A 61-year-old patient visited the emergency department due to pain in the right eye following entry by a foreign body a week earlier while working outdoors. Her medical history with regard to ophthalmology included a diagnosis of bilateral diabetic retinopathy being treated with intravitreal antiangiogenic therapy and chronic simple glaucoma being managed with topical treatment.
Examination revealed a paracentral corneal ulcer after 8 h, with satellite stromal infiltrates. It was labeled infectious keratitis, a sample of corneal exudate was taken for culture, the patient was prescribed treatment with tobramycin (3 mg/mL, 1 drop/6 h) and moxifloxacin (5 mg/mL, 1 drop/12 h), and a follow-up appointment was scheduled. The patient returned after 48 h; no improvement was observed, and the exudate culture was negative. Treatment was started with corticosteroids, a cycloplegic, fortified vancomycin eye drops (25 mg/mL, 1 drop/4 h), and ceftazidime 5% (50 mg/mL, 1 drop/4 h), and, given the suspicion of fungal keratitis, the patient was prescribed topical voriconazole (10 mg/mL, 1 drop/2–4−6 h in a tapering regimen for 5 days at each dosage). After two weeks, the patient still did not show a satisfactory response; her ulcer had become larger, the infiltrate had become deeper, and her stromal and endothelial edema had increased; therefore, she was scheduled for penetrating keratoplasty. During the operation, fluid, stroma, and corneal scraping samples were taken and sent to the Microbiology laboratory. The patient stayed on the same treatment for 3 months following the operation and showed gradual improvement in the appearance of the graft and complete epithelialization. In the last examination performed 8 months after keratoplasty, she continued to follow a good clinical course with visual acuity of 0.500 with correction.
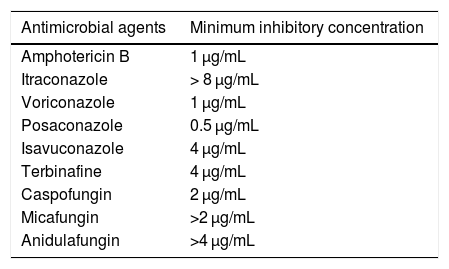
A filamentous fungus was isolated in the corneal scraping culture; all the other cultures were negative. This fungus was sent to the Spanish National Center for Microbiology, where it was identified by molecular methods using sequencing of the internal transcribed spacer region according to the previously described procedure.1 The strain was molecularly identified as Albifimbria verrucaria (A. verrucaria) (Genbank access no.: MK946705) with a percentage of similarity of 99.9% to the internal transcribed spacer sequence of the A. verrucaria type strain (KU845893). A sensitivity test was performed according to the recommendations of the European Committee on Antimicrobial Susceptibility Testing (EUCAST).2Table 1 shows the results of the antifungigram. As there are no established cut-off points, minimum inhibitory concentrations cannot be interpreted.
Sensitivity test for Albifimbria verrucaria isolate.
| Antimicrobial agents | Minimum inhibitory concentration |
|---|---|
| Amphotericin B | 1 μg/mL |
| Itraconazole | > 8 μg/mL |
| Voriconazole | 1 μg/mL |
| Posaconazole | 0.5 μg/mL |
| Isavuconazole | 4 μg/mL |
| Terbinafine | 4 μg/mL |
| Caspofungin | 2 μg/mL |
| Micafungin | >2 μg/mL |
| Anidulafungin | >4 μg/mL |
A. verrucaria, formerly called Myrothecium verrucaria, is a saprophytic fungus with a global distribution that inhabits both soil and decomposing plant matter.3 It is a fungus with significant phytopathogenic activity,3 having recently been identified in two cases of fungal keratitis.4,5 Refojo et al.5 analyzed 157 cases of keratitis and identified one case due to Myrothecium spp. Similarly, Rameshkumar et al.4 reported a case of keratitis due to M. verrucaria in which the patient did not respond to topical treatment with natamycin (5%) and voriconazole (1%) and had to undergo keroplasty. None of the studies analyzed clinical course or antifungigram results.
A. verrucaria can synthesize a number of mycotoxins, such as trichothocenes,3 which are capable of a exerting a cytotic effect on animal cells such that they may interfere with protein synthesis, the immune system, and alveolar macrophages.6 Trichothocenes have been shown to inhibit protein synthesis in eukaryotic cells by binding to ribosomal subunit 60S and interacting with a particular enzyme, peptidyltransferase.7
Species belonging to the genus Albifimbria are characterized by a lack of sporulation and slow growth in culture media.4 This renders conventional microbiological diagnosis difficult and requires resorting to molecular biology techniques. Management of these types of infection involves application of topical antifungals (natamycin or voriconazole); surgery is necessary in cases in which there is no response to treatment.4 Therefore, in cases of lacerating and/or penetrating eye injuries caused by plant matter or similar, fungal infection should always be considered. In addition, given the diagnostic difficulty associated with some species of filamentous fungi, in cases of clinically and microbiological demonstrated fungal infection, it is advisable to perform identification and a sensitivity study at a reference center, which in Spain would be the Spanish National Microbiology Center.
Please cite this article as: Moreno-Flores A, Álvarez-Reguera A, Álvarez-Fernández M, Alastruey-Izquierdo A. Queratitis por Albifimbria verrucaria: a propósito de un caso. Enferm Infecc Microbiol Clin. 2020;38:398–399.