Women with gestational diabetes mellitus (GDM) have an increased risk for developing diabetes mellitus (DM). Their postpartum metabolic classification using a 75g oral glucose tolerance test (75g OGTT) is recommended. The purpose of this study was to assess the value of hemoglobin A1c for postpartum evaluation in women with recent GDM.
Patients and methodsFifty-six women with recent GDM underwent a 75g OGTT at our center to assess postpartum changes in carbohydrate metabolism and were classified using diagnostic criteria of the American Diabetes Association (ADA). Receiver operating characteristic (ROC) curves analysis was used to assess the diagnostic performance of hemoglobin A1c, and kappa index was used to evaluate diagnostic agreement between hemoglobin A1c and 75g OGTT.
ResultsDM was diagnosed in 7 women, and other categories of increased risk for DM in 25 women. Kappa index for diagnosis agreement was 0.22. Hemoglobin A1c≥5.7% had 47% sensitivity and 71% specificity for identifying any change in carbohydrate metabolism. A hemoglobin A1c value≥6.5 had 29% sensitivity and 100% specificity for diagnosis of DM. Area under the ROC curve was 0.57 for identifying any change in carbohydrate metabolism and 0.81 for diagnosis of DM.
ConclusionUsing ADA cutoff values, hemoglobin A1c is not appropriate for postpartum glucose tolerance evaluation in women with recent GDM.
Las mujeres con diabetes mellitus gestacional (DMG) previa presentan mayor riesgo de desarrollar diabetes mellitus (DM). En estas mujeres, se recomienda realizar una reclasificación metabólica después del parto. El objetivo de este estudio fue valorar el rendimiento de la hemoglobina A1c para la evaluación postparto en mujeres con DMG reciente y evaluar la concordancia en el diagnóstico de las distintas formas de alteración de la tolerancia a la glucosa con el test de tolerancia con sobrecarga oral de 75g de glucosa (TTOG 75g), método recomendado actualmente para dicha reclasificación.
Material y métodos56 mujeres con DMG reciente fueron reclasificadas tras el parto en nuestro centro según los criterios de la Asociación Americana de Diabetes (ADA). Se analizó la concordancia en el diagnóstico entre la hemoglobina A1c y el TTOG 75g y se evaluó el rendimiento de la hemoglobina A1c para el diagnóstico de DM y para la detección de cualquier forma de alteración de tolerancia a la glucosa.
ResultadosSe diagnosticó DM en 7 mujeres y otras formas de alteración de la tolerancia a la glucosa en 25. El índice kappa de concordancia en el diagnóstico fue de 0,22. Una hemoglobina A1c ≥ 5,7% presentó una sensibilidad de 47% y una especificidad de 71% para identificar cualquier forma de alteración de la tolerancia a la glucosa. Una hemoglobina A1c ≥ 6,5 presentó una sensibilidad de 29% y una especificidad de 100% para el diagnóstico de DM. El área bajo la curva ROC para la detección de cualquier forma de alteración de la tolerancia a la glucosa fue 0,57 y para el diagnóstico de DM de 0,81.
ConclusionesLa hemoglobina A1c, empleando los puntos de corte de la ADA, no es apropiada para la reclasificación metabólica de mujeres con antecedente reciente de DMG.
Women with a history of GDM have an increased risk of subsequently developing DM.1,2 The Spanish Group of Diabetes and Pregnancy (GEDE) therefore recommends metabolic reclassification of women with GDM after delivery using a 75-g OGTT.3 However, a high degree of noncompliance with this recommendation is seen in daily practice at our healthcare area, which prevents the early diagnosis of these changes and the adoption of preventive and therapeutic measures.
The ADA recently introduced hemoglobin A1c as a diagnostic criterion for DM and other forms of impaired glucose tolerance associated with an increased risk of DM and cardiovascular disease like impaired fasting blood glucose (IFBG) and decreased glucose tolerance (DGT). Hemoglobin A1c values≥6.5% are a diagnostic criterion for DM, while levels ranging from 5.7% to 6.4% define other forms of glucose intolerance.4 This study assessed the value of hemoglobin A1c as a diagnostic criterion for DM and other forms of impaired glucose tolerance in women with a recent history of GDM as compared to 75-g OGTT, the standard criterion used for such diagnosis.
Materials and methodsThis prospective, 12-month study was conducted at Hospital General Básico de la Defensa and Complejo Hospitalario Universitario in Cartagena. Fifty-six women with prior GDM who attended our hospital for a 75-g OGTT at least six weeks after delivery and after the end of breast-feeding were enrolled into the study. An additional blood sample was drawn from all of them after an 8-h fast for measuring hemoglobin A1c. Informed consent for this test was requested from all pregnant women. The study was approved by the Ethics and Research Committee of the hospital.
DM and other forms of impaired glucose tolerance were diagnosed, based on the criteria recommended by GEDE3 and ADA4:
- •
IFBG: fasting blood glucose≥100mg/dL and <126mg/dL.
- •
DGT: blood glucose 2h after administration of a 75-g glucose overload≥140mg/dL and <200mg/dL.
- •
DM: fasting blood glucose (confirmed by a second test)≥126mg/dL or blood glucose 2h after the administration of 75g of glucose≥200mg/dL.
Serum glucose levels were measured by the hexokinase method using HITACHI 917 and Cobas 6000 (Roche Diagnostic) analyzers for which the transferability of results had previously been verified. During the study period, both analyzers met the desirable quality specifications based on biological variability for imprecision (<3.1%) and total error (<7.2%), according to the results of the quality assurance program for clinical laboratories of the Spanish Society of Clinical Chemistry and Molecular Pathology. Hemoglobin A1c was measured by high-performance liquid chromatography using Variant I and Variant II analyzers (Bio-Rad), a methodology certified by the National Glycohemoglobin Standardization Program (NGSP) and standardized against the reference Diabetes Control and Complications Trial, in accordance to ADA recommendations for the use of hemoglobin A1c as a criterion for the diagnosis of DM. During the study period, the method used showed an imprecision less than 4%, the criterion stated in the consensus document for harmonization of hemoglobin A1c results in Spain.5
Statistical analysisSPSS v 15.0 and EPIDAT 3.1/4.0 software was used for statistical data analysis. Quantitative variables are given as mean and standard deviation (SD) or as median (interquartile range). A Student's t test was used for means comparison. A value of p<0.05 was considered statistically significant. A ROC curve analysis was used to assess the diagnostic yield of hemoglobin A1c for the diagnosis of any form of impaired carbohydrate metabolism (IFBG, DGT, and DM) and DM alone. The sensitivity and specificity of hemoglobin A1c for the cut-off points recommended by the ADA for the diagnosis of DM (≥6.5%) and any form of impaired glucose tolerance (≥5.7%) were calculated. A weighted kappa index was also used to analyze the diagnostic agreement between the two criteria, hemoglobin A1c and 75-g OGTT, used as the reference test.
ResultsFifty-six Caucasian women with a mean age of 33.3 (4.6) years and a mean pregestational body mass index of 26.9 (4.8)kg/m2 were enrolled into the study. Mean time after delivery was 11 (2) months.
After delivery, 24 women (42.9%) showed normal glucose tolerance, while 32 women (57.1%) had some form of impaired glucose tolerance: DM was diagnosed in 7 women (12.5%), IFBG in 16 (28.6%), DGT in 2 (3.6%), and IFBG with DGT in 7 (12.5%) women. Women with DM postpartum had significantly higher hemoglobin A1c values as compared to those with no DM (6.1 [0.6] vs 5.5% [0.4]; p<0.05). However, there was no difference in hemoglobin A1c between women with normal glucose tolerance and those with any form of impaired glucose tolerance (IFBG, DGT, or DM) (5.5 [0.4] vs 5.6% [0.5]).
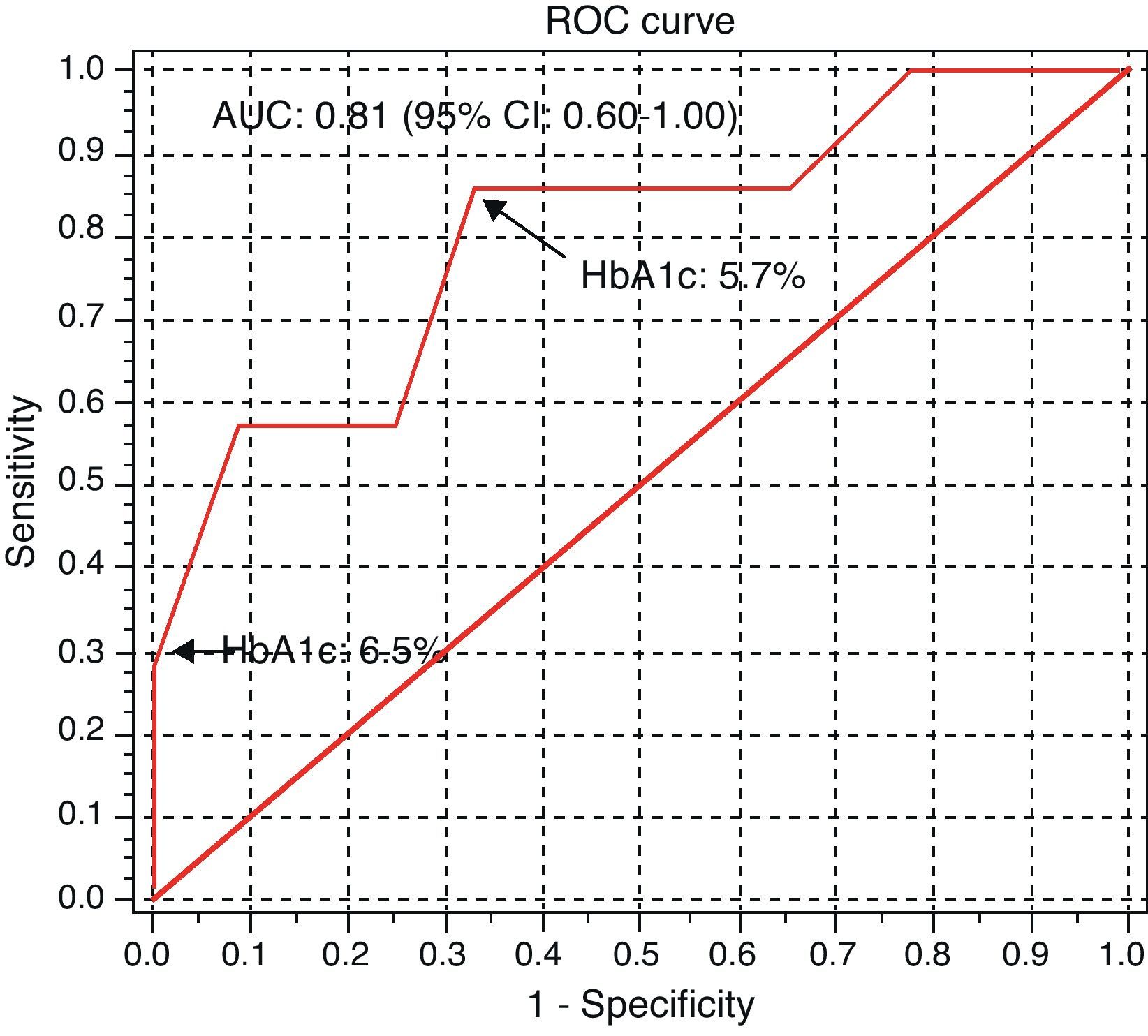
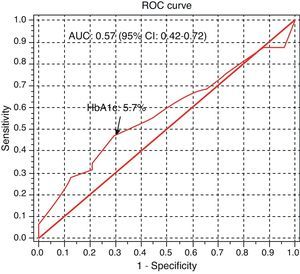
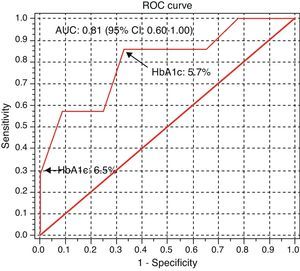
The area under the ROC curve of hemoglobin A1c for the detection of any form of impaired carbohydrate metabolism was 0.57 (95% confidence interval (CI): 0.42–0.72; Fig. 1), with 47% sensitivity and 71% specificity for a value≥5.7%. The area under the ROC curve of hemoglobin A1c for the diagnosis of DM was 0.81 (95% CI: 0.60–1.00; Fig. 2), with 29% sensitivity and 100% specificity for a value≥6.5%. The hemoglobin A1c value with the highest yield for the diagnosis of DM was 5.7%, which showed 86% sensitivity and 67% specificity.
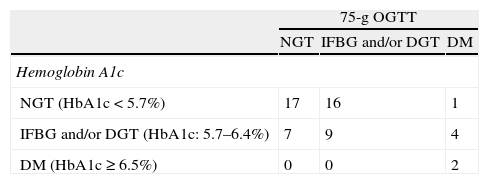
The kappa index of agreement in the diagnosis of the different forms of impaired carbohydrate metabolism using hemoglobin A1c and 75-g OGTT was 0.22 (95% CI: 0.002–0.45). Twenty-eight women (50%) were erroneously classified when hemoglobin A1c was used as the criterion to diagnose the different forms of impaired glucose tolerance (Table 1); hemoglobin A1c underestimated the diagnosis in 21 women (37.5%) and overestimated the diagnosis in 7 women (12.5%).
Agreement in diagnosis of the different forms of impaired carbohydrate metabolism using hemoglobin A1c (HbA1c) and a 75-g oral glucose tolerance test (75-g OGTT).
| 75-g OGTT | |||
| NGT | IFBG and/or DGT | DM | |
| Hemoglobin A1c | |||
| NGT (HbA1c<5.7%) | 17 | 16 | 1 |
| IFBG and/or DGT (HbA1c: 5.7–6.4%) | 7 | 9 | 4 |
| DM (HbA1c≥6.5%) | 0 | 0 | 2 |
DM: diabetes mellitus; IFBG: impaired fasting blood glucose; DGT: decreased glucose tolerance; NGT: normal glucose tolerance.
GDM is the most common metabolic disorder during pregnancy, with a prevalence rate of 8.8%6 in our environment, and is associated with increased fetal and maternal morbidity, including an increased risk of developing DM, mainly of type 2, and other forms of impaired glucose tolerance after delivery.1 Postpartum monitoring is therefore required to detect any changes in carbohydrate metabolism and associated conditions such as metabolic syndrome.
Despite the small sample size and the short time elapsed after delivery, this group of women had prevalence rates of DM and IFNG and/or DGT of 12.5% and 44.6%, higher than reported in similar studies.7,8
Metabolic reclassification of women with GDM is currently based on an OGTT. The high degree of noncompliance with such reclassification seen in our healthcare area led us to consider the use of hemoglobin A1c, a parameter recently included as a criterion for the diagnosis of DM and other forms of impaired glucose tolerance that does not require fasting measurement or an oral glucose overload, as a diagnostic tool to improve the monitoring of these women, thus contributing to the early diagnosis of DM and to the identification of women at an increased risk of suffering DM and cardiovascular disease.
This study found a weak agreement between metabolic reclassification using hemoglobin A1c and 75-g OGTT, with a high proportion of women inadequately reclassified when hemoglobin A1c was used as the criterion. Moreover, hemoglobin A1c yield using the cut-off points recommended by the ADA is not adequate for the diagnosis of DM or for the detection of any form of glucose intolerance. In a recent study with a sample of a similar size, Kim et al.9 showed an area under the curve for detecting any change in carbohydrate metabolism of 0.76, greater than the one found in this study, with 75% sensitivity and 62% specificity for a cut-off point of 5.7%. Such differences in diagnostic yield are probably due to two factors: the recruitment of women of different ethnic origins, because of the influence of race on hemoglobin A1c values,10 and the recruitment of women with a longer time from delivery to reclassification, because the correlation between hemoglobin A1c and blood glucose under fasting conditions and after OGTT was stronger in women reclassified more than one year after delivery than in those reclassified before one year had elapsed after delivery.
In conclusion, it is inferred from our study that, when the cut-off points recommended by the ADA are used, hemoglobin A1c is not a helpful marker for postpartum metabolic reclassification in women with a recent history of GDM. A potential explanation could be the change in lifestyle and dietary habits, and in some cases the need for therapeutic intervention with insulin, required after the diagnosis of GDM to maintain normal glycemia. This would justify the stronger correlation between hemoglobin A1c and fasting blood glucose reported by Kim et al.9 in pregnant women in whom a longer time had elapsed between delivery and reclassification. Hemoglobin A1c measurement is widely available. However, before its use as a diagnostic criterion for glucose intolerance in this population can be recommended, it will be necessary to conduct studies on larger samples in order to validate the recommended cut-off points or to redefine them, taking into account the potential influence of factors such as the time elapsed after delivery and the ethnic origin of the patients.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: García de Guadiana Romualdo L, et al. Utilidad de la hemoglobina A1c en el diagnóstico de diabetes mellitus y otras alteraciones del metabolismo glucídico en mujeres con diabetes mellitus gestacional reciente. Endocrinol Nutr. 2012;59:362–6.