Iodine deficiency is a factor that may compromise child development, but is not the only one. Other health determinants, some of them outside the healthcare system, are able to influence development. Fighting iodine deficiency may be a pragmatic and useful strategy if it is found to be not maleficent, beneficial to health, and cost-effective, and does not make us lose the notion that child development goes beyond psychomotor or cognitive performance. This article analyzes such constraints from a critical point of view.
El déficit de yodo es un factor que puede comprometer el desarrollo del niño. Pero no es el único. Otros determinantes, algunos de ellos ajenos al sistema sanitario, tienen capacidad para influir en el desarrollo del niño. Luchar contra la deficiencia de yodo podría ser una estrategia pragmática y útil si resultara ser no maleficente, beneficiosa en términos de salud, coste-eficiente y no nos hiciera perder la noción de que el desarrollo del niño va más allá del desempeño psicomotor o cognitivo. En el presente artículo se analizarán desde el punto de vista crítico si dichos condicionantes se dan en la actualidad.
It is indisputable that all children should have the right to enjoy living conditions that promote their development.1 Since iodine deficiency during pregnancy limits cognitive and psychomotor maturation, some researchers and experts have stated that iodine supplementation through the pregnant mother is an essential right of children to “ensure optimal development”.2
However, we may wonder if cognitive development is the only determinant for the future of children and if it may be dissociated from their physical, moral, spiritual, or social development to which they are also entitled according to the Convention on the Rights of the Child. These different aspects cannot be separated.
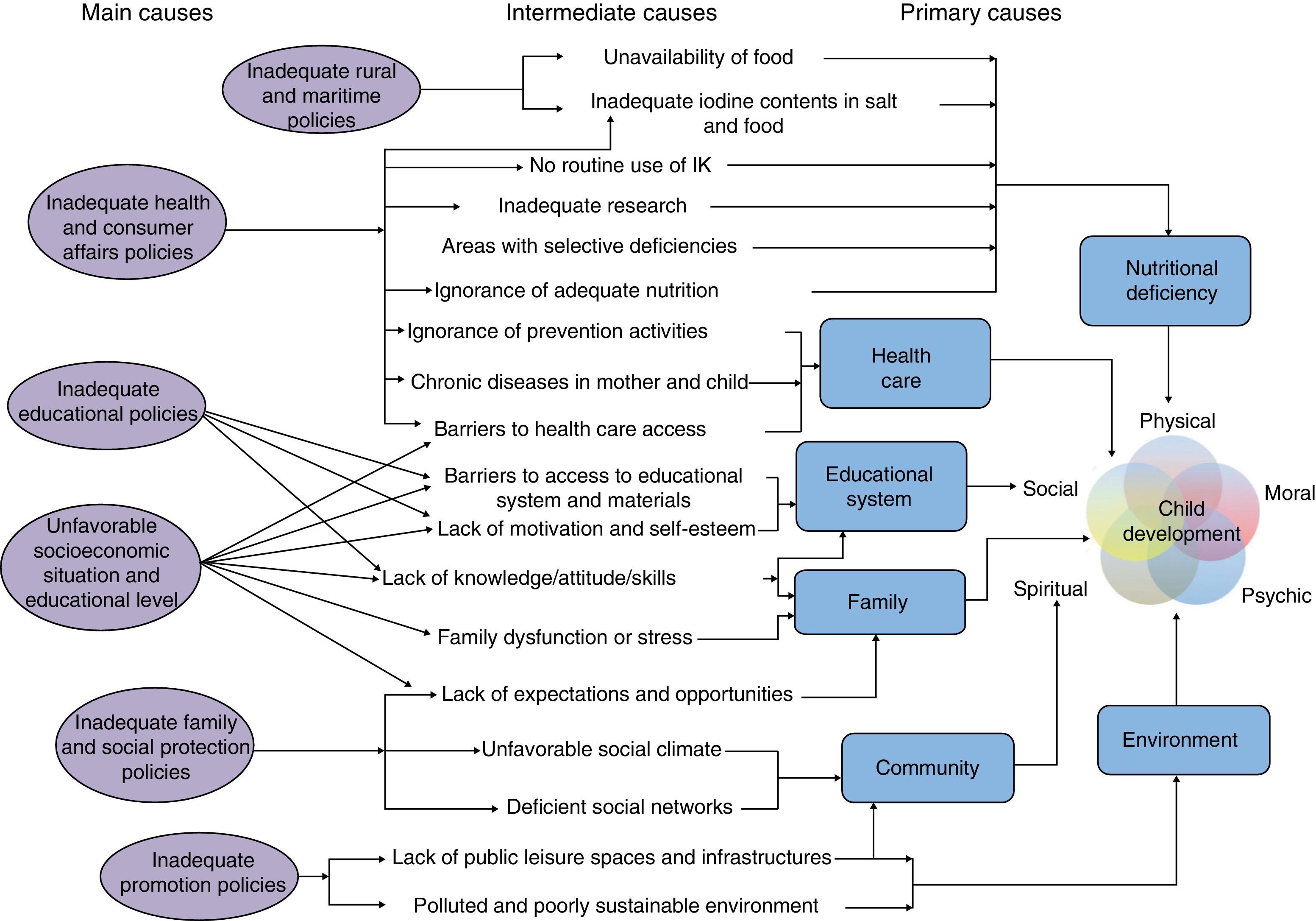
There are many factors which influence overall child development3–6 (Fig. 1). Adequate nutrition is undoubtedly essential, but is not the only component. Adequate educational and health services are required, but there should also be a favorable milieu and a healthy and just family and social environment that provides opportunities for children to develop their natural qualities. In fact, programs providing social and educational support which focus on non-cognitive aspects may promote substantial changes in overall child development.7 Finally, as occurs in many other fields of health, child development is highly influenced by the social and economic conditions in which children grow up. Even if iodine improves the cognitive maturation of the child, something which is still to be proven, we may speculate that if the social and economic conditions of the family are not favorable, children will not develop their whole potential to the extent that they would do if such conditions were more favorable.8
Proposed framework of determinants of overall child development. IK: potassium iodide. Prepared by the authors from references 3–6.
Two positions are possible in this regard. On the one hand, a complex comprehensive position stemming from the idea that we cannot focus on a single aspect, disregarding all other potential determinants of child development, because the potential benefit from such intervention will be mitigated if all other factors are not changed. The opposite, more pragmatic position is to make a routine recommendation of iodine supplementation alone, with no other associated measures aimed at promoting cognitive child development.9
If we opt for the second position, such adhesion cannot be unconditional. Logic imposes a number of conditions:
- •
That intervention is proven to be safe.
- •
That supplementation is shown to be beneficial for health.
- •
That the measure is cost-effective.
- •
That the implementation of iodine provision programs does not obscure the fact that what is really important is not iodine, but the psychomotor, cognitive, social, and moral development of the child.
Iodine deficiency has greatly decreased in Spain as compared to previous decades. This decrease has partly resulted from the increasing use of iodine supplements and some livestock practices (the iodine enrichment of cattle feeding stuffs and the disinfection of cow udders with povidone iodine have both caused high iodine levels in commercial milk).10 A preparation recently marketed in Spain containing 300μg of potassium iodide already has a 9% market share.11 In addition, the number of families which follow medical advice to use iodine-rich salt and food is increasing. All of these facts have led us to a situation not only far from iodine deficiency, but even close to high total iodine consumption levels, which appear to be associated with an increased risk of thyroid dysfunction.12
On the other hand, no sufficient data are available to state that the strategy of covering iodine requirements in countries with mild to moderate deficiency is effective in preventing iodine deficiency disorders. The clinical trials conducted to date, of disparate quality, have only assessed intermediate variables with a doubtful capacity to predict health outcomes.13 Moreover, positive findings were not replicated in all studies. In studies where statistically significant changes were found as compared to placebo, the results were not always sufficiently relevant to have a potential clinical impact. Two quasi-experimental studies assessed the effect on psychomotor and cognitive child development, but only some slight effects were found due to the poor performance of the measurement tools used.14,15 Thus, there is only inconsistent evidence of improvements in some biochemical parameters, and weak low quality evidence that it may be associated with slight improvements in some functions related to cognitive and psychomotor development.
The belief that exogenous iodine provision is “indispensable” for child development16 may be barring the way to continued research on the subject. A possible example of this is the decision by the research ethics committee of Hospital Carlos Haya in Málaga17 to recommended that no comparison group be used in the Velasco et al.14 study. This prevented the conduct of a randomized, controlled clinical trial with a potassium iodide preparation with a mid-term measurement of cognitive development variables. By contrast, other countries such as France, India, or Thailand appear to be open to the conduct of studies with such characteristics.1 Until data from those trials become available, we must rely on the substantial indirect evidence available to continue recommending iodinated salt and commercial milk to women. However, because of the ‘first do no harm’ principle, we should be cautious before routinely recommending drug supplements.
On the other hand, no cost-effectiveness studies on iodine prophylaxis are available, although supplements containing iodine alone (not associated with other components) are inexpensive and accessible.
Finally, a high number of research groups and public health experts have been working for a long time on iodine deficiency problems in Spain with excellent results. More in-depth study of this subject is required, but this does not mean that we should forget the place that all this work occupies within the wide range of factors influencing child development.
To give or not to give: is this the only question?Clinically, there are many more questions in addition to whether or not potassium iodide should be administered. It remains to be seen what total amount (including all potential provisions) achieves the best benefit-risk balance, and whether the approach of achieving adequate iodine levels by providing drug supplements in the preconceptional status-pregnancy-lactation continuum is appropriate, or only at given times. There are also questions pending about some population subgroups. For example, we should know what to do with hypertensive pregnant women who are sensitive to salt and who are unable to take iodinated salt to prevent blood pressure increase. The same applies to women intolerant to cow proteins, who may be advised not to drink milk. An additional important question is what should be the approach to women with known thyroid dysfunction. It is also indispensable to have local information collected from adequate representative samples in geographic areas, particularly those which are iodine-deficient, to complement and update the already available information.18 An attempt should therefore also be made to answer these questions in specific profiles and populations in order to be able to individualize clinical decisions.
Toward overmedicalization of woman-incubatorThe problem of iodine is an example not only of biomedical reductionism, but also of the medicalization of everyday natural events such as pregnancy and lactation. If the various arms of medicine and its power to decide on what is normal and “abnormal”, “what should and should not be done”, reach only the pregnant woman initially, they subsequently extend to encompass the whole lactation period, and now even to the complete childbearing period. The expansion of these recommendations conditions the life of women in one of the most beautiful stages of their lives by making them responsible for the development of the future child. Intervention is the basic principle, and under this premise we will probably know what deficiency states of other micronutrients have negative effects on health. It is also imperative to eradicate such threats.
The scientific justification of the routine recommendation of iodine supplements also represents an example of an aggressive application of biometrics. Advice focuses on the need to reach given amounts of microelements. Clinical decisions are based on changes in biochemical variables which we intend, sometimes obsessively by continuous monitoring, to return to “normal” levels (although we do not know in most cases if the achievement of such levels is able to predict for the achievement of health benefits). We thus perpetuate a blind faith in numbers, levels, or ranges of questionable clinical relevance.
Another important question is how to measure the expected changes in cognitive or psychomotor development of the child. The availability of widely diverse instruments, which appear to measure different and often not superimposable attributes, and the lack of knowledge of the changes that may be clinically relevant, may cause statistically significant improvements in some sub-indicators of the available tools to be falsely interpreted as global advances in all aspects related to child development.
This biometric idolatry of intermediate variables with no clinical correlates leads to a depersonalized and medicalized health care.19
A golden opportunity for more updated and sensible recommendationsThe Spanish Ministry of Health, Social Services, and Equality is preparing clinical practice guidelines on pregnancy and puerperium in the framework of its National Strategy for Sexual and Reproductive Health.20 This is a golden opportunity to adapt advice to current knowledge. As discussed above, it cannot be stated yet that the recommendation of iodine-containing medicinal products is safe, beneficial for health, and cost-effective. Adequately designed placebo-controlled clinical trials measuring mid- and long-term benefits and health risks should therefore be undertaken, and a recommendation should be withheld until the results of such studies are available.
Moreover, in a context where more natural ways, instead of drug supplements, tend to be used to achieve adequate iodine levels, it is only natural to continue in this direction and to try and guarantee the use of such procedures through specific regulation and adequate control and vigilance mechanisms. This detailed and updated information is indispensable and should be provided by public administrations in order that clinicians are able to take the most appropriate decisions.
Finally, since iodine deficiency is a problem that does not only affect child health, and because overall child development is a multifactorial process that goes beyond the realm of health care, the implementation of intersectoral policies that ensure the adequate development of the physical, mental, social, moral, and spiritual capacities of the child in a healthy and equal opportunity environment should be taken into consideration. We owe it to the children: it is their right.
Conflicts of interestThe authors state that they have no conflicts of interest.
To Rafa Cofiño, Luis Rajmil, and Antonio Villafaina for ideas which were indispensable for writing the text. To the participants in the workshop on iodine and folic acid supplementation during pregnancy and lactation, from which many of the data provided are taken.
Please cite this article as: Gavilán E, Jiménez de Gracia L. Desarrollo global del niño: más allá de la suplementación farmacológica con yodo. Endocrinol Nutr. 2013;60:577–581.
At least 3 randomized and controlled clinical trials with potassium iodide in healthy pregnant women with medium term clinical effects have been registered since the 2nd of April, 2013 in the database of clinicaltrials.gov: http://clinicaltrials.gov/ct2/show/NCT01049659, http://clinicaltrials.gov/ct2/show/NCT00791466 and http://clinicaltrials.gov/ct2/show/study/NCT00379535.