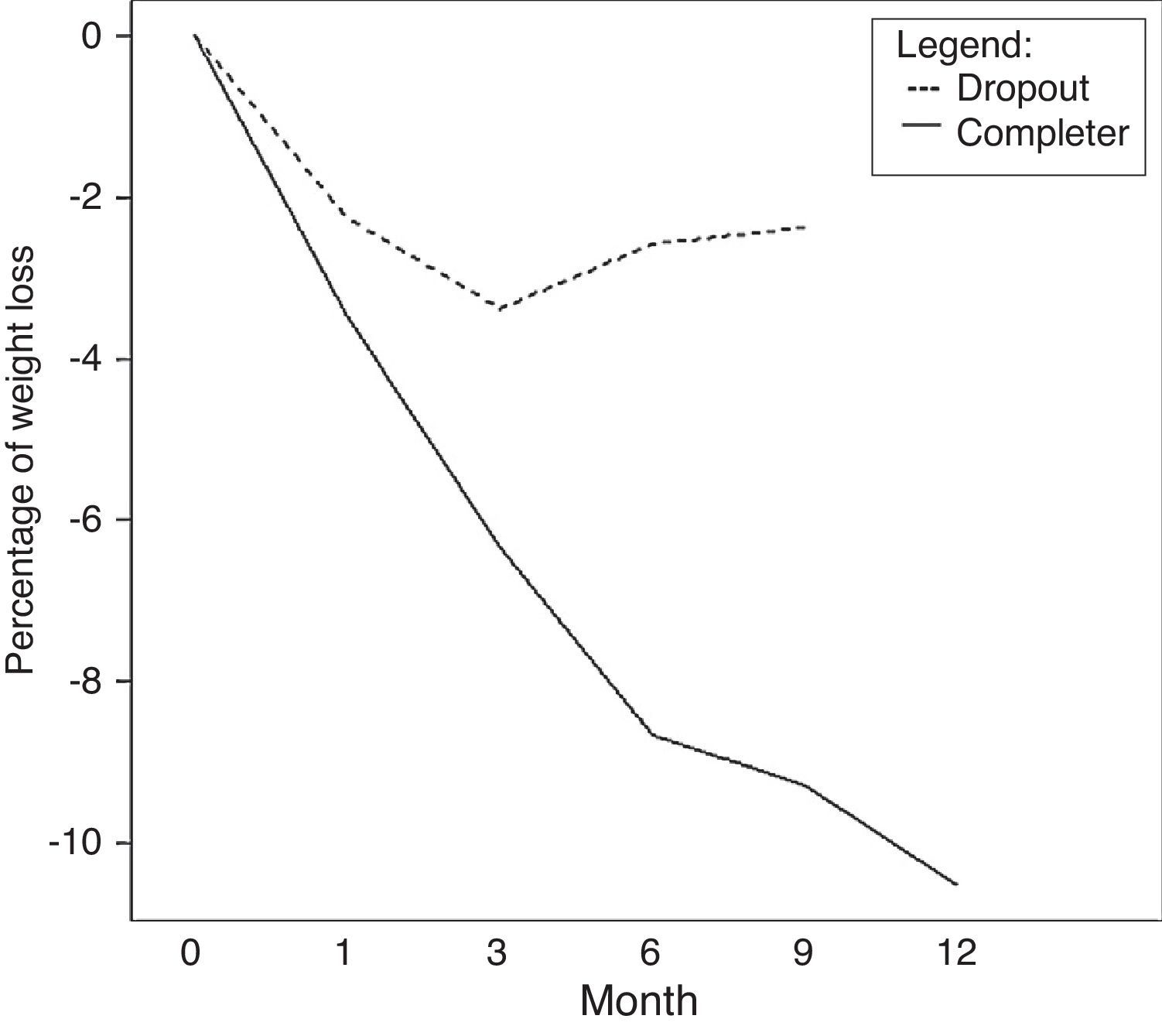
A significant BMI reduction was noticed in the completers at 12th month (p=.0001) (R2=0.3614) vs. dropouts. The completer patients at 12 month had lost 13.09kg of mean (10.8%) (Fig. 1) of their original body weight, in comparison with the dropout patients (Table 2), who just lost 3.75kg (3.01%) (p=.0003) (R2=0.3882). We did not notice any significant (p=.11) change in the waist circumference between both groups.
The rate of decline in the patients attending our intensive interdisciplinary weight loss program was 41.6% in the first year. In a subgroup (n=13) of extreme obese patients with BMI>50kg/m2, we found that the dropout rate was significantly higher (61.5%) than in the patients with BMI>40–50kg/m2 (31.9%) population (n=47) at 12th month. Of importance is that, 40% of these morbidly obese patients who completed one year of therapy, had dropped one level in the degree of obesity (independently of their initial BMI), from BMI>50kg/m2 improved to BMI 40–50kg/m2 and from class III improved their weight to become class II obesity.
Forty-two patients completed the Plutchik's questionnaire at baseline. In fact, 14 patients were dropout in one year and 28 continued the study. The algorithm J48Graph rated: 12 (A.a1+C.c1) patients dropped out in one year and 30 (B.b1+D.d1) continued the study (the training prediction tree model by artificial intelligence), therefore:
- •
10 dropouts were correctly predicted (DROPOUT/DROPOUT) ((A.a1−A.a2)+(C.c1−C.c2)).
- •
Dropouts were misclassified as completers (COMPLETER/DROPOUT) ((D.d2)).
- •
26 completers were correctly predicted as completers (COMPLETER/COMPLETER) (B.b1+(D.d1-D.d2)).
- •
2 completers were misclassified as dropouts (DROPOUT/COMPLETER) (A.a2+C.c2).
In particular in Plutchik's questionnaire results show that:
Branch E, <= 0 score for Q7. Twenty-seven patients classified by J48Graph (Leaf B.b1+Leaf D.(d1−d2)+ Leaf C.c2) out of 28 real completers (96.43%) answered “never” to question 7: “Is it difficult for you to control sexual impulses?”, were completers of our therapy one year later. Eight patients classified by J48Graph (Leaf C.(c1−c2)+Leaf.D.d2) who answered “never” (score=0), were dropout in one year of 14 (real dropouts patients, 57.1%). That question is essential for predicting NO dropout in the training prediction tree.
Branch A, > 0 score for Q7. Six patients classified by J48Graph (Leaf A.(a1−a2)) of 14 (real dropouts patients, 42.85%) answered different of “never” (score≠0) to question 7: “Is it difficult for you to control sexual impulses?”, were dropout of our therapy a year later.
Branch B, > 1 score for Q5. Ten patients classified by J48Graph (Leaf B.(b1)) of 28 (real completers patients, 35.71%) answered always (score=3) or almost always (score=2) to question 5: “Often loses patience?”, were completers of our therapy one year later (previously having answered in Q7 “never”). J48Graph was no misclassification.
Branch C, >1 score for Q10. Four patients classified by J48Graph (Leaf C.(c1−c2)) of 14 (real dropouts patients, 28.57%) answered always (score=3) or almost always (score=2) to question 10: “Are you impulsive?”, were dropouts of our therapy one year later (previously having answered in Q7 “never” and Q5 “never” (value=0) or sometimes (value=1)).
Branch D, <= 0 score for Q10. Sixteen patients classified by J48Graph (Leaf D.(d1−d2)) of 28 (real completers patients, 57.1%) answered “never” (value=0) or sometimes (value=1) to question 10: “Are you impulsive?”, were completers of our therapy one year later (previously having answered in Q7 “never” and Q5 “never” (value=0) or sometimes (value=1)).
In the correlation matrix performed our data did not show any correlations between age, sex, marital status gender and study level with dropout. In our study the patients who showed a higher dropout rate had medium study level (13–15 years), followed by patients who had basic study level (<12 years).
As a final result of this detailed review of the analysis realized, we noted that in question 7 of the Plutchik test, depending on the patient's response, the analysis classifies it as predisposed to drop out of the program.
DiscussionOur data show that the rate of dropout in the patients attending an intensive life style intervention weight loss program was 41.6% in the first year. This elevated number of patients who did not complete the weight loss program, is in agreement with previous studies in the literature and, it is a major limiting factor for the ultimate success of these weight loss interventions.18 We used data mining analysis to develop an evaluation system of different health status, depression, sexual satisfaction and anxiety questionnaires that could be a useful analytic tool to predict the likelihood of dropout in these intervention weight loss program. This analysis consisted of the establishment of decision trees, taking into account the answers reported by the patients to the different items of these questionnaires. Fabricatore et al.19 have performed a multivariate analysis of these baseline parameters with other predictors (the early weight loss, attendance to scheduled visits and completion of feeding reports during the first three weeks of treatment) trying to predict the success in the different weight loss therapies (medication, life style modification and combined therapy). They concluded that the earlier success in weight loss, had a bigger predictive power over the rest earlier variables of process discussed, however their conclusions were not inferable to different interventions and/or different contexts (e.g. commercial programs). They also underlined the need of further research, emphasizing in those individual factors related with recruitment (inclusion criteria), duration of these therapies and the design of intervention (face to face/remote).
Our data suggested that an early success in weight loss could be a good predictor of success in patients following life style weight loss therapies (Fig. 1).
Depending on this parameter, patients could be classified in different group levels of therapy, with the aim of minimizing the perception of failure and feelings of inadequacy or low self-esteem. This indication is reinforced by our finding regarding the subpopulation of class III obese patients (BMI>50kg/m2) that probably should be carefully screened before inclusion in this type of therapy, and distributed in specific groups, in an effort to minimize stigma and to promote the development of specific strategies for these patients.
Earlier studies20 have shown that disinhibition is predictive of poorer success at weight loss, and of weight regain after weight loss regimes. This characteristic is associated with lower self-esteem, low physical activity and poor psychological health. This data would be consistent with our findings about the influence of impulsivity on attrition.
Previous attrition research examining reasons for dropout (comparing differences between program completers and not completers) has provided scientific evidence, regarding the influence of demographic factors, specifically age.21 Interestingly, younger patients tend to be more likely to prematurely end treatment,21 however gender and ethnicity were not consistently associated with the rate of attrition in weight loss programs.18–21
Other psychosocial factors such as high level of stress, presence of depressive symptoms and high expectations of success in addressing these therapies for weight loss,21,22 have been associated with higher level of attrition.
ConclusionThe review of the outcomes of the analysis of our population suggests that the profile of the patient with higher chance of dropout, corresponds to a person of any age, married, less than 15 years of school attendance, poor management of impulses, with little initial success losing weight and who is unable to lose weight after six months of intervention.
Our results suggest that the Plutchik Impulsivity questionnaire, could be used as a predictive tool for success/attrition in intensive life style weight loss program.
In summary, the possibility of having a decision tool with enough predictive power to detect the risk of dropout would give us the option of an early intervention, as well as to better select patients to include in these weight loss programs. We should carry out bootstrapping and use the out-of-bag observations to evaluate the predictive accuracy in larger populations.
Further studies to design strategies to reduce dropout in weight loss interventions are urgently needed.
FundingThis study has been sponsorized by Fundación Mutua Madrileña.
We thank Biobanco HUSE (code RD09/076/054) for its contribution to the project with the processing and storage of the biological samples.
Conflict of interestNone declared.
Please cite this article as: Tur JJ, Escudero AJ, Romaguera D, Burguera B. ¿Cómo podemos predecir qué pacientes con obesidad mórbida se adherirán a programas de pérdida de peso basados en cambios en el estilo de vida? Endocrinol Nutr. 2012;60:297–302.