Neonatal sepsis can be classified as early onset or vertical transmission and late onset (LOS), depending on the timing of the appearance of symptoms. LOS is generally nosocomial.1 In the latest Spanish study on LOS,2 730 cases of sepsis were diagnosed in 662 newborns out of a total of 30,993 hospitalised newborns. This gives an incidence of 2.4%, and an incidence density rate of 0.89 per 1000 days of admission. At present, nosocomial infections are the leading cause of morbidity and mortality in neonatal units (10–15%).1
We present a retrospective, descriptive study conducted in a level IIIB neonatal intensive care unit (NICU) that included all patients admitted between January 1, 2010 and December 31, 2014 with a positive blood culture and a diagnosis of LOS according to the Centre for Disease Control and Prevention (CDC) criteria.3 In patients with suspected LOS, at least 1ml of blood was collected and introduced into a paediatric BD BACTEC Peds Plus/F blood culture bottle (Becton Dickinson, USA) and incubated in the Bactec FX automated system for up to 5 days. Positive samples were then reseeded in standard media and analysed using mass spectrometry (MALDI-tof, Bruker Diagnostics, Germany). Isolates were confirmed against the antibiogram using the Microscan system (Beckman Coulter, USA). The study was approved by our hospital's Ethics Committee.
We observed an incidence of LOS of 6.8%, with an incidence density of 4 cases per 1000 days of admission. The median weight at birth was 1420g (interquartile range [IQR]: 990–2310g) and mean gestational age was 31 weeks (95% confidence interval [95% CI] 23–40.5). The median days of life at onset was 10 (IQR: 6–22). In total, 99 patients (67%) received parenteral nutrition (median duration of 8 days, IQR: 5–14) for other reasons at the time of onset of the infectious disease; 35 patients (24%) were intubated (median duration of 7 days, IQR: 5–26) before onset of LOS and 135 patients (92%) had a central venous catheter (median duration of 10 days, IQR: 6–23) at the time of onset of sepsis symptoms. The median length of hospital stay was 39 days (IQR: 19–63).
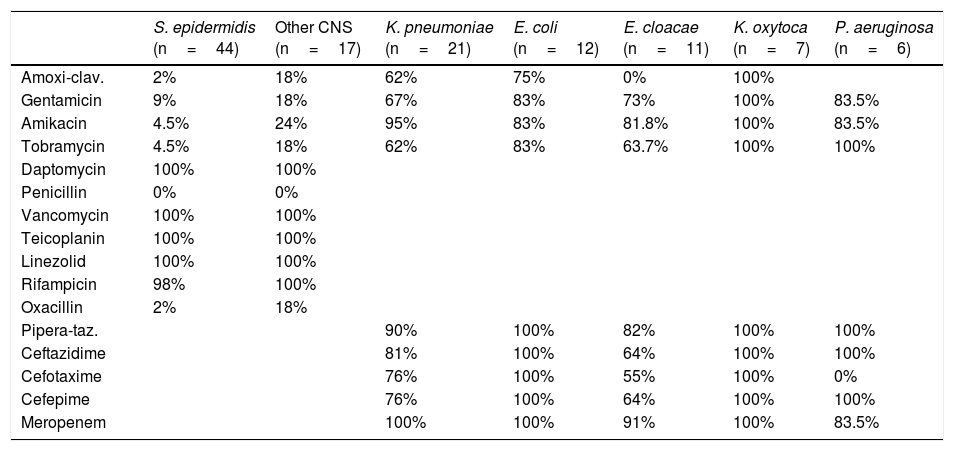
The most frequently isolated microorganisms were: Staphylococcus epidermidis 30% (44/147), Klebsiella pneumoniae (K. pneumoniae) 14% (21/147), Escherichia coli 8% (12/147), Enterobacter cloacae (E. cloacae) 7.5% (11/147), Staphylococcus haemolyticus 5% (7/147), Klebsiella oxytoca 5% (7/147), Staphylococcus hominis 4% (6/147), Candida albicans 4% (6/147), Candida parapsilosis 4% (6/147), Pseudomonas aeruginosa (P. aeruginosa) 4% (6/147), Staphylococcus capitis 3% (4/147) and Enterococcus faecalis 2% (3/147). The antibiotic sensitivities of these bacteria are shown in Table 1. Eight cases of extended-spectrum beta-lactamase (ESBL) producing E. cloacae (73%) and 5 of ESBL-producing K. pneumoniae (24%) were found among the isolates.
Percentage of antimicrobial sensitivity of the most frequently isolated bacteria.
| S. epidermidis (n=44) | Other CNS (n=17) | K. pneumoniae (n=21) | E. coli (n=12) | E. cloacae (n=11) | K. oxytoca (n=7) | P. aeruginosa (n=6) | |
|---|---|---|---|---|---|---|---|
| Amoxi-clav. | 2% | 18% | 62% | 75% | 0% | 100% | |
| Gentamicin | 9% | 18% | 67% | 83% | 73% | 100% | 83.5% |
| Amikacin | 4.5% | 24% | 95% | 83% | 81.8% | 100% | 83.5% |
| Tobramycin | 4.5% | 18% | 62% | 83% | 63.7% | 100% | 100% |
| Daptomycin | 100% | 100% | |||||
| Penicillin | 0% | 0% | |||||
| Vancomycin | 100% | 100% | |||||
| Teicoplanin | 100% | 100% | |||||
| Linezolid | 100% | 100% | |||||
| Rifampicin | 98% | 100% | |||||
| Oxacillin | 2% | 18% | |||||
| Pipera-taz. | 90% | 100% | 82% | 100% | 100% | ||
| Ceftazidime | 81% | 100% | 64% | 100% | 100% | ||
| Cefotaxime | 76% | 100% | 55% | 100% | 0% | ||
| Cefepime | 76% | 100% | 64% | 100% | 100% | ||
| Meropenem | 100% | 100% | 91% | 100% | 83.5% |
The prevalence of LOS varied greatly (up to 4.9% or up to 3.8 cases per thousand days of admission).1,2 Although our figures are slightly higher, they were influenced by the ESBL E. cloacae outbreak in 2011 involving a total of 8 patients and 2 fatalities. Had the average of 2.5 cases occurred in any other year, our incidence density would be 3.2 cases per 1000 days of admission.
The most important factor in the development of LOS was venous catheters, which were used in the vast majority of our patients for a duration similar to that reported in the literature.4 Symptoms, however, appear earlier in our centre.5 This could be related to catheter management. In half of all cases, parenteral nutrition was scheduled to be withdrawn over the following days, which could also be a point of improvement, despite the fact that duration of parenteral nutrition in our hospital is similar to or even better than that of other centres.6 Use of endotracheal intubation in our centre does not differ from earlier studies.4
Due to the aforementioned outbreak, the relative frequency of E. cloacae in our hospital is slightly higher than other centres,7 but no significant differences were observed in the frequency of other microorganisms.4
The sensitivity profile of our gram-positive bacteria was largely similar to that observed in other non-Anglo-Saxon countries.8 Gram-negative bacteria, even with a good profile for P. aeruginosa, show greater sensitivity to aminoglycosides (75%) than that described in developing countries,9 but far less than susceptibility data from developed countries.10 The sensitivity to carbapenems was higher (93%) than that reported in the literature,10 even though we observed several cases of drug-resistant E. cloacae and P. aeruginosa. With regard to cephalosporins, bacteria showed high sensitivity to cefepime (76.5%),10 but not to cefotaxime. This could also be due to the presence of several ESBL-producing strains.
Please cite this article as: Alonso-Ojembarrena A, Marín-Lozano ÁC, Galán-Sánchez F, Rodríguez-Iglesias MA. Etiología y frecuencia de factores de riesgo de sepsis tardía en una unidad de cuidados intensivos neonatales de nivel IIIb. Enferm Infecc Microbiol Clin. 2018;36:144–145.