Routine thyroid ultrasound examination in a single medical appointment is rarely performed in Spain. The objective of this study was to evaluate the care and economic impact of thyroid US examination in a single endocrine appointment.
MethodsA prospective, observational, descriptive study was conducted to analyze data from 2274 patients (mean age, 59±16 years; 83% females) performed at least one thyroid US in a single visit to an endocrinology clinic during 2013 and 2014. The number of endocrine acts with thyroid US, single endocrine and US acts without review, and the change in the number of thyroid US requested by endocrinologists to the radiology department and total thyroid US examinations performed at the radiology department during the study period were assessed.
ResultsIn 2013 and 2014, 2558 endocrine acts with thyroid US were performed, of which 42.2% were single endocrine and US appointments without a second endocrine act, with estimated savings of €58,946.40. As compared to 2012, the number of thyroid US requested by endocrinologists to the radiology department decreased by 43.3% and 86.0% in 2013 and 2014 respectively, and total thyroid US performed by the radiology department decreased by 28.1% and 68.3% respectively, with estimated savings of €94,441.36.
ConclusionsThyroid US examination in a single endocrine appointment allows for decreasing the number of both second endocrine acts and thyroid US examinations performed at the radiology department, thus reducing the number of unnecessary clinic visits and promoting considerable economic savings.
La realización de ecografía tiroidea en consultas en acto único está escasamente implantada en nuestro país. El objetivo de este estudio fue evaluar el impacto asistencial y económico de la utilización de la ecografía tiroidea en consultas de endocrinología en acto único.
MétodosSe trata de un estudio prospectivo, observacional y descriptivo en el que se analizaron los datos de 2.274 pacientes (edad media: 59+/-16 años; 83% mujeres) a los cuales se les realizó al menos una ecografía tiroidea en acto único en consultas de endocrinología durante 2013 y 2014. Se evaluaron el número de consultas de acto único, consultas con alta directa y la variación en el número de ecografías solicitadas y realizadas en radiodiagnóstico durante el período de estudio.
ResultadosEn 2013 y 2014 se realizaron 2.558 ecografías tiroideas en consultas de endocrinología en acto único, siendo el 42,2% consultas de alta directa sin revisión de resultados, con un ahorro estimado de 58.946,40 euros. En 2013 y 2014 se redujo el número de ecografías solicitadas a radiodiagnóstico en un 43,3% y 86,0%, respectivamente. De forma global se realizaron en radiodiagnóstico un 28,1% y un 68,3% menos ecografías tiroideas respecto al año 2012, estimándose un ahorro económico de 94.441,36 euros.
ConclusionesLa realización de ecografías tiroideas en consultas de endocrinología en acto único permite reducir tanto el número de revisiones de recogida de resultados como las ecografías tiroideas realizadas en radiodiagnóstico, lo cual disminuye el número de desplazamientos innecesarios de pacientes y favorece un ahorro económico considerable.
Thyroid disease currently represents one of the main reasons for referral to endocrinology outpatient clinics1,2 because of both the high prevalence of thyroid conditions in the general population3,4 and the expansion of hormone measurements and imaging procedures, which have led to a marked increase in the detection of both impaired thyroid function and incidentalomas in the thyroid gland.2,4 While approximately 4%–7% of the general population has palpable thyroid nodules, imaging tests reveal nodules in up to 20%–70% of the population.4,5
Thyroid ultrasonography (US) is the most important imaging procedure for diagnosing thyroid disease.5 US has evolved in recent years thanks to the design of increasingly compact and manageable equipment with improved quality and definition. This has allowed for the increasing use of this equipment at clinics, rather than at radiodiagnosis units.6,7 The performance of thyroid US at single visits to endocrinology clinics might therefore be expected to lead to cost reductions by reducing the number of visits necessary–both to the radiodiagnosis unit for the performance of thyroid US and subsequently to the endocrinology clinic a second time to be given the results. However, this has not been confirmed by clinical studies.
Following the model of the Thyroid Core Group of the Mayo Clinic,8 the endocrinology unit of our center has been performing thyroid US since January 2013. Patients are only referred to the radiodiagnosis unit for more comprehensive US in the event of difficult or doubtful diagnosis. This model of care at a single visit to the endocrinology clinic (with clinical, hormonal, and US assessment by the endocrinologist on the same day) is still uncommon in Spain6,7 and coexists with the predominant organizational model, in which patients are evaluated by the endocrinologist, who requests US or US-guided fine-needle aspiration (US-FNA) of the thyroid gland, which is then performed on a different day and whose results are assessed by the endocrinologist at another visit (thus patients usually have to attend the center on three different days).9 It is therefore necessary to assess whether thyroid US at a single visit to the endocrinology clinic allows for direct savings in costs by reducing the number of appointments, both to the radiodiagnosis unit and subsequently to endocrinology.
MethodsThe Thyroid Ultrasound in Endocrinology (ETIEN) study was designed in January 2013 as a prospective, observational, descriptive study intended to assess the clinical results and the care and economic impact of the implementation of thyroid US at single visits to the endocrinology outpatient clinics of Hospital Universitario Puerto Real in Cádiz, Spain. The purpose of the ETIEN 1 substudy was to assess the economic impact of the use of thyroid US at a single visit during the first two years (2013 and 2014) of its implementation. The 2274 patients (mean age, 59+/−16 years; 83% females) seen at the endocrinology unit for thyroid disease who had at least one US performed at endocrinology clinics during 2013 and 2014 were considered candidates for inclusion in the analysis.
Thyroid disease assessmentSince 2010, the approach to the diagnosis of thyroid nodule and dysfunction at our hospital has been based on a protocol that coordinates the activities of the endocrinology, radiodiagnosis, general surgery, and pathology departments. The protocol was revised on 2012 and 2014, and annual evaluations have shown a high level of compliance. The criteria for the referral of patients with thyroid disease (thyroid dysfunction and nodule) to endocrinology clinics are in accord with those for primary care and include the need for previous TSH measurement to characterize thyroid hormone function before referral.
Patients with thyroid disease (suspected or documented) are usually referred to our unit by primary care or other specialties, and are assessed by an endocrinologist from the unit. Until January 2013, both thyroid US and US-FNA were performed exclusively at the radiodiagnosis unit of the hospital, but after that date, the performance of thyroid US and US-FNA at single visits to endocrinology clinics was gradually introduced. Thus, by the end of 2014, approximately 81% of all thyroid US tests performed on our patients were done by endocrinologists at the clinic itself. All the US tests at the unit were performed using digital portable Sonosite Micromax US equipment with a 6–13Mhz broadband linear transducer. In order to prevent bias in the indication of thyroid US, there were no restrictions on indicating US in any of the periods evaluated, and endocrinologists used their clinical judgment to decide both the indication of the procedure and whether they would perform it themselves or request it from radiodiagnosis. The main indications were thyroid nodules, goiter, and thyroid cancer follow-up.
In our unit, patients with no significant disease, hormonally stabilized, and with no criteria for performing US-FNA or surgical exploration are discharged on the same day (direct discharge visit with no review of results), while all other patients are appointed for a review of hormone and/or cytological results (if thyroid US-FNA has been requested). Finally, patients with thyroid nodules who are candidates for thyroidectomy are referred to the surgical unit, while patients with no surgical criteria and hormonal stability are discharged.
Study variables and cost saving estimationThe variables analyzed included age, sex, place of origin, the number of thyroid US tests and US-FNAs performed at the unit and the type of visit (a visit to a high-performance clinic with no review of the results or a single visit with a subsequent appointment for a review). The radiodiagnosis unit provided information on the number of thyroid US tests requested by physicians from the unit in the 2011–2014 period, and on the total number of thyroid US and US-FNAs performed by the radiodiagnosis unit during the same period.
To estimate the potential financial savings using the model of the single endocrinology visit, only the direct costs of health care not performed were considered. These included both the cost of a thyroid US that would theoretically have been performed at the radiodiagnosis unit and the cost of control at endocrinology of patients attending a direct discharge visit with no subsequent review of the results. Direct costs were calculated using the prices listed in the order of October 14, 2005 of the Department of Health of the government of Andalusia that established the public prices of the health services provided by centers dependent on the Andalusian public health system.10 A cost sensitivity analysis was subsequently carried out to assess the economic consequences of the impact of changes in the set prices by a simple univariate analysis of minimum and maximum costs11 using the updated reference prices in five Spanish autonomous communities.12–16
Statistical analysisPatient data were entered into a database of the Microsoft Access 2007 database, and statistical analysis was performed using the Statistical Package for the Social Sciences version 11.0. Continuous variables were displayed as mean±standard deviation, while qualitative variables were given as absolute and relative frequencies (percentages). The results of sensitivity analysis for financial costs are given as a range of the minimum and maximum costs, based on the different reference prices of thyroid US and control visits to endocrinologists established in the autonomous communities evaluated.
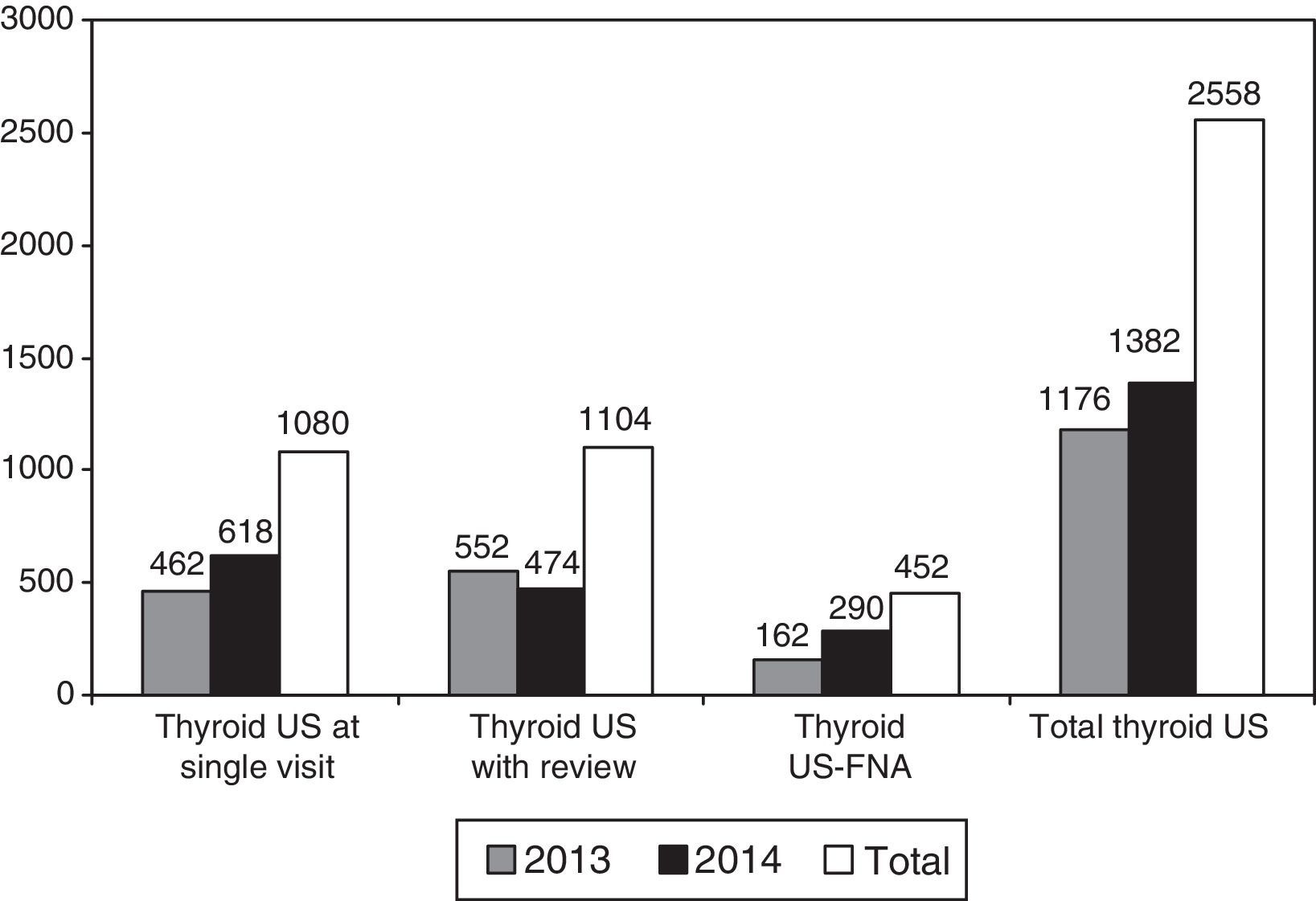
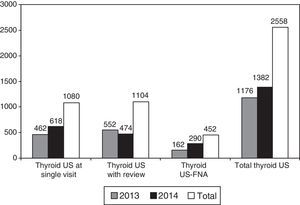
ResultsDuring 2013 and 2014, 2558 thyroid US tests were performed at endocrinology clinics, with a 17% increase in 2014 as compared to 2013 (1382 versus 1176). Of all US tests, 42.3% were performed at a single visit with direct discharge and no appointment for a review of the results (Fig. 1), while in the remaining 57.7% of cases at least one subsequent appointment was required for further study after diagnostic tests were requested, including thyroid US-FNA, performed in 452 patients.
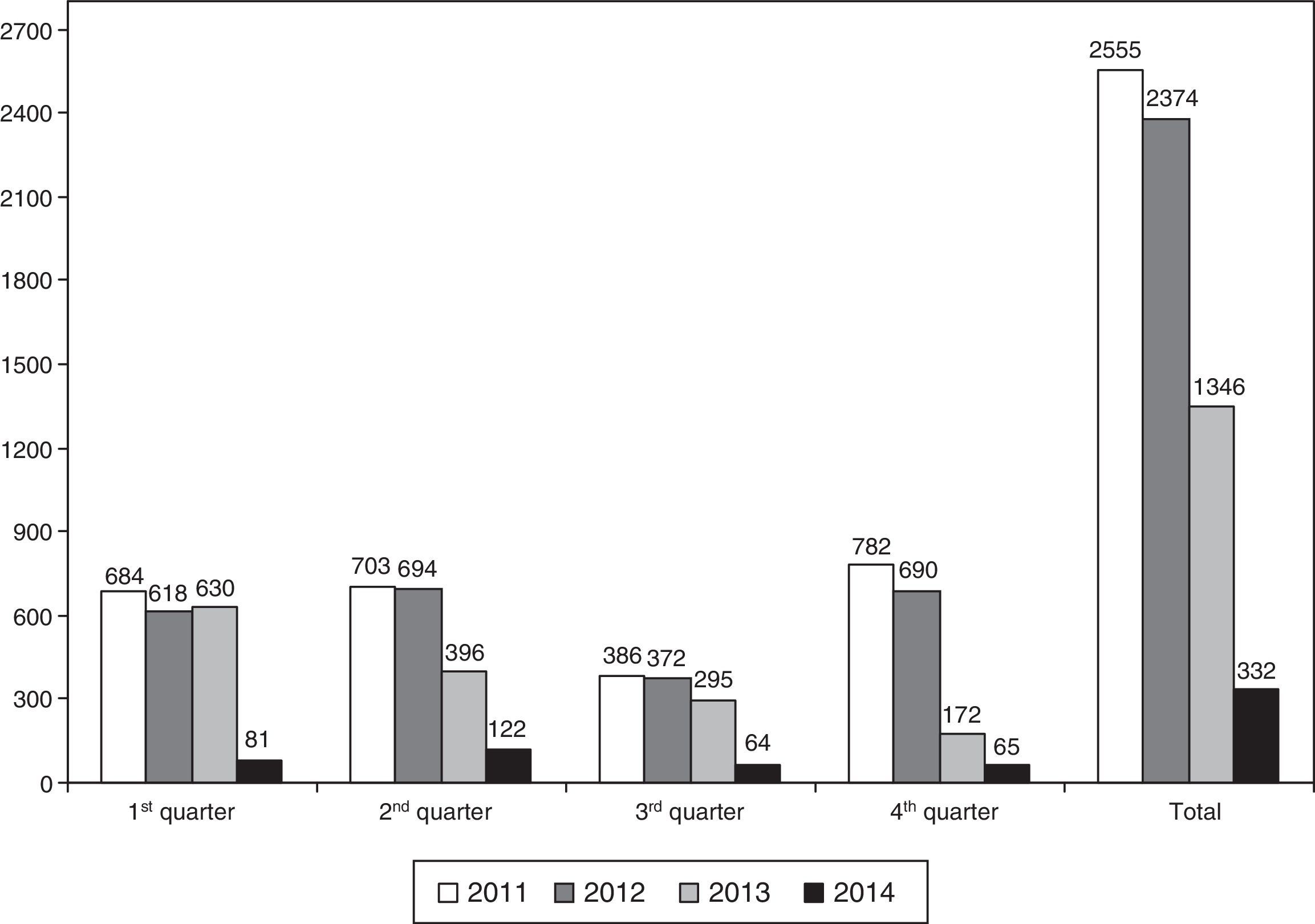
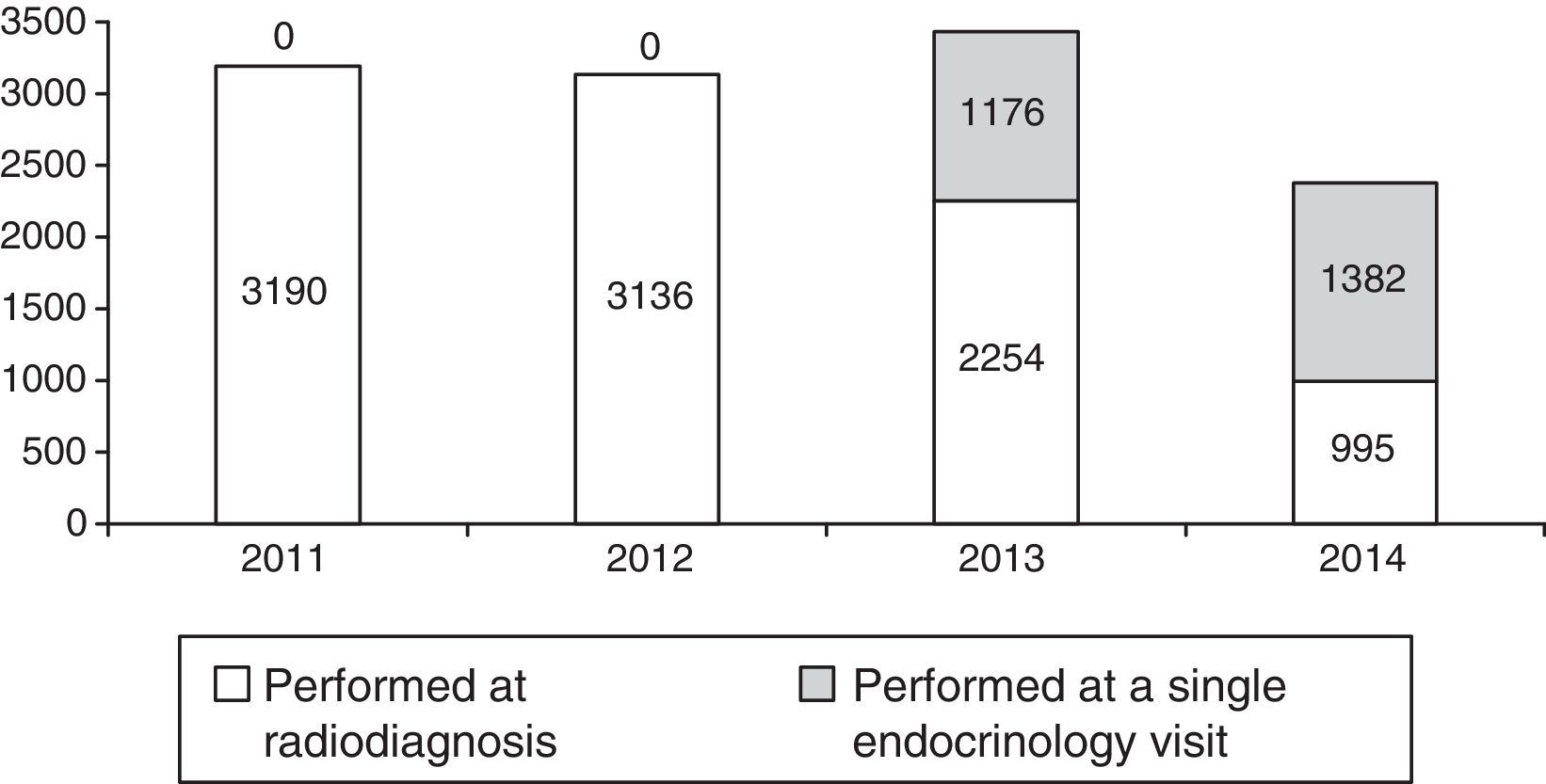
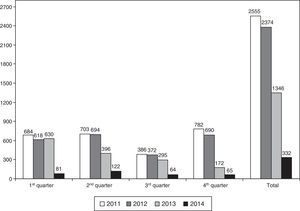
The number of thyroid US tests requested from the radiodiagnosis unit by endocrinologists decreased in parallel, so that, as compared to 2012 (before thyroid US was implemented at endocrinology clinics), the number of thyroid US tests requested decreased by 43% and 86% in 2013 and 2014 respectively (Fig. 2). In this regard, it should be noted that in 2014, 2042 fewer US tests were requested from the radiodiagnosis unit as compared to 2012.
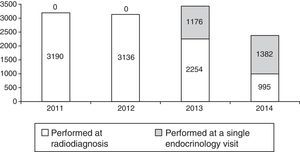
Fig. 3 shows the change over time in thyroid US performed at our hospital between 2011 and 2014. While 100% of thyroid US tests were carried out at the radiodiagnosis unit during 2011 and 2012, only 65.7% and 41.9% of all procedures were performed there in 2013 and 2014 respectively. On the other hand, while in 2013 the total number of thyroid US procedures performed at the hospital increased by 9.4% as compared to 2012, a 24.2% reduction occurred in 2014.
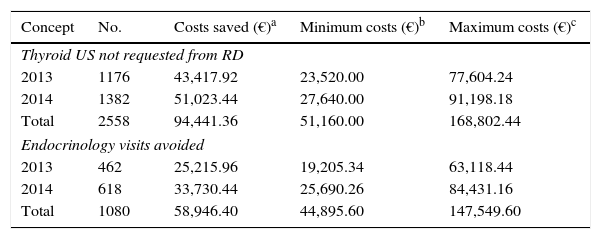
Table 1 shows the potential direct financial savings derived only from the non-performance of thyroid US at the radiodiagnosis unit and the non-appointment for a subsequent visit to the endocrinology clinic for a review of the results. Savings estimated in 2013 and 2014 were €94,441.36 (cost range in the sensitivity analysis: €51,160.00–168,802.44), derived from the non-performance of 2558 thyroid US tests at the radiodiagnosis unit, and €58,946.40 (cost range in the sensitivity analysis: €44.895,60–147.549,60) from the avoidance of 1080 visits to endocrinology clinics for a review of the results.
Estimate of the potential savings in direct costs in the model of ultrasonography at single visits to endocrinology clinics during the study period.
| Concept | No. | Costs saved (€)a | Minimum costs (€)b | Maximum costs (€)c |
|---|---|---|---|---|
| Thyroid US not requested from RD | ||||
| 2013 | 1176 | 43,417.92 | 23,520.00 | 77,604.24 |
| 2014 | 1382 | 51,023.44 | 27,640.00 | 91,198.18 |
| Total | 2558 | 94,441.36 | 51,160.00 | 168,802.44 |
| Endocrinology visits avoided | ||||
| 2013 | 462 | 25,215.96 | 19,205.34 | 63,118.44 |
| 2014 | 618 | 33,730.44 | 25,690.26 | 84,431.16 |
| Total | 1080 | 58,946.40 | 44,895.60 | 147,549.60 |
€: euro; US: ultrasonography; RD: radio-diagnosis.
High-performance (or single visit) outpatient clinics aim at resolving the health problem of a patient on the same day of the visit by performing the supplemental tests adequate for that purpose. High-performance cardiology clinics, introduced throughout Spain and performing most supplemental examinations required for patient work-up (electrocardiogram, echocardiogram, etc.), are a good example of this approach and have proven positive efficiency results.17,18
Thyroid disease is among the most common reasons for referral to endocrinology clinics,1,2 at which US to detect goiter or thyroid nodules, or US-FNA to rule out thyroid cancer, present in approximately 5% of thyroid nodules, may be required.19 A one-stop clinic where the endocrinologist integrates clinical, hormonal, and US information from the patient in a single visit, and decides the most adequate therapeutic approach, has been shown to be cost-effective and efficient for decreasing waiting times.6,7 However, this organizational model is little used in Spain9,20 and coexists with other models in which patients undergo clinical and hormonal evaluation by the endocrinologist and US by the radiologist.21 This requires greater coordination between units and more frequent visits by patients to the healthcare center, which significantly impairs system efficiency.22 As an example, a patient who attends an endocrinology one-stop clinic and undergoes thyroid US, but requires no additional appointment for a review of the results incurs in our autonomous community a theoretical cost of €114.12 (first visit).10 By contrast, the “theoretical invoice” with the model of a first visit to endocrinology (€114.12), plus thyroid US at the radiodiagnosis unit (€36.92) plus a visit to endocrinology for review of results (€54.59), would amount to €205.63.
The results of this study support the concept that a one-stop or high-performance clinic for thyroid disease incorporating thyroid US or US-FNA represents an alternative to other organizational systems that improves the efficiency of the health system. This approach requires ultrasound equipment to be purchased or transferred from radiodiagnosis units, but this financial investment is rapidly compensated by savings in US performed by the radiodiagnosis unit, estimated in our study at €94,441 in two years (€51,160.00–168,802.44 in sensitivity analysis). In addition, a decrease in the number of thyroid US tests requested from radiodiagnosis units could make possible a reduction in the waiting times for other US procedures requested by other specialties. Moreover, a one-stop clinic allows for improvements in the management of endocrinology clinics by decreasing the number of unnecessary appointments for the collection of US results, with potential savings estimated in our study of €58,946.40 in two years (€44,895.60–147,549.60 in the sensitivity analysis).
As this was a study analyzing direct costs, this research did not consider the potential economic savings to be derived from decreased expenses for travel to the center or for less time off work, among other factors. Finally, patient satisfaction is likely to increase, because waiting times are markedly decreased, the indirect costs associated with subsequent visits are reduced, and anxiety caused by delays in diagnosis and treatment is minimized.23
To conclude, thyroid US at endocrinology clinics makes it possible to reduce both the number of thyroid US tests requested from and performed by the radiodiagnosis unit and the number of return visits to the endocrinology clinic to find out the results, thus decreasing unnecessary patient travel and promoting substantial economic savings.
Conflicts of interestThe authors of this article have no conflicts of interests in relation to the objective or the results of this article.
This study was funded by the SAEN 2013 research grant and the 2015 SEEN Foundation grant for research in thyroid pathology.
Please cite this article as: Carral F, Ayala MC, Jiménez AI, García C. Impacto asistencial y económico de la ecografía tiroidea en acto único en consultas de endocrinología (estudio ETIEN 1). Endocrinol Nutr. 2016;63:64–69.