To assess HAV serologic and vaccination status among people who live with HIV (PLWH), and to evaluate the impact of a vaccination-based strategy on HAV-negative patients in Seville, Spain.
MethodsStudy with two time-overlapping phases: (i) cross-sectional study of HAV immunity prevalence among PLWH followed at a Spanish hospital between August 2019 and March 2020. (ii) Patients seronegative for HAV, reliably unvaccinated were included in a before-and-after quasi-experimental study, with an intervention focused on HAV vaccination according to national recommendations in force.
ResultsSix hundred and fifty-six patients were included, of which 111 [17%, 95% confidence interval (95% CI) 14–20%] were seronegative for HAV. Of these, 48 [43% (95% CI, 34–53%)] individuals were MSM. The absence of HAV immunity was attributed in 69 [62% (95% CI, 52–71%)] patients to non-referral to vaccination, followed by lack of achievement of a correct vaccination scheme [n=26; 23% (95% CI, 16–32%)]. After the program implementation, 96 [15% (95% CI, 12–18%)] individuals were seronegative (17% vs. 15%, p=0.256), of whom 42 [41% (95% CI, 32–51%)] were MSM. The absence of immunity after the intervention was mainly attributed to: adherence failure in 23 [24.0% (95% CI, 15.8–33.7%)] patients, on-course immunization scheme in 34 [33% (95% CI, 24–43%)] individuals and pending appointment at the vaccine delivery unit in 20 [20.8% (95% CI, 13.2–30.3%)] patients.
ConclusionsA sizeable proportion of PLWH remains susceptible for HAV infection in future outbreaks. A program based on referral to the vaccine delivery unit yields poor results, largely due to program adherence failures. New strategies are needed to increase HAV vaccination coverage.
Evaluar la prevalencia de inmunidad frente al VHA en personas que viven con VIH así como el impacto de una intervención basada en la vacunación de pacientes seronegativos frente al VHA.
MétodosEstudio con dos fases solapadas en el tiempo: 1) transversal de prevalencia de inmunidad frente al VHA en personas que viven con VIH seguidas en un hospital de tercer nivel, entre agosto de 2019 y el inicio de las medidas nacionales de contención de la epidemia por SARS-CoV-2, marzo de 2020. 2) Cuasiexperimental, con una intervención centrada en la vacunación frente a VHA de pacientes seronegativos, en la unidad responsable de esta.
ResultadosCiento once (17%, [95% IC, 14-20%]) de los 656 pacientes incluidos eran seronegativos frente al VHA. Las principales causas de la ausencia de inmunidad fueron: 69 (62% [95% IC, 52-71%]) individuos no derivados a la unidad responsable de la vacunación; 26 pacientes (23% [95% CI, 16-32%]) no completaron el esquema vacunal. Tras la intervención, 96 (15% [95% IC, 12-18%]) pacientes continuaron siendo seronegativos frente al VHA (comparada con la prevalencia basal, p=0,256), 42 (18% [95% IC, 13-23%]) eran HSH. Las principales causas de la ausencia de inmunidad fueron: 26 (23% [95% IC, 15-32%]) individuos presentaron fallos de adherencia al circuito vacunal; 34 (33% [95% IC, 24-43%]) pacientes habían recibido una sola dosis; 22 (22% [95% IC, 14-31%]) seguían sin una primera valoración por parte de la unidad responsable de la vacunación.
ConclusionesUna proporción considerable de personas que viven con VIH, particularmente HSH, sigue siendo susceptible a la infección por VHA. La derivación sistemática a la unidad responsable de la vacunación se traduce en modestos incrementos de la prevalencia de inmunidad. Son necesarias nuevas estrategias para aumentar la cobertura vacunal.
Hepatitis A virus (HAV) is one of the leading causes of acute hepatitis. In the majority of European Union/European Economic Area (EU/EEA) countries, decreased in HAV circulation in the past decades has resulted in a significant proportion of individuals without immunity following natural infection and then susceptible to HAV infection.1 Likewise, the incidence of hepatitis A in Spain remains low and steady.2 However, periodic HAV outbreaks arise periodically, particularly affecting men who have sex with men (MSM), most of them living with HIV. In this respect, between 2016 and 2017 a large hepatitis A epidemic occurred across EU/EEA. Spain was one of the most struck countries, accounting for over 50% of HAV infections.3 In this subset, MSM were disproportionately affected and nearly half of the individuals with available HIV status data were living with HIV.3 Moreover, the majority of individuals who acquired HAV infection during this EU/EEA outbreak had not been previously vaccinated against HAV.3 In addition to that, health costs associated to HAV outbreaks are not negligible. Although HAV-related mortality is rare, morbidity due to HAV infection is significant, especially for the adult population.4 In this sense, between January and June 2017, only in Barcelona, 39% of the reported HAV infected individuals were admitted in hospital facilities.5 Besides, indirect costs linked to work absenteeism should not be underestimated.
In the vast majority of countries of the EU/EEA, universal HAV vaccination has not been adopted and is only currently recommended for high-risk groups. Thus, HAV immunization among MSM is commonly advised. However, as of February 2020, very few countries also recommend and cover HAV vaccination among people living with HIV (PLWH), such as Spain.6 Among PLWH with good immunological status, HAV vaccination with two standard doses achieves seroconversion rates above 90%.7,8 Consequently, lack of HAV immunity is the main cause of HAV outbreaks.9 Hence, current pockets of susceptible individuals along with environmental and behavioral risk factors may be determinant for new epidemics. However, HAV seroepidemiological data among PLWH are scarce and most of the studies which assessed HAV immunity prevalence are outdated and might not be reflecting the current situation.10–18 Besides, information on HAV vaccine coverage for PLWH is lacking and HAV vaccination programs outcomes remain unknown in real-life interepidemic conditions.
Therefore, the aims of this study were, firstly, to assess HAV serologic status among PLWH in Seville, Southern Spain, and, secondly, to evaluate the impact of a vaccination-based intervention among HAV-seronegative PLWH.
MethodsStudy design and patientsThis was a two-step study with overlapping phases. Firstly, a cross-sectional study of HAV immunity prevalence among PLWH was carried out. All consecutive PLWH, with active follow-up in a Unit of Infectious Diseases at a University Hospital in Spain, seen from August 1st 2019 to March 15th 2020, were included. At the same time, PLWH seronegative for HAV were recruited in a quasi-experimental study (pre-test and post-test design) with an intervention focused on vaccine delivery. All participants were evaluated at least every six months in accordance with national protocols for the monitoring of PLWH, until the end of the study (October 31st, 2020).19
Intervention: HAV vaccinationThe first pre-scheduled HIV follow-up visit of each patient during the study period was considered the baseline time-point. At the time of the enrollment, HAV serological status and HAV vaccination history of all patients were assessed, based on the information collected in the electronic health record. Among individuals seronegative for HAV, without previous HAV vaccination according to the national recommendations in force,20 HAV immunization was indicated. As in the vast majority of Spanish health facilities, vaccination among PLWH was managed by the Preventive Medicine Unit at the same Hospital. In accordance with the latest recommendations of the National Health Department, individuals received 2 or 3 doses of monovalent HAV vaccine (HAVRIX® 1440 SI, GlaxoSmithKline, United Kingdom) based on CD4+ cell count: if it was higher than 350cells/mm3, they received 2 doses separated by 6 months. On the contrary, if CD4+ cell count was below this figure, 3 doses provisions were scheduled at 0–1–6 months. In order to assess the serological response to the vaccine, HAV serology was performed one month after receiving the last dose. Response to HAV vaccination was considered for a HAV antibodies (anti-HAV) titer above 20SI/ml. The causes for the non-detection of anti-HAV were investigated before and after program implementation by checking electronic medical records.
Outcomes and definitionsThe main outcome of this study was the presence of specific anti-HAV in serum above 20SI/ml. HAV seropositive patients were defined as individuals with anti-HAV titer above this cut-off. All HAV seropositive participants were considered immune against HAV infection. Anti-HAV were measured using a commercial bioluminescence immunoassay with Elecsys anti-HAVII kits (Roche Diagnostics, Rotkreuz, Switzerland) according to manufacturer's specifications.
Statistical analysisFirstly, descriptive analyses were performed. Continuous variables were expressed as median (Q1–Q3) and categorical variables as frequencies (percentage). Prevalence of HAV-seronegative individuals was estimated by dividing the number of non-immune patients by the total number of patients. Similarly, the proportions of patients referred to Preventive Medicine, the percentage of individuals vaccinated against HAV during the study period and the prevalence of HAV immunity after the intervention were assessed. All point estimates are provided along with exact Clopper–Pearson 95% confidence interval (95% CI). The χ2 test or Fisher's exact test were used to compare the distribution of categorical variables. These analyses were carried out using the SPSS software 25.0 (IBM Corporation, Somers, New York, New York, USA).
EthicsThis study was conducted according to the Helsinki declaration and was approved by the Ethics Committee of the Hospital Universitario de Valme. Informed consent was obtained from all individuals.
ResultsCharacteristics of the study populationSix hundred and fifty-six patients were included in this study. The main characteristics of the study population are depicted in Table 1. Three hundred and fifty-eight (54.6%) individuals had acquired HIV infection through sexual intercourse. All patients were receiving antiretroviral therapy. Five hundred and fifty-one patients (83.9%) showed CD4+ cell count at baseline higher than 350cells/mm3.
Main characteristics of the study population (N=656).
| Parameter | n (%) |
|---|---|
| Male sex | 543 (82.8) |
| Age, years* | 51 (42–56) |
| Risk factors for HIV infection | |
| PWID | 263 (40.1) |
| MSM | 243 (37) |
| Sexual transmission non-MSM | 115 (17.5) |
| Other | 6 (0.9) |
| Unknown | 29 (4.4) |
| Positive anti-HCV | 296 (45.1) |
| Positive HBsAg | 12 (1.8) |
| Baseline HIV viral load<50cp/ml | 614 (93.6) |
| CD4+ cell count (cells/mm3)* | 670 (445–868) |
Data are number (%) of participants. Continuous variables (indicated with*) are reported as median (quartile 1–quartile 3).
Abbreviations: HIV: human immunodeficiency virus; PWID: people who inject drugs; MSM: men who have sex with men; anti-HCV: hepatitis C virus antibodies; HBsAg: hepatitis B surface antigen.
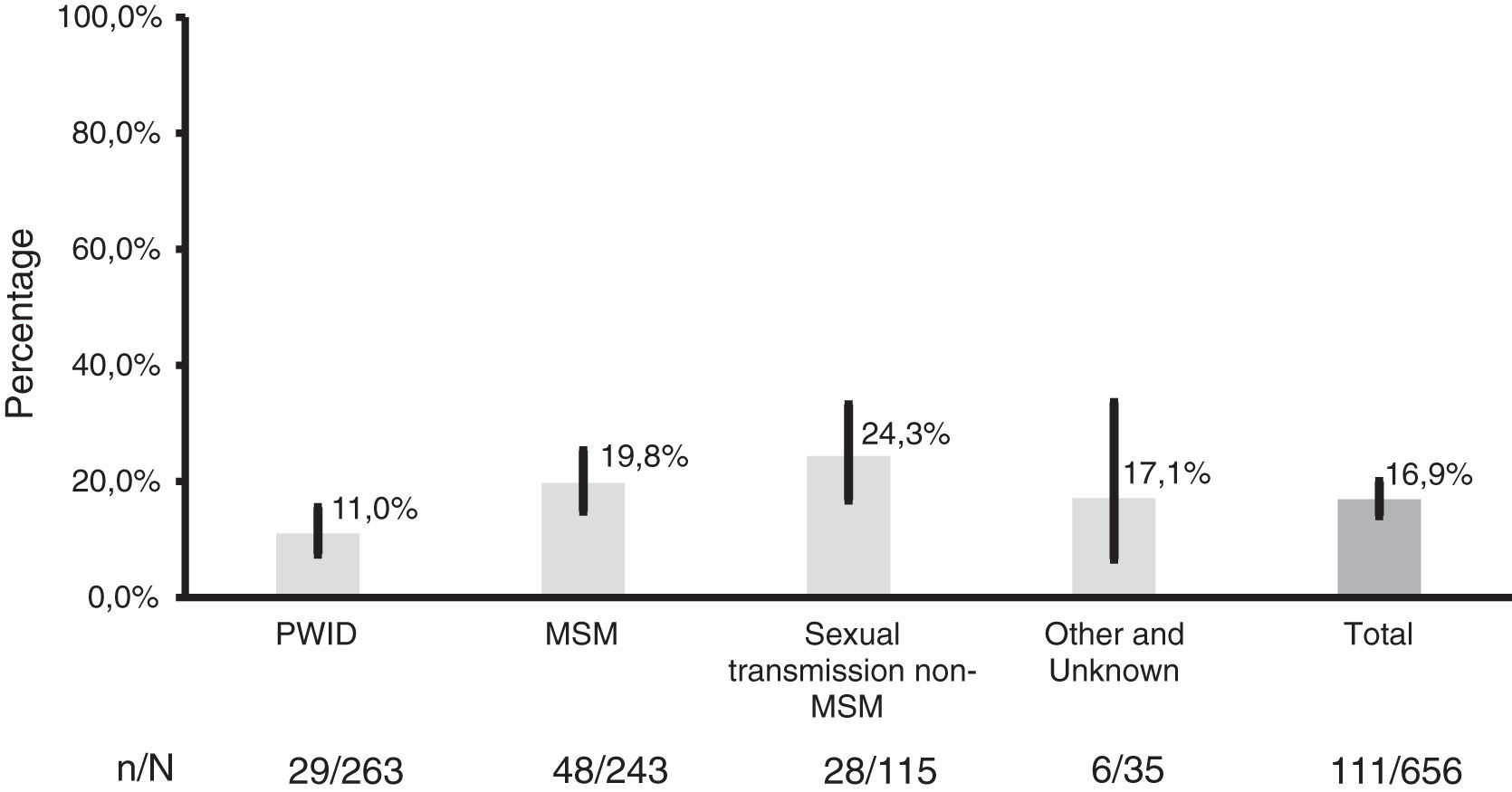
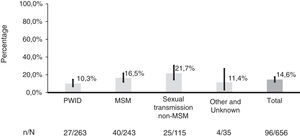
Overall, 111 [17.0% (95% CI, 14.1–20.0%)] patients were seronegative for HAV at baseline. The prevalence of HAV seronegative individuals was significantly different according to the risk factor for HIV infection (Fig. 1). Thus, a higher prevalence of non-immune patients was found in the group of people who acquired HIV infection through sexual intercourse [n=76 (21.2%, 95% CI, 17.1–25.8%)]. Among the causes for the absence of HAV immunity at baseline, the main reason was the non-referral to Preventive Medicine Unit for vaccination [n=68 (61.3%, 95% CI, 51.5–70.4%)], followed by the lack of completion of an appropriate immunization scheme [n=21 (19.0%, 95% CI, 12.1–27.5%)]. Seven [6.3% (95% CI, 2.6–12.6%)] patients were non-responders and 1 [0.9% (95% CI, 0.02–4.9%)] showed seroreversion after a successful vaccination. Among 5 [4.5% (95% CI, 1.5–10.2%)] individuals, vaccination could not be carried out because of vaccine shortage. Finally, the Vaccine Delivery Unit advised against vaccination in 7 [6.3% (95% CI, 2.6–12.6%)] patients. In the remaining individuals [n=2 (1.8%, 95% CI, 0.2–6.4%)], the cause of the absence of HAV immunity could not be ascertained.
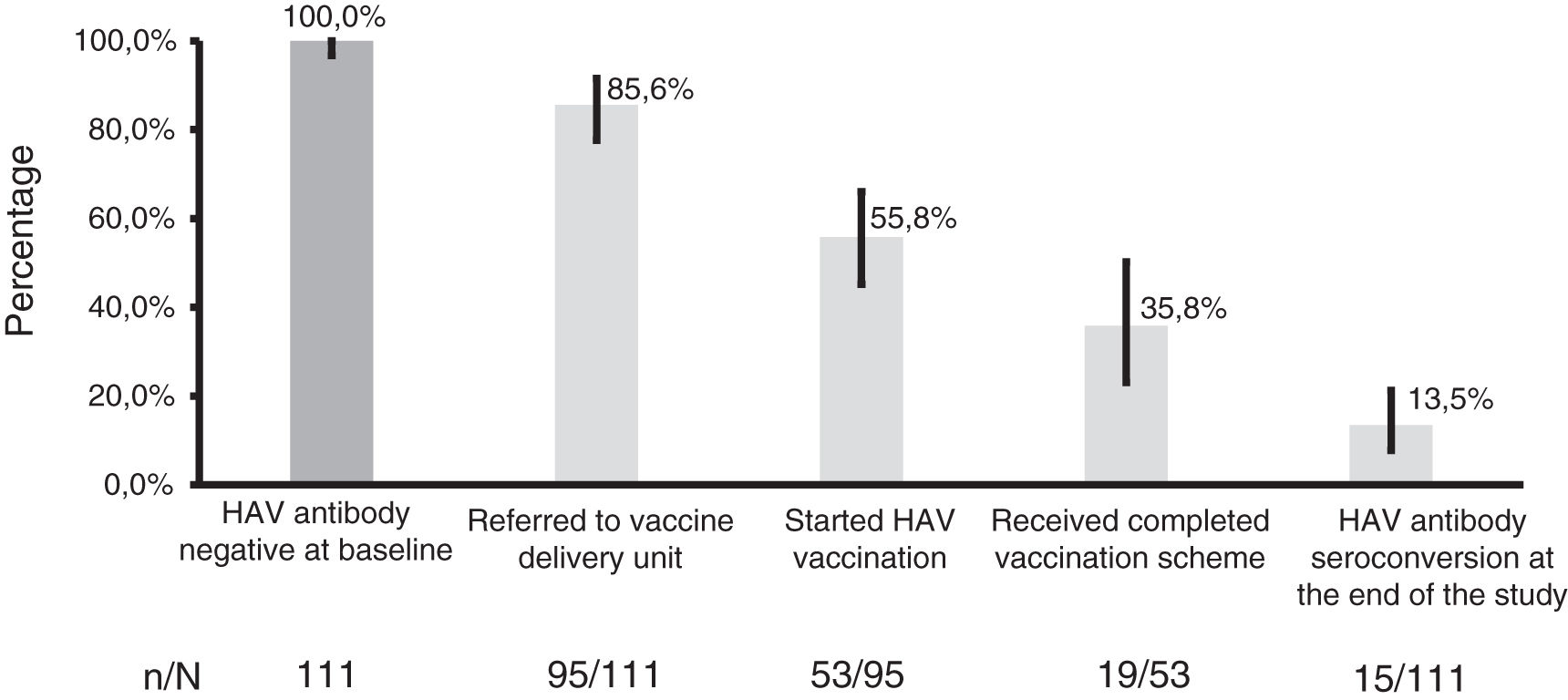
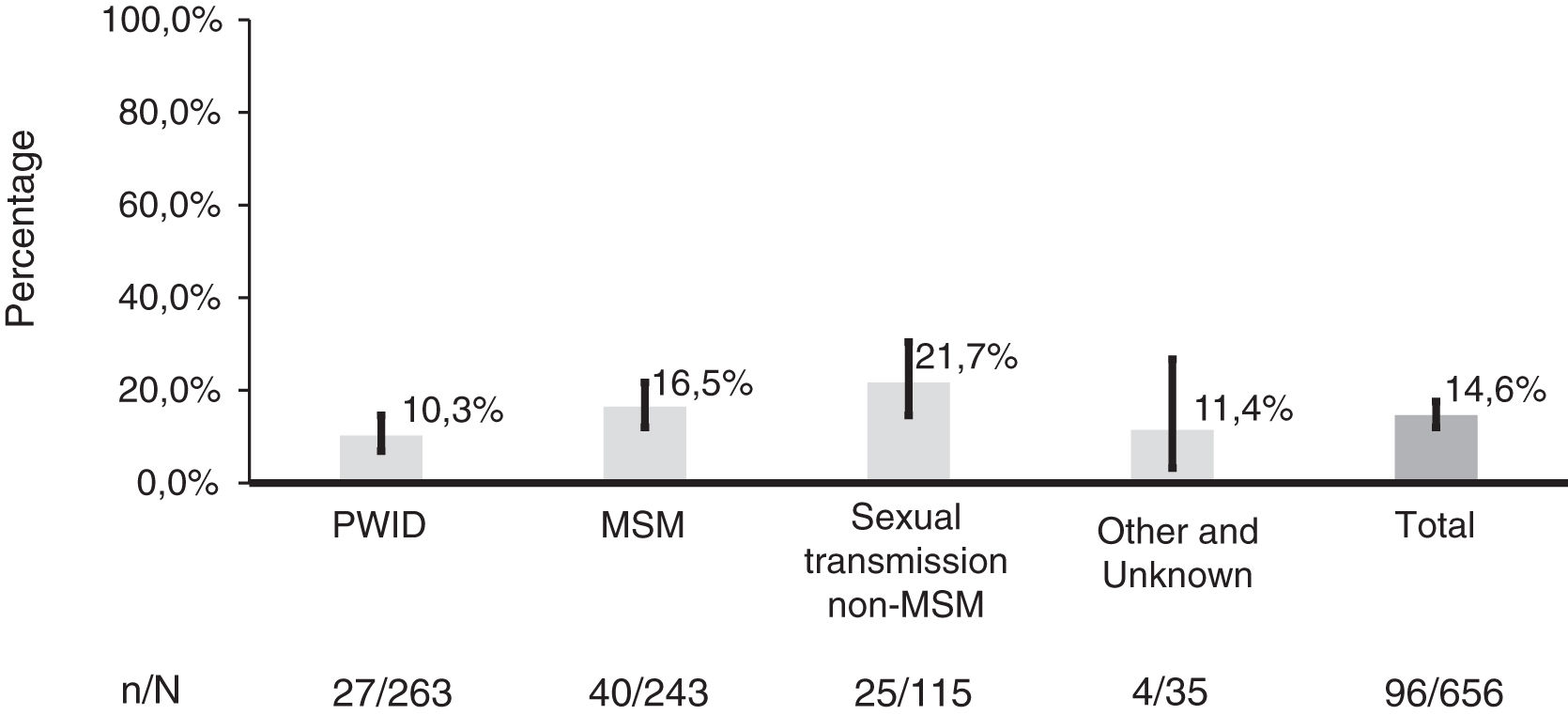
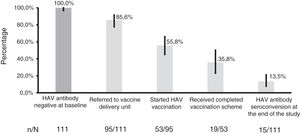
Immunization-based intervention outcomesHAV vaccination cascade among PLWH is shown in Fig. 2. The vast majority of individuals were referred to the vaccination delivery unit. Eight (7.2%) patients had other priority health conditions that prevent their referral within the study period. Likewise, the 7 (6.3%) patients who showed non-response to prior HAV vaccination and the one who seroreverted were not referred to the Vaccine Delivery Unit. Overall, 19 [17.1% (CI 95%, 10.6–25.4%)] individuals received a complete immunization scheme and 15 [13.5% (95% CI, 7.8–21.3%)] patients seroconverted against HAV. Consequently, at the end of the study, the prevalence of non-immunized PLWH was 14.6% [96/656 (95% CI, 12.0–17.6%) (Fig. 3). No significant differences in the proportion of HAV seronegative patients were found before and after the program implementation (17.0% vs. 14.6% respectively, p=0.256). Again, patients who acquire HIV infection through sexual transmission were more frequently susceptible to HAV infection [n=65, 18.2% (95% CI, 14.3–22.5%)] (Fig. 3). More specifically, taking into account MSM, no significant differences were found in the prevalence of HAV non-immune patients, before and after the intervention (19.8% vs. 16.5%, p=0.357). The leading causes of the absence of HAV immunity after the intervention were: adherence failure to the program in 23 [24.0% (95% CI, 15.8–33.7%)] patients, immunization scheme still ongoing in 34 [35.4% (95% CI, 25.9–45.8%)] individuals and waiting the first appointment with the vaccine delivery unit in 20 [20.8% (95% CI, 13.2–30.3%)] patients. In 3 [3.1% (95% CI, 0.6–8.9%)] individuals, the cause could not be determined. Because of COVID-19 pandemic, fifteen out of the 75 (20.0%) patients who already had a scheduled appointment at Preventive Medicine Unit had their consultation canceled. Overall, the median (Q1-Q3) time to referral date to vaccination starting was 180 (88–207) days.
Distribution of prevalence of hepatitis A virus seronegative individuals after the vaccination program implementation, overall and by risk factor for HIV infection (p=0.022). Abbreviations: HIV: human immunodeficiency virus; PWID: people who inject drugs; MSM: men who have sex with men.
In our setting, a considerable proportion of PLWH are still susceptible to HAV infection, mainly those who acquired HIV infection through sexual transmission. A strategy based on the active investigation of HAV non-immune cases and subsequent systematic referral for vaccination results in only modest increases in the proportion of individuals immune against HAV infection, which is largely due to failures in adherence to the vaccination program.
The current study reveals that a substantial number of patients, particularly MSM, are at risk of acquiring HAV infection in future hepatitis A outbreaks, which will likely emerge, as they are historically cyclical.4 In addition, in the setting of acute symptomatic HAV infection, it has been reported that HAV viral load and duration of viremia are higher among PLWH than in non-HIV infected individuals.21 These two conditions could promote the maintenance and spreading of HAV outbreaks. Besides, health resources might be wasted, as patients who are screened do not initiate vaccination or even do not complete vaccination due to losses to follow-up.
Characterizing the epidemiology of HAV infection among PLWH, particularly HAV susceptibility trends, is essential to design effective vaccination programs. As a matter of fact, in the past decades, the prevalence of individuals susceptible to HAV infection has increased as HAV circulation has declined in middle and high-income countries along with insufficient vaccination coverage.1 However, in the present study, the proportion of PLWH immune to HAV was substantially greater than those estimated in most of these settings among general population1,22 and PLWH.13,22 In spite of this, considerable non-immunization rates were observed, ranging from 11% to 26%, depending on the HIV risk factor considered. Critical immunity threshold for preventing hepatitis A outbreaks has been estimated to be ≥70% among MSM.23 However, the threshold of 70% PLWH with immunity might be insufficient in case of an outbreak emergence, as data from the recent HAV outbreak in Lyon, France, has shown.24 Thus, even if the susceptibility prevalence is lower than in other populations, specific groups could be more vulnerable to HAV infection due to high-risk behaviors. Accordingly, in a seroincidence study carried out in our area, we found that, even if an elevated proportion of individuals were immune, incident HAV cases peaked in the last two major outbreaks occurred in 2009–2010 and 2017–2018.9 In the present study, the prevalence of HAV immunity was higher among injecting drug users, as reported in other studies.13,14,25 This is probably driven by a greater exposure to HAV related to parenteral drug use and poorer hygienic-sanitary living conditions. It is remarkable that, despite the implementation of HAV vaccination for MSM and PLWH in the recent years, the rates of immunization in our area were similar to those found in 2008–2009,11 suggesting that immunization strategies have not been effective. In this study, the intervention carried out succeeded at identifying a maximum number of HAV-seronegative individual. However, no significant increase of the overall immunization rate was achieved, largely due to failures in adherence to the vaccination circuit.
The present study results highlight the need of improving HAV vaccination coverage in at-risk populations. Identifying perceived barriers and facilitators of HAV vaccination among PLWH should be imperative when designing an effective immunization-based intervention, particularly in pandemic conditions. In the present work, the causes of the absence of HAV immunity were multifactorial. Thus, the poor results of the immunization program could be influenced by the fact that vaccination and post-vaccination controls require additional medical visits at different units, which may be enhancing missed opportunities for hepatitis A immunization. Secondly, lack of knowledge about HAV might lead PLWH to underestimate the risk and severity of HAV infection and therefore consider vaccination not important. In the European MSM Internet Survey published in 2017, only 45% of the participants were aware of hepatitis A or B disease, the existence of a vaccine and its specific recommendation.26 More recently, this issue has once again arisen in a French study.27 Thus, interventions targeting PLWH to improve health education are needed. Finally, we cannot rule out that COVID-19 pandemic has negatively impact on immunization provision. Reduction of face-to-face medical visits, including routine immunizations, along with national lockdowns and patients concern due to COVID-19 fear have probably strengthened immunization disruption, as recent investigations have shown.28 Consequently, if maintained overtime, this situation may create pockets of susceptible individuals. Hence, identification of HAV seronegative individuals through active recruitment and the use of recalls must be a priority. Besides, to increase adherence to vaccination circuit new strategies are warranted, such as increasing the number of consultations and making schedules more flexible, while strengthening vaccination in a single act, which would acquire an additional value in times of health system overload.
This study may have some limitations. Firstly, it is a local study that may not reflect the situation in the rest of the country. However, in a large proportion of Spanish facilities, HIV and vaccination consultations are not unified. In any case, multicenter studies would be needed to confirm these findings. Secondly, part of the study was carried out in the context of the SARS-CoV-2 pandemic. This situation could have led to greater delays in the appointment at the unit responsible for vaccination or even contributed to lower attendance at the visits scheduled by this unit. However, this fact would be in line with our results, reinforcing the need for strategies that promote adherence to these consultations. Besides, as far as we know, information about the causes of HAV non-immunization among PLWH and vaccinations programs outcomes beyond outbreaks were missing. Therefore, new insights in this regard are provided herein and this is a strength of the present study.
In summary, in our setting, a significant proportion of PLWH are not immune to HAV infection and are therefore at risk of acquiring this infection in future epidemic outbreaks, especially MSM. A program based on referral to the vaccine delivery unit yields poor results, mainly due to program adherence failures. This situation could be influenced by the long waiting time to the first assessment, which might have been extended in the context of SARS-CoV-2 pandemic. Thus, a simplified follow-up strategy, with unified HIV controls and vaccination implementation, could be crucial to improve HAV immunization rates among this high-risk population.
Authors’ contributionsJuan Macias (J.M.) and Anaïs Corma-Gómez (A.C.G.) had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Juan A. Pineda (J.A.P.) and A.C.G.
Acquisition, analysis, or interpretation of data: J.M., J.A.P., A.C.G., Luis M. Real (L.M.R.), Alejandro González-Serna (A.G.S.), Noemi Oliver (N.O.), Jesús Ortega (J.O.), Pilar RINCON (P.R.), Elena Rodríguez-Pineda (E.R.P.), Marta Trigo-Rodríguez (M.T.R.).
Statistical analysis: J.A.P., J.M. and A.C.G.
Drafting of the manuscript: J.M. and A.C.G.
Critical revision of the manuscript for important intellectual content: A.C.G., J.A.P., J.M., L.M.R., M.F.F., A.S., A.G.S., N.O., J.O., P.R., E.R.P., M.T.R.
Obtained funding: J.M., A.C.G and J.A.P.
Study supervision: J.A.P. and J.M.
Financial support statementThis work was supported in part by the Instituto de Salud Carlos III (Project “PI16/01443”) integrated in the national I+D+i 2013-2016 and co-funded by the European Union (ERDF/ESF, “Investing in your future”), by the Spanish Network for AIDS investigation (RIS) (www.red.es/redes/inicio) (RD16/0025/0040), as a part of the Nacional I+D+I, ISCIII Subdirección General de Evaluación and the European Fund for Development of Regions (FEDER). JAP has received a research extensión grant from the Programa de Intensificación de la Actividad de Investigación del Servicio Nacional de Salud Carlos III (I3SNS). ACG has received a Río Hortega grant from the Instituto de Salud Carlos III (grant number CM19/00251).
Conflict of interestACG has received lecture fees from Gilead and Abbvie. JM has been an investigator in clinical trials supported by Bristol-Myers Squibb, Gilead and Merck Sharp & Dome. He has received lectures fees from Gilead, Bristol-Myers Squibb, and Merck Sharp & Dome, and consulting fees from Bristol Myers-Squibb, Gilead, and Merck Sharp & Dome. JAP reports having received consulting fees from Bristol-Myers Squibb, Abbvie, Gilead, Merck Sharp & Dome, and Janssen Cilag. He has received research support from Bristol-Myers Squibb, Abbvie and Gilead and has received lecture fees from Abbvie, Bristol-Myers Squibb, Janssen Cilag, and Gilead. The remaining authors report no conflict of interest.