Liver abscess is an uncommon disease whose incidence varies by series and geographic area from 2 to 20 cases per 100,000 hospital admissions.1 In Spain, the most common etiology is bacterial.2 Polybacterial etiology is relatively common and accounts for 13% of all visceral abscesses.
We present the case of a 78-year-old male with a history of hypertension, dyslipidemia, and abnormal baseline glycemia with a previous aortocoronary bypass. In the prior weeks, with no clear temporal relationship to his having had a colonoscopy, he presented feverishness, weight loss, and pain in the right shoulder. Following successive tests (CT scanning of the chest and abdomen), he was ultimately hospitalized in the General Surgery Department, as a supcapsular liver lesion at the level of the hepatic dome (segment IV-A), poorly defined on CT despite contrast, oval in shape, and having a maximum diameter of 56 mm was documented. Moreover, this lesion was found to be connected to a lobed collection whose walls exhibited hyperuptake between the anterior half of the diaphragm and the diaphragm surface. Laboratory testing on admission revealed leukocytosis with left shift, normal coagulation testing, and clinical chemistry with a modest elevation in alkaline phosphatase (147 U/l; reference range 38–126) with elevated acute-phase reactants. Emergency surgery was indicated to clean and drain the diaphragm. Matter with a firm consistency and an appearance not consistent with a tumor or pyogen was obtained, whereupon assessment by the Internal Medicine Department was ordered.
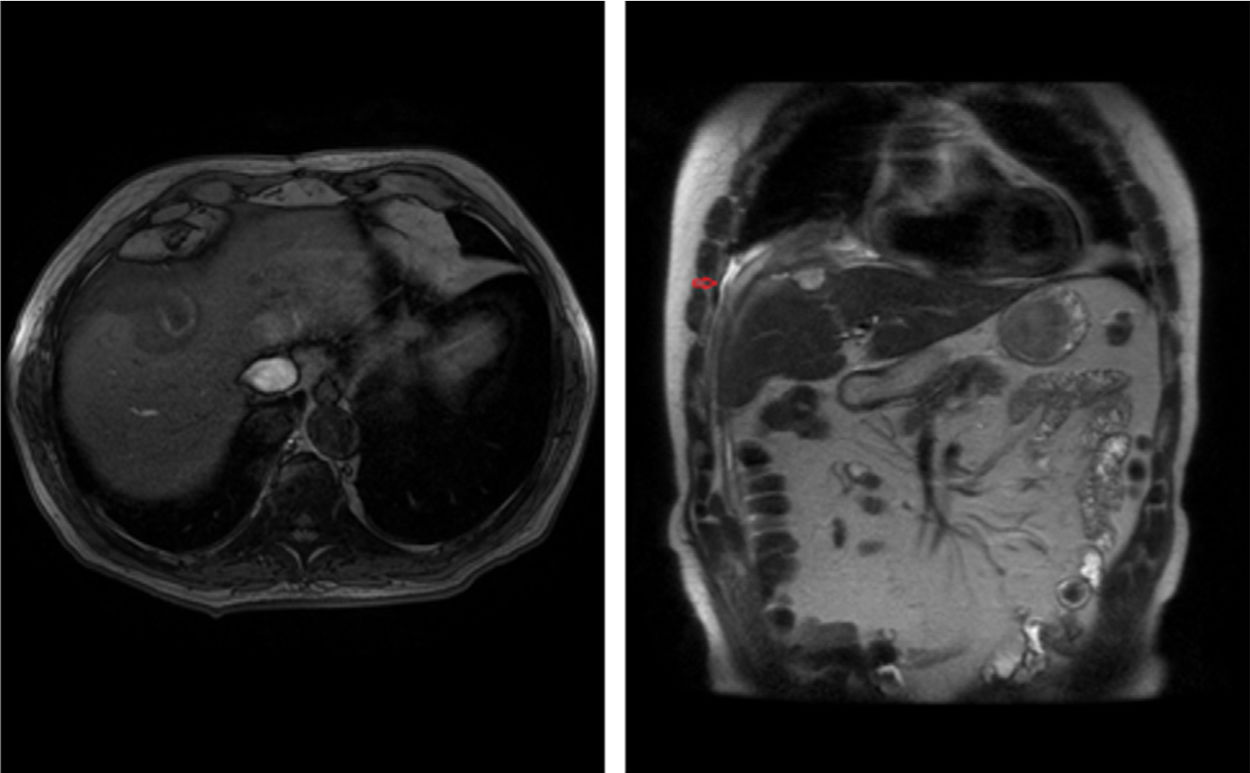
Culture of the matter obtained was found to be sterile, as were blood cultures and tests of feces and matter obtained through postoperative drainage; all autoimmunity determinations were negative. Pathology testing of the lesion revealed inflammation with plasma cells, eosinophils, cholangitis, and presence of granulomas. Accordingly, a battery of serology tests (successively, Toxocara spp., Trichinella spiralis, Fasciola hepatica, Echinococcus granulosus, Enthamoeba histolytica, Anisakis, and Toxoplasma) was indicated and demonstrated positivity for Toxocara by ELISA. Finally, liver-specific MRI demonstrated a hyperintense oval-shaped lesion in a T1 sequence3 without intravenous contrast and an inflammatory fistula tract in a T2 sequence corresponding to the postoperative drainage tract (Figure 1). Immunoglobulin E levels were ordered once after steroid treatment was started and came back normal. Serial Toxocara was not deemed useful. The fundus of the eye was normal.
Several characteristics led to suspicion of a parasitic origin. From a clinical point of view, the patient had few symptoms, with very modest abnormality in his liver function tests4,5 and no eosinophilia6 seen in the course of his disease.7 He sometimes lived with a dog and had a potential epidemiological history in relation to consumption of cow and pig liver, as well as products of pig slaughtering in a social context. Regarding his imaging tests, the oval appearance and the poorly defined capsule on both MRI and CT were consistent with visceral larva migrans, T1 hyperintensity on MRI being characteristic.3 Although its typical size is around a centimetre,8 lesions of a larger size and a cystic appearance due to confluence9 considering the migration of the parasite through the liver parenchyma have been reported. The patient's histology results ruled out gallbladder neoplasm, liver neoplasm, primary biliary cirrhosis, and IgG4-related disease. The patient's levels of eosinophils, histiocytes and plasma cells invited suspicion of a parasitic origin, although the discovery of larvae in such lesions is rare9 given their brief life cycle lasting just a few weeks. Finally, the inflammatory appearance of the fistula tract originating from surgical drainage supported suspicion of parasitic infestation as parasites leave a trail of glycosylated proteins in their path.10 For all these reasons, we considered the fact that the patient had undergone a colonoscopy a few weeks earlier to be anecdotal.
Due to our lack of experience, the patient received treatment with albendazole for several months along with steroids in a tapering regimen, with a favorable clinical course: 3 years after finishing treatment, he presented a residual lesion on MRI and a persistent lack of symptoms.
Please cite this article as: Bernardo-Cofiño J, Gómez-Illán R, Riera Lavilla L, Asensio Fierro F. Larva visceral migrans secundaria a Toxocara en paciente anciano. Enferm Infecc Microbiol Clin. 2020;38:400–401.