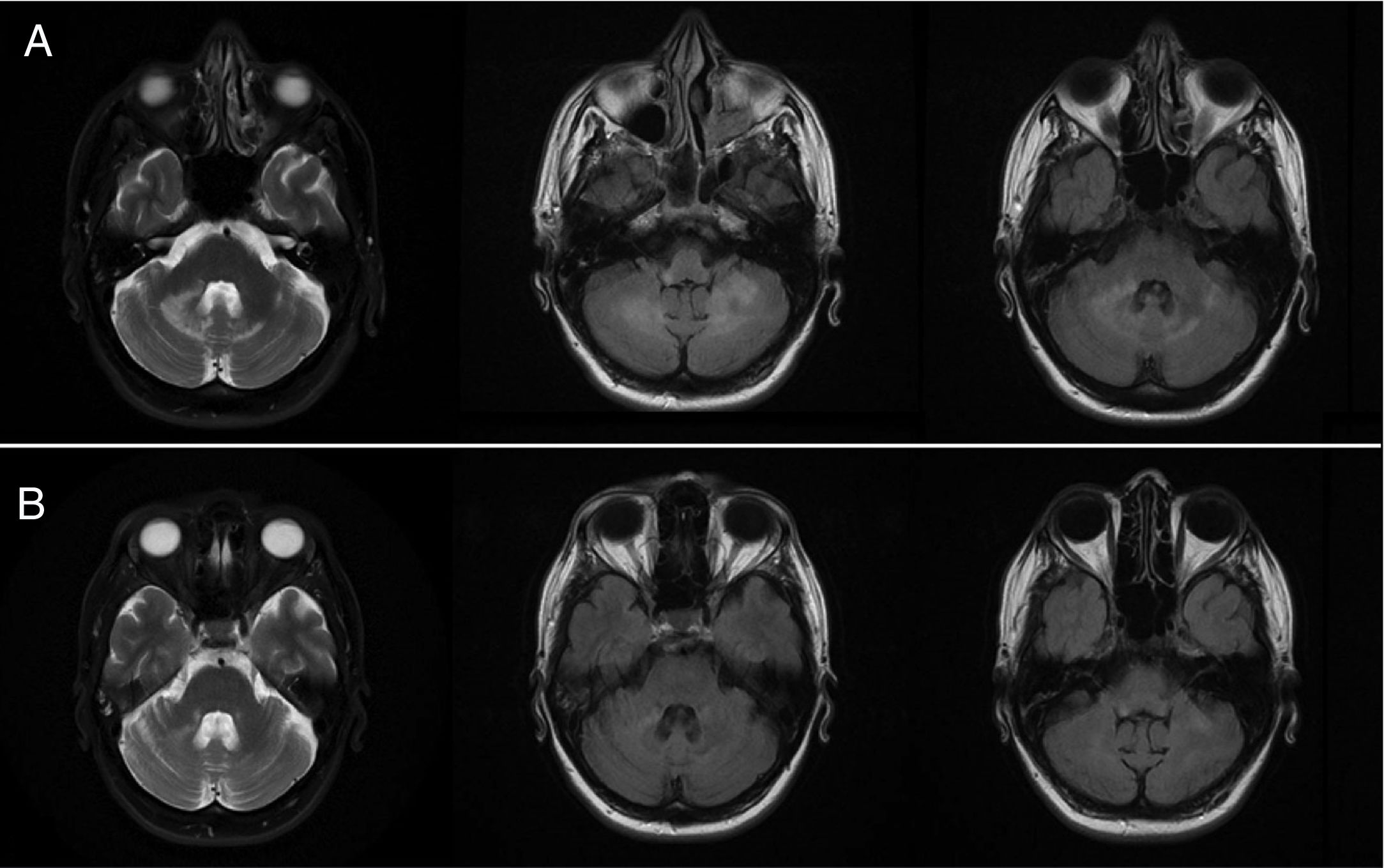
A 44-year-old woman, a former parenteral drug user, with human immunodeficiency virus (HIV) infection for the past 19 years, severe immunosuppression despite good virological control (RNA < 20 copies/mL, 120 CD4+/mm3, CD4+ 10%, CD4+/CD8+ ratio 0.20), and concomitant infection with HBV (HBsAg negative), being treated with tenofovir alafenamide + emtricitabine + darunavir/cobicistat (TAF + FTC + DRV/c) in a single pill and prophylaxis with cotrimoxazole, with negative HCV serology and RNA. She was admitted to our hospital due to worsening signs and symptoms for the past month of dysarthria, ataxia, limb dysmetria, intention tremor, right leg paresis (RLP) and right homonymous hemianopia. A CT scan showed left parieto-occipital hypodensity suggestive of encephalomalacia due to prior ischemic injury, and hypodensitity of periventricular white matter suggestive of small-vessel ischemic disease. A lumbar puncture was performed and the CSF sample taken showed normal clinical chemistry characteristics. An MRI of the brain showed evidence of cerebellitis with increased signal in diffusion and long TR sequences in white matter and hypointensity in T1, which did not enhance following contrast (Fig. 1A).
The suspicion of progressive multifocal leukoencephalopathy (PML) was confirmed by JC virus PCR detection in positive CSF, with a viral load (VL) for HIV in CSF < 20 copies/mL. Multiple PCR for other pathogens, culture and onconeural antibodies in CSF were negative. No risk factors for developing PML other than severe immunosuppression due to HIV infection were detected in the patient.
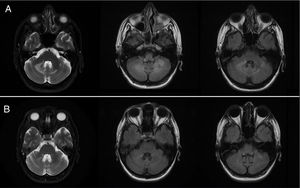
With approval for off-label use, treatment was started with pembrolizumab. The patient received 3 doses of 2 mg/kg of body weight 4 weeks apart, with excellent tolerance and without showing any clinical or laboratory abnormalities that could be attributed to the treatment. JC virus PCR detection in CSF became negative 4 weeks after the first dose, and the patient showed gradual improvement in terms of ataxia, strength, and stability of dysarthria, and radiological improvement 3 months after the last dose (Fig. 1B), with JC virus PCR detection in CSF remaining negative. The VL of HIV in CSF and in plasma was always <20 copies/mL, and there was no immune reconstitution; 3 months after the last dose, the patient presented 150 CD4+/mm3, CD4+ 9.1%, and CD4+/CD8+ ratio 0.18. Therefore, we attributed her improvement to treatment with pembrolizumab.
PML is an opportunistic central nervous system infection caused by the JC virus that almost exclusively affects people with cellular immunosuppression. It is characterized by progressive multifocal impairment of white matter. Restoration of immunity may lead to an immune reconstitution syndrome known as inflammatory PML, which features initial clinical worsening and contrast uptake by lesions on MRI.1
In the presence of a clinically and radiologically consistent syndrome, the gold standard for diagnosis is brain biopsy, although, given its high rates of morbidity and mortality, JC virus PCR detection in CSF is used in its stead, despite its lower sensitivity. In fact, negative PCR results are often found in patients with AIDS who start antiretroviral treatment (ART). These patients should be considered to have “potential PML,” after other entities such as primary central nervous system lymphoma, encephalopathy due to HIV, and toxoplasmosis have been duly ruled out. In cases with clinical and radiological characteristics consistent with PML, but with negative PCR, it is suggested that PCR be repeated in CSF and that biopsy be reserved for cases in which repeat PCR is negative.1
The mainstay of treatment is restoration of immunity with ART or suspension of immunosuppressants. Up to now, other treatments have achieved limited success, with anecdotal evidence of efficacy, but without evidence of a clinical benefit in randomized trials or prospective studies, or with poorly tolerated adverse effects. Today, the following are not considered to be effective treatments: cytarabine, cidofovir, topotecan, mirtazapine, mefloquin, maraviroc, interleukin-7, and virus-specific T-cell therapy.2 As a new development, in several recently published studies on a total of 10 patients with PML, treatment with immune checkpoint inhibitors, pembrolizumab or nivolumab (monoclonal antibodies that block programmed cell death protein 1 [PD-1]), was associated with clinical improvement or stabilization in 7 of the 10 patients.3–5 However, cases of PML following treatment with nivolumab have been reported.6
In the largest of those studies,3 8 adults with PML received one to 3 doses of pembrolizumab 2 mg/kg every 4–6 weeks. This treatment reduced PD-1 expression in lymphocytes in blood and CSF in all 8 patients. Five of them improved or stabilized clinically, showing a decrease in the VL of the JC virus in CSF and an increase in CD4+ and CD8+ cells with anti-JC activity. In the other 3 patients no significant change was observed in terms of VL or magnitude of antiviral immune response, and there was no clinical improvement.
FundingWe did not receive funding of any kind for this purpose.
We would like to thank the Pharmacy and Neurology Departments at the hospital for their assistance with patient management.
Please cite this article as: Mozo Ruiz M, Rosado Barrasa N, Tena Gómez D, Torralba González de Suso M. Tratamiento con pembrolizumab en paciente con infección por virus de la inmunodeficiencia humana y leucoencefalopatía multifocal progresiva. Enferm Infecc Microbiol Clin. 2020;38:396–397.