A 67-year-old woman who underwent a kidney transplant two months prior, developed an erythematous plaque with coalescent purplish nodules on the back of her right hand during the month after the transplant (Fig. 1), with no fever or systemic symptoms. She was on immunosuppressive therapy with prednisone, mycophenolate mofetil and tacrolimus. The lesion appeared after traumatic peripheral venous cannulation, and it was treated initially as bacterial cellulitis, with oral antibiotherapy, with no response. She also presented with a small purplish nodule on the lateral side of her right foot (Fig. 2), which the patient said had appeared after manipulating with her hands a wound caused by her shoes.
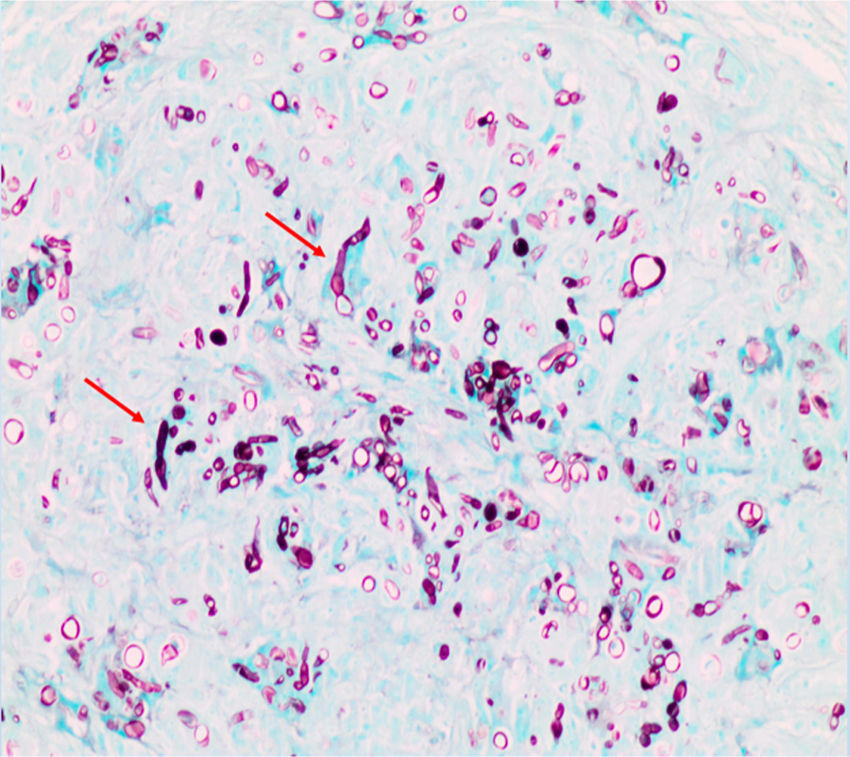
After a torpid clinical course, skin biopsies of the back of her hand and of the nodule on the lateral side of her right foot were carried out. The histological study with the Grocott technique enabled fungal structures corresponding to a dematiaceous fungus affecting the mid and deep dermis to be observed (Fig. 3, red arrows). Samples from both biopsies were sent for microbiological culture, and growth of Alternaria spp. was observed.
Chest X-ray and blood cultures were performed, which ruled out seedings or haematogenous spread. The patient received treatment with posaconazole IV (300 mg/12 h) for one month with rapid improvement a few weeks after starting treatment. Subsequently, she continued with oral posaconazole 300 mg daily until she had completed a total of six months of antifungal treatment, achieving complete resolution of both lesions.
Final comments/discussionPhaeohyphomycosis is a group of mycoses in which dematiaceous fungi intervene, in the form of budding yeast or in the form of hyphae. These organisms are generally considered to be saprophytic or commensal. Alternaria is a saprophytic dematiaceous fungus of the soil and a plant pathogen, which rarely causes infections in immunocompetent individuals,1 with cutaneous or subcutaneous involvement being the most common (74.3%), causing eye infections, rhinosinusitis and onychomycosis on a less frequent basis.1 Only 56 cases of alternariosis have been gathered in the literature in the last 10 years,2 and 212 since the first case was published in 1933.1–3 The main risk factor for suffering from the infection is immunosuppression, with 71% of the cases collected in a review being individuals who had undergone a solid organ transplant and 11% patients with haematological malignancies.2 The manner in which the infection starts is not clearly established, although it seems that the history of skin wound has to be present.4 It is more common in males, in Mediterranean countries and the extremities are the most commonly affected place.1,2,5
The clinical manifestations of the skin infection caused by alternaria are highly varied. In the superficial (epidermal) forms, erythematosus and desquamative areas with papular elements appear which tend to erode and flake,1–3 while the deeper (dermal) forms are generally preceded by a penetrating trauma, tend to present as a purplish plaque, which is sometimes painful, and tend to form ulcers.2,6 The time range between inoculation and the appearance of the lesions ranges between two months and several years.7
Although on many occasions the spores can be detected in the histological image,2,7 the diagnosis of Alternaria spp. infection requires isolation of the fungus by culture. In this, the morphology of the conidia and whether or not there is formation of conidial chains are the main element with which the diagnosis is established.1 However, the microorganism is often not able to sporulate, and, consequently, they cannot be detected under the microscope or are difficult to distinguish from other contaminating forms. On these occasions, molecular biology techniques have to be used for the definitive diagnosis.8,9
The prognosis of this condition is insidious, and the treatment is not clearly standardised, meaning that greater cure rates have been achieved with the combination of surgery and systemic antifungal therapy.2,7,8 Cases of resolution with the exclusive use of thermotherapy have been described, as the slowing down of the proliferation of the fungus in vitro at a temperature of 37 °C has been found.8 Itraconazole (between 100–600 mg/day with a variable treatment duration), voriconazole, fluconazole and posaconazole have been used as systemic antifungals, with the former being used on a large number of occasions and showing cure rates in monotherapy of 60%.2,5,8 Surgery alone is acceptable for small and localised lesions.
FundingThe authors declare that they did not receive funding to complete this study.
Please cite this article as: Sendín-Martín M, Nieto-García FJ, García-Bolaños JA, Pulpillo-Ruiz Á. Lesiones cutáneas en la mano de una paciente trasplantada. Enferm Infecc Microbiol Clin. 2019. https://doi.org/10.1016/j.eimc.2019.04.005