Foruncular myiasis is a rare entity in our environment and, as it is usually an imported disease, it is poorly known and suspected in our country. Hence the importance of reporting the very few cases that come across in our health system.
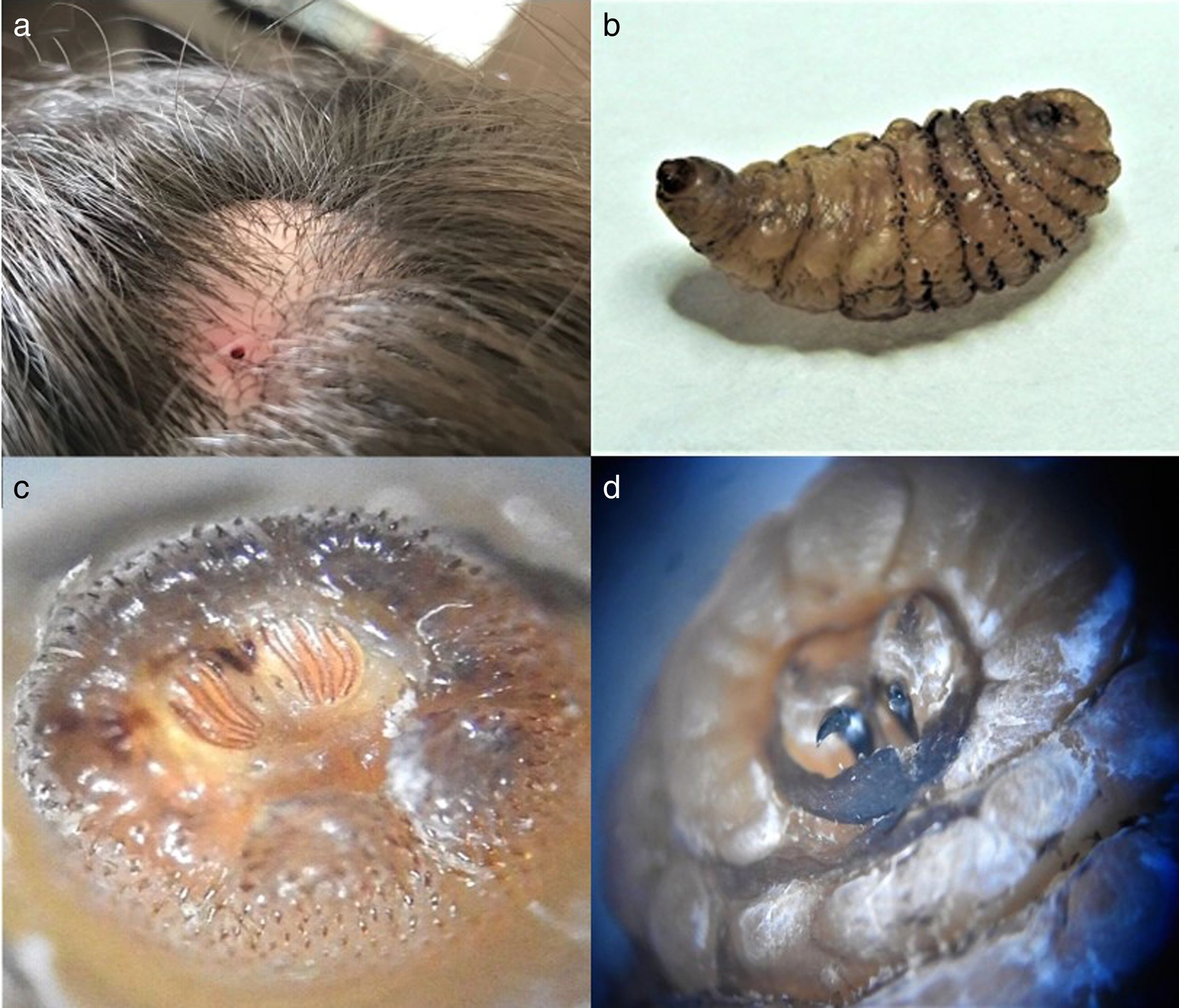
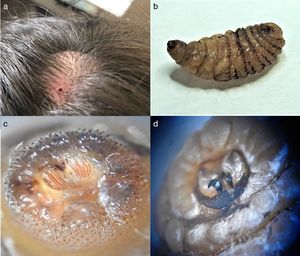
We report the case of a 24-year-old female who presented with a frontal scalp tumor that had grown gradually during the month prior to her admission. She had traveled to Peru a month before and denied fever or other symptoms, except for itching within the lesion. She was assessed by a plastic surgeon showing a lump with a hole which resembled an epidermoid cyst and was scheduled for surgical excision of the mass (Fig. 1a). After incision, a maggot was found (Fig. 1b), and resection was performed without incidents. It was directly sent to the Microbiology Department where it was identified as a Dermatobia hominis larva, based on the characteristics of its posterior spiracle (Fig. 1c), with three spiracular slits, each spiracular plate has three split curves directed toward the belly and slightly toward the middle.1 After extraction, patient was discharged with amoxicilin/clavulanic acid as preemptive treatment of secondary bacterial infection of the wound, presenting no further complications.
Myaisis means invasion of organs and tissues by fly maggots.2 The most common fly species that cause these affection are Cordylobia anthropophaga, original of the African continent, and D. hominis, from Central and South America.3,4 The number of cases of myaisis in countries from continents different to these is increasing due to rise on migration to tropical regions.5 To our knowledge, there are less than 30 cases of myiasis caused by D. hominis reported in Spain.6
D. hominis has three forms on its cycle: adult fly, pupa and larva. Only larvae are parasites,7 and present three different stages. It is interesting that D. hominis is unable of biting because of its poorly developed buccal apparatus. Female adult flies capture hematophagous insects of other species and deposit their eggs on them (around 15–20 eggs at a time).5 As the hematophagous vector bites a mammal, the eggs hatch and larvae fall onto the mammal's skin, where after penetrating and reaching the epidermis, remain growing for 33–41 days. When a 3rd stage larva is under the skin, it fixes its hooks (Fig. 1d) in soft tissue and orientates its respiratory organ, located in its last segment, toward the surface. This respiratory organ is used for species identification,1,4 based on the morphology of this posterior spiracle (peritrem, button and spiracular slit).7
Clinically, in the first 24h, a bug-bite lesion usually appears at the inoculation site, which grows wider and deeper within days, producing pruritus at first and then pain, even referring patients a sense of movement.5 Treatment consists in removal of the maggot. First stage larvae can be removed by expression, but in late stages the tail portion of the larvae is wider than the anterior portion and the presence of spines make the extraction very difficult, resulting in the need of surgical removal.6,8
In conclusion, it is important to report the study of these cases, because of their increasing number, to make an accurate treatment. It is also important to instruct travelers about using protective clothing and insect repellent to prevent possible infestations.
Special thanks to: José Alejandro Rincón Almansa and Javier Pemán García.