Ciprofloxacin, a quinolone, is widely used in clinical practice. The most common adverse effects are gastrointestinal disorders (nausea and vomiting) and central nervous system abnormalities.1,2 Renal failure (RF) secondary to this drug is a rare adverse effect (<1/10,000 to <1/1000) indicated in its summary of product characteristics.3 Several cases have been reported in the literature on RF due to interstitial nephritis (IN)4,5 as well as crystal precipitation in the kidney tubules.6–11 We present the case of a patient with RF without oliguria or evidence of rhabdomyolysis attributed to ciprofloxacin.
Our patient was a 76-year-old man and a former smoker with no known drug allergies. He had a medical history of hypertension, aortic stenosis with mechanical valve implantation and atrial fibrillation, stable stage 2 chronic kidney disease and severe chronic obstructive pulmonary disease (COPD) with multiple admissions. His baseline treatment consisted of warfarin, pravastatin, azithromycin, paracetamol, amiodarone, furosemide, enalapril, bisoprolol, hydralazine, umeclidinium/vilanterol/fluticasone, and calcium/vitamin D3. The patient had come in several times in the past year due to decompensation of his heart failure (HF) and COPD. He required admission due to decompensation of his HF and feverishness for 4 days. Blood cultures were performed and came back negative. Given the patient's increased expectoration with changes in purulence, a sputum culture was performed and came back positive for Pseudomonas aeruginosa. In view of this initial isolation and clinical stability, treatment was started with ciprofloxacin 750 mg every 12 h for 21 days, and the patient was discharged the day after said treatment was started. No other new treatment was started at discharge; the patient continued to take his baseline medication.
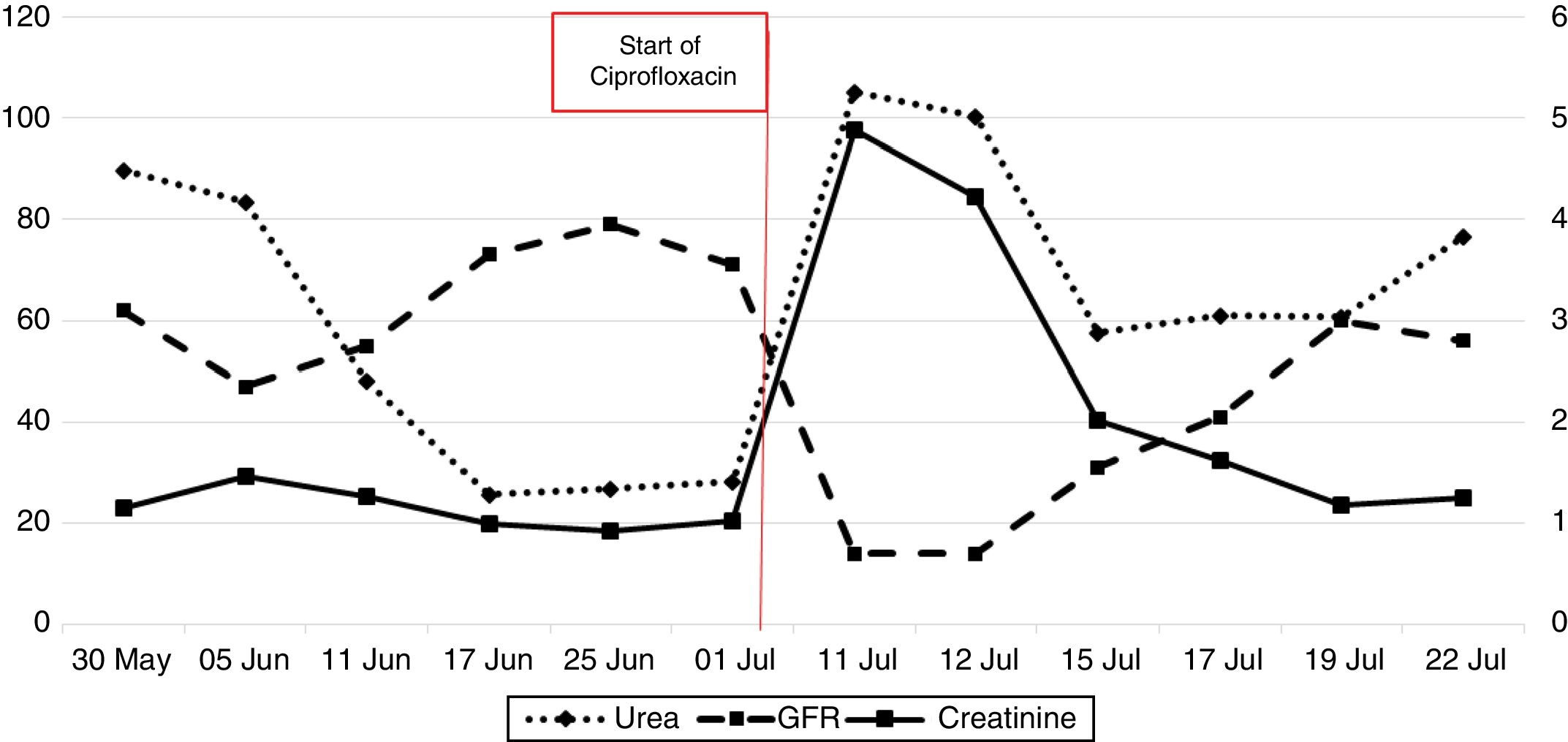
After 9 days, the patient returned due to clinical worsening. Laboratory testing showed: urea 105 mg/dl, creatinine 4.80 mg/dl, estimated glomerular filtration rate (GFR) according to CKP-EPI < 15 mL/min/1.73 m2, C-reactive protein 0.73 mg/dl, and hemoglobin 10.9 g/dl, with all other values within normal limits. Prior laboratory testing had shown urea 28.2 mg/dl, creatinine 1.02 mg/dl, and estimated GFR 71 mL/min/1.73 m2. Given the suspicion of acute RF according to the RIFLE system,11 a kidney ultrasound was performed, which ruled out an obstructive cause, and urine sediment testing was performed, which came back normal, with a pH of 8 (reference range 5–8). Therefore, it was decided to admit the patient with serum therapy, bladder catheterization, and strict urine output monitoring. As ciprofloxacin was suspected as a cause of RF, a decision was made to stop that antibiotic and continue treatment with intravenous ceftazidime. The patient followed a satisfactory clinical course, recovering near-usual laboratory values after 10 days, with urea 76.6 mg/dl, creatinine 1.25 mg/dl and GFR 56 mL/min/1.73 m.2
Community-acquired acute RF is due to prerenal causes in 70% of cases and obstructive causes in 17% of cases.12,13 The most common causes of acute RF are kidney hypoperfusion and toxins such as antibiotics and iodinated contrasts.
Ciprofloxacin can be a cause of acute RF. In a review of the literature with a PubMed search using the terms "ciprofloxacin induced acute renal failure," we found 33 references, the earliest from 1987. Cases of acute IN due to ciprofloxacin have been reported,4,5 this being the main etiology of RF due to this drug. It has been reported both in patients with a drug overdose14 and in patients using regular therapeutic doses. IN is usually due to drugs such as antibiotics and non-steroidal anti-inflammatory drugs, and is characterized by skin rash, eosinophilia and eosinophiluria; these findings are inconsistent, but if they are present, they aid in diagnosis. Histological confirmation by renal biopsy shows an interstitial inflammatory infiltrate believed to be due to an immunoallergic process rather than a toxic effect.
Another less common cause of RF due to ciprofloxacin is crystal nephropathy. At present, there are 5 references on this complication in the literature6–11 (according to a PubMed search using the terms "ciprofloxacin and crystal nephropathy"). It presents with RF with elevated levels of creatinine and urea, with neither oliguria nor laboratory signs of rhabdomyolysis. The presence of acidified urine (pH < 6) in affected patients has been reported. Crystals can be visualized in both histology and urine sediment. The treatment used to reverse this condition is suspension of the drug and initiation of conservative treatment with serum therapy; in most cases, this achieves resolution and a return to baseline laboratory values between the first and the second week.
In our case, creatinine and urea increased without eosinophilia, with diuresis maintained (Figure 1). The condition could not be confirmed by histology, nor could crystals be seen in sediment; however, the patient's urinary alkalosis and his laboratory and clinical course were consistent with the few cases in the literature of RF secondary to ciprofloxacin crystal precipitation. Using a causality algorithm from Naranjo et al.,15 we obtained a score of 6, corresponding to a probable adverse drug reaction; hence, the case was reported through the pharmacovigilance system.
Please cite this article as: Martin M, Boixeda R, Muñoz A, Felip À. Ciprofloxacino como causa de insuficiencia renal aguda. Enferm Infecc Microbiol Clin. 2020;38:402–403.