On 27 February 2017, the WHO published the list of the 10 microorganisms resistant to priority antibiotics in the search for therapeutic solutions.1Neisseria gonorrhoeae resistant to cephalosporins and quinolones is one of them. Although the levels of resistance of N.gonorrhoeae to ceftriaxone are still very low in Europe,2 in the article by Fuertes de Vega et al. 9.1% of gonococcal strains isolated from a tertiary hospital in Barcelona were resistant to cefotaxime, and 17.3% were resistant/intermediate to azithromycin.3 The increasing resistance to available antibiotics, along with the delay in the development and marketing of new active antibiotics, have aroused interest in the reintroduction of “old” antibiotics such as fosfomycin.
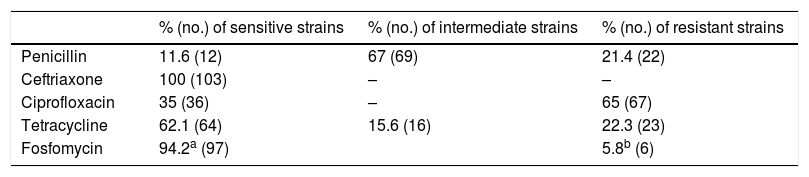
We have studied the sensitivity to fosfomycin of isolated gonococcal strains in patients from five regions of the province of Barcelona: Anoia, Alt Penedès, Garraf, Baix Llobregat and Barcelonès. Strains isolated from urethral (96), vaginal (3), endocervical (2), balano-preputial (1) and semen (1) smears from January 2017 to March 2018 have been prospectively included. Gram staining demonstrated the presence of Gram-negative diplococci in 100/101 samples with staining performed. For the gonococcal isolate, samples were seeded in chocolate agar and Thayer-Martin agar (bioMérieux). The identification of N. gonorrhoeae was done using MALDI-TOF-MS. For the sensitivity study using gradient strips (E-test), the CG II agar medium (Becton Dickinson) was used, adjusting the inoculum to a turbidity equivalent to 0.5 of the McFarland scale in physiological serum. The plates incubated at 35°C, in an atmosphere with 5–7% CO2 for 20–24h before reading. The results were interpreted in accordance with the cut-off value of the European Committee on Antimicrobial Susceptibility Testing (EUCAST), Version 8.1, 2018-05-15, for enterobacteria. No isolate showed resistance to ceftriaxone, but the rest of the antibiotics tested did (Table 1). The molecular detection of Chlamydia trachomatis and N. gonorrhoeae was performed in 48 patients with positive culture, being positive for gonococcus in all cases, highlighting an excellent sensitivity of the molecular method compared to the culture. Coinfection with C. trachomatis was detected in 11/48 cases (22.9%). The high percentage of coinfections with chlamydia confirms the need to add the second antibiotic to the treatment with fosfomycin in the case of suspected gonococcal urethritis.
Antibiotic sensitivity in N. gonorrhoeae.
Over time N. gonorrhoeae has been acquiring resistance to the main antibiotics used.4 Currently, the recommended treatment is the combination of ceftriaxone with azithromycin.5 The emergence of strains resistant to third-generation cephalosporins, or even to the combination of two drugs, has raised alerts about encountering cases of intractable gonorrhoea. The fosfomycin used in the past as an alternative to treatment6 allows better bioavailability of the drug with its current formulations. In their study, Yuan et al. demonstrated non-inferiority between the fosfomycin trometamol regimen 3g daily on days 1, 3 and 5 compared to ceftriaxone plus azithromycin.7 Most of the strains in our study presented an MIC≤32μg/ml for fosfomycin, sensitivity cut-off value proposed for other microorganisms by EUCAST. If we consider the sensitivity according to the cut-off values of the Clinical and Laboratory Standards Institute (sensitive≤64mg/l, intermediate=128mg/l and resistant≥256mg/l), only one strain was resistant and one presented intermediate sensitivity. Despite its effectiveness in monotherapy, fosfomycin is more likely to be used in combination therapy. Barbee et al. studied the combination of ceftriaxone with fosfomycin, and although there is no synergy, a lower fractional inhibitory concentration index (0.96) has been observed compared to other combinations studied.8 Another study also showed no synergy of the combinations of fosfomycin with azithromycin or ceftriaxone.9 Further studies are needed to ensure adequate concentrations of fosfomycin at the site of infection. Recently, Wijma et al. have shown significant variability in the pharmacokinetics of fosfomycin among healthy volunteers, which could explain therapeutic failures of uncomplicated UTI treatment with the recommended regimen of 3g of oral fosfomycin in a single dose.10 Even so, the available data position fosfomycin as a promising therapeutic alternative for uncomplicated cases of genital location.
Please cite this article as: Zboromyrska Y, Guerrero-Torres MD, Benítez MÁ. ¿Es la fosfomicina una buena alternativa terapéutica para la gonorrea en nuestro medio? Enferm Infecc Microbiol Clin. 2019;2020:38–39.