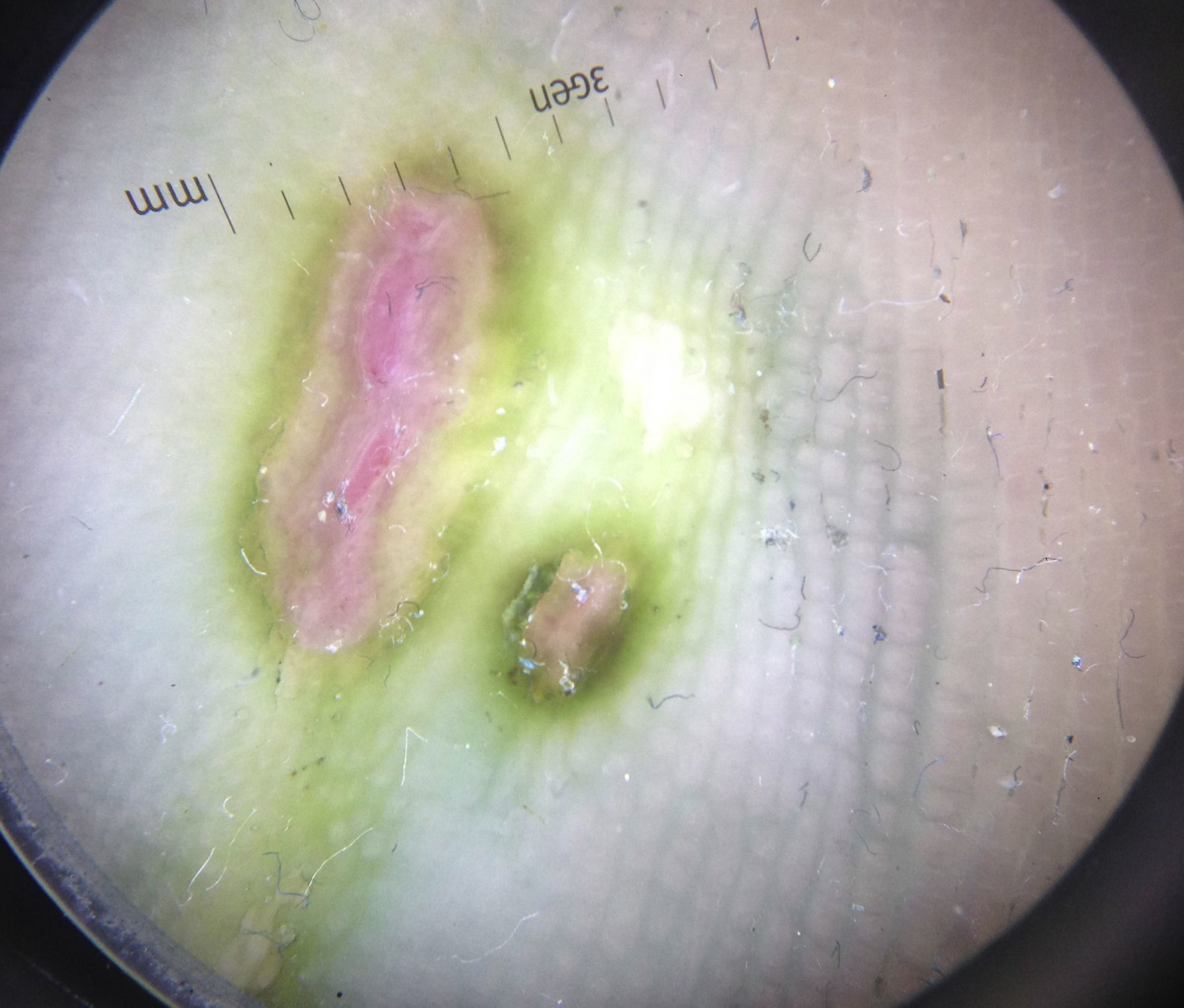
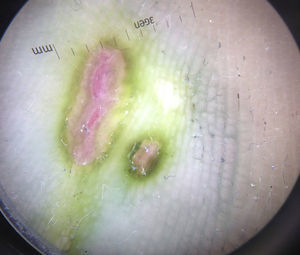
A 49-year-old woman with a history of β-lactam allergy, referred for evaluation of small painful, bilateral and symmetrical ulcers in the anterior plantar region of both feet with one month of evolution. The patient worked in a damp environment and wore rubber boots. She denied having suffered any trauma or injuries to this location. During the examination, 2 small ulcers were observed at the head of the third metatarsal of the right foot and 3 on the left foot (Fig. 1). They had a rounded or ovaloid shape with discharge exuding from the base and a characteristic greenish hyperkeratotic halo. Upon illuminating the ulcers with a Wood lamp, a faint peripheral light green fluorescence was observed. With epiluminescence, we observed an intense greenish colouration around the ulcers and a bluish colouration following a “parallel furrow” and a “lattice-like” pattern (Fig. 2). Samples were collected for culture via a smear of the ulcers on the soles with a sterile swab with medium, and by scraping the scales of the greenish borders.
Clinical courseEmpirical treatment with oral ciprofloxacin was started (250mg/12h, for 2 weeks), also recommending filing of the hyperkeratotic areas and application of 4% acetic acid poultices by immersion for 10min per day. Gram-negative bacilli were isolated in the cultures of both samples, corresponding to Pseudomonas aeruginosa (P. aeruginosa), confirming the diagnosis of ulcerative green foot. Two weeks later, the ulcers had re-epithelialised, although the peripheral green colouration persisted. Based on the culture results and the antibiogram, her primary care physician decided to complete treatment with oral levofloxacin (500mg per day) for 2 weeks, with good tolerance and full resolution of pigmentation and ulcers.
CommentsP. aeruginosa is a motile, strict aerobic gram-negative bacillus that is frequently isolated in damp natural media such as water, soil or plants, as well as in the hospital environment.1P. aeruginosa is responsible for a wide spectrum of skin infections, although they are relatively rare in immunocompetent patients.2–4 In healthy patients, Pseudomonas genus bacteria penetrate the skin via a break in the skin causing: otitis externa (swimmer's ear), paronychia (green nail syndrome), interdigital intertrigo, green foot syndrome,5,6 folliculitis (hot tub folliculitis) and neonatal omphalitis. However, when they affect immunocompromised patients, they can cause potentially serious infections, such as infections of open ulcers or diabetic foot, ecthyma gangrenosum, cellulitis or abscesses, as well as necrotising fasciitis and malignant otitis externa.1,3,7 After reviewing the literature, we have not found references to ulcerative forms of green foot syndrome at the sub-metatarsal level in healthy patients.
The presence of the greenish colouration of any skin lesion should make us suspect the presence of Pseudomonas genus bacteria. Most strains of P. aeruginosa produce pigments, such as pyoverdine and pyocyanin, responsible for the greenish-blue colouration of infected fingernails and the light green fluorescence that they emit under a Wood lamp. However, cultures must be taken and an antibiogram conducted in order to obtain a firm diagnosis. Cultures taken from smears may be contaminated with other skin bacteria,8 therefore scrapings from the keratotic borders in these types of ulcer may increase the specificity of the cultures. Dermatoscopy is not usually used in the diagnosis of pyodermitis. However, it allowed us to observe the presence of an intense green colouration surrounding the ulcer, and a peripheral bluish tint with a defined parallel furrow and lattice-like pattern not visible to the naked eye (Fig. 2).
Treatment of uncomplicated P. aeruginosa infections will be based on the antibiotic therapy selected on the basis of the antibiogram.1 Although controversial, monotherapy is accepted in uncomplicated Pseudomonas skin and soft tissue infections in immunocompetent patients. In this case, we chose quinolones associated with topical antiseptics, such as 4% acetic acid poultices, due to their good bioavailability profile in soft tissues. Just like for interdigital intertrigo, debriding of keratotic borders of these ulcers is recommended.2
Please cite this article as: García-Martínez FJ, López-Martín I, Castellanos-González M, Segurado-Rodríguez MA. Úlceras plantares verdes. Enferm Infecc Microbiol Clin. 2017;35:534–535.