Automated antimicrobial susceptibility testing devices are widely implemented in clinical microbiology laboratories in Spain, mainly using EUCAST (European Committee on Antimicrobial Susceptibility Testing) breakpoints. In 2007, a group of experts published recommendations for including antimicrobial agents and selecting concentrations in these systems. Under the patronage of the Spanish Antibiogram Committee (Comité Español del Antibiograma, COESANT) and the Study Group on Mechanisms of Action and Resistance to Antimicrobial Agents (GEMARA) from the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC), and aligned with the Spanish National Plan against Antimicrobial Resistance (PRAN), a group of experts have updated this document. The main modifications from the previous version comprise the inclusion of new antimicrobial agents, adaptation of the ranges of concentrations to cover the EUCAST breakpoints and epidemiological cut-off values (ECOFFs), and the inference of new resistance mechanisms. This proposal should be considered by different manufacturers and users when designing new panels or cards. In addition, recommendations for selective reporting are also included. With this approach, the implementation of EUCAST breakpoints will be easier, increasing the quality of antimicrobial susceptibility testing data and their microbiological interpretation. It will also benefit epidemiological surveillance studies as well as the clinical use of antimicrobials aligned with antimicrobial stewardship programs.
Los sistemas automáticos utilizados en el estudio de la sensibilidad a los antimicrobianos están introducidos en la mayoría de los laboratorios de Microbiología Clínica en España, utilizando principalmente los puntos de corte del European Committee on Antimicrobial Susceptibility Testing (EUCAST). En 2007, un grupo de expertos publicó unas recomendaciones para incluir antimicrobianos y seleccionar concentraciones en estos sistemas. Bajo el auspicio del Comité Español del Antibiograma (COESANT) y del Grupo de Estudio de los Mecanismos de Acción y Resistencia a los Antimicrobianos (GEMARA) de la Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica (SEIMC) y alineado con el Plan Nacional frente a la Resistencia a los Antibióticos (PRAN), un grupo de expertos ha actualizado dicho documento. Las principales modificaciones realizadas sobre la versión anterior comprenden la inclusión de nuevos agentes antimicrobianos, la adaptación de los rangos de concentraciones para cubrir los puntos de corte clínicos y los puntos de corte epidemiológicos (ECOFF) definidos por el EUCAST, y para la inferencia de nuevos mecanismos de resistencia. Esta propuesta debería ser considerada por los diferentes fabricantes y los usuarios cuando se diseñen nuevos paneles o tarjetas. Además, se incluyen recomendaciones para realizar informes selectivos. Con este enfoque, la implementación de los puntos de corte del EUCAST será más fácil, aumentando la calidad de los datos del antibiograma y su interpretación microbiológica. También será de utilidad para los estudios de vigilancia epidemiológica, así como para el uso clínico de los antimicrobianos, de acuerdo con los programas de optimización de uso de antimicrobianos (PROA).
In 2007, the Study Group on Mechanisms of Action and Resistance to Antimicrobial Agents (GEMARA) and the Spanish Committee on Antimicrobial Susceptibility testing (named as MENSURA at that time) published, under the auspices of the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC), “Recommendations for selecting antimicrobial agents for in vitro susceptibility studies using automatic and semiautomatic systems.1 Since then, significant efforts in Europe for harmonization of susceptibility testing methods and definition of breakpoint clinical criteria have been done led by the European Committee of Antimicrobial Susceptibility Testing (EUCAST)2 and Spain has created the COESANT (Comité Español del Antibiograma) committee, which is the Spanish National Antimicrobial Committee (NAC) aligned with EUCAST.3 Ever since, several new antimicrobials have been marketed, new resistance mechanisms have been described,4,5 and health authorities have promoted plans to address the problem of antimicrobial resistance.6 In addition, professional societies, such as the SEIMC, have designed antimicrobial stewardship programs, for the better use of antimicrobial agents with the aim to curtail increasing prevalence of resistance.7 Within these programs, the importance of antimicrobial susceptibility testing (AST), characterization of resistance mechanisms and analysis of clonal relationship are highlighted.
Unlike Northern European countries, but in common with many other countries worldwide, automated and semiautomated systems for AST are widely distributed in Spanish clinical microbiology laboratories. In a recent survey performed by the SEIMC in which 156 Spanish microbiology laboratories participated, 92.3% of them routinely used these systems (unpublished data). These data are consistent with those reported in recent multicentre quality control studies on antimicrobial susceptibility testing performed in Spain.8–10 This wide distribution may have several advantages such as testing a high number of antimicrobial agents per isolate, and a better inference of resistance phenotypes with the aid of the so-called “expert systems” incorporated in these devices, the potential aggregation of data in MIC-based surveillance systems, and the reporting of MIC values to adapt patients’ antimicrobial therapy applying pharmacokinetics-pharmacodynamics (PK-PD) criteria. Nevertheless, different manufacturers include diverse antimicrobials with different ranges of concentrations, which hinder some of these advantages, particularly the data aggregation in surveillance programs and in some cases, the inference of resistance mechanisms. In most cases, the design of panels or cards used in these systems does not follow a consensus procedure and only few documents address which antibiotics and concentrations should specifically be included.1,11,12
In the current document we have updated the previous version of “Recommendations for selecting antimicrobial agents for in vitro susceptibility studies using automatic and semiautomatic systems”.1 This new version has been led by COESANT, SEIMC and its study group GEMARA in the context of the Spanish Plan of Antimicrobial Resistance (PRAN, Plan Nacional de Resistencia a los Antimicrobianos) coordinated by the Spanish Agency of Medicines and Sanitary Products (AEMPS, Agencia Española de los Medicamentos y Productos Sanitarios).13 This manuscript was prepared by a group of experts and was submitted for public consultation through the COESANT and SEIMC websites. The manufacturers of automated AST devices marketed in Spain were also included in this consultation. The final version was constructed considering all these opinions.
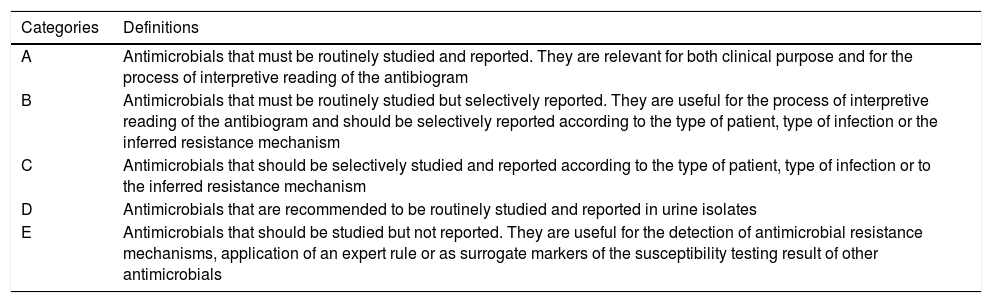
Objectives and general recommendations for antimicrobial susceptibility testing using automated and semiautomated systemsThe main objective in the elaboration of this document was to update the general recommendations for the selection of the antibiotics and their concentrations to be included in the AST panels used by automated or semiautomated systems commercialized in Spain that was published in 2007.1 Likewise, suggestions for selective reporting of susceptibility testing results are also included (Table 1). The participating experts have also agreed on these recommendations of selective reporting. Recently, a European study has recognized this procedure as part of the stewardship programs in which clinical microbiology laboratories should actively participate through their informatics systems.14 Obviously, this selective reporting can be facilitated with appropriate recommendations for antimicrobial testing against different microorganisms. In the European study, Spain was classified as a country with partial implementation of this procedure and the present document can facilitate criteria to enhance the number of laboratories with this practice.
Categories used for the inclusion of the antimicrobial agents in susceptibility testing panels for automated systems.
| Categories | Definitions |
|---|---|
| A | Antimicrobials that must be routinely studied and reported. They are relevant for both clinical purpose and for the process of interpretive reading of the antibiogram |
| B | Antimicrobials that must be routinely studied but selectively reported. They are useful for the process of interpretive reading of the antibiogram and should be selectively reported according to the type of patient, type of infection or the inferred resistance mechanism |
| C | Antimicrobials that should be selectively studied and reported according to the type of patient, type of infection or to the inferred resistance mechanism |
| D | Antimicrobials that are recommended to be routinely studied and reported in urine isolates |
| E | Antimicrobials that should be studied but not reported. They are useful for the detection of antimicrobial resistance mechanisms, application of an expert rule or as surrogate markers of the susceptibility testing result of other antimicrobials |
However, although the document focuses on MIC-based automated systems, most of the established criteria related to the selection of the antibiotics to be included in the antibiogram and the reporting of the results can also be applied to the agar diffusion-based methods, either with disc or with MIC gradient strips. Since the first consensus document was published in 2007, a number of new antimicrobial agents have been approved, several indications have been changed or expanded, and different breakpoints have been significantly modified making it necessary to revise the previous document and to include new antimicrobials (Supplementary Tables S1–S9). Moreover, the use of traditional susceptible clinical breakpoints does not necessarily recognize isolates with low-level resistance mechanisms15,16 and recognition of wild-type populations and the definition of the epidemiological cut-off values (ECOFF) have been widely used.
More recently, EUCAST has modified definitions of interpretive clinical categories [susceptible (S), intermediate (I) and resistant (R)]. These new definitions mainly affect to the I category, which is now interpreted as “susceptible, increased exposure” which occurs when there is a high likelihood of therapeutic success because exposure to the agent is increased by adjusting the dosing regimen or by its concentration at the site of infection.17 As a consequence, EUCAST has modified some breakpoints and others only apply when high exposure of the microorganisms to the agent is considered (i.e. most β-lactams and Pseudomonas aeruginosa).18 In addition, Modify the order: EUCAST has introduced a new concept which has been designed as an Area of Technical Uncertainty (ATU) for some organism-agent combinations. It corresponds to an MIC value and/or zone diameter interval where the categorisation is doubtful. Further explanations and how to deal with results in the ATU are explained in the EUCAST breakpoint Tables.18
Automated and semiautomated systems should have a minimal set of characteristics making them appropriate to fulfill the objectives for which they were designed, allowing the application of the general criteria used in the antibiogram interpretive reading.19,20 These criteria are summarized in the following points:
- (a)
Availability of the identification of the microorganism under study which is necessary for the antibiogram interpretive reading and for the inference of the resistance mechanisms.18,19 This can be achieved through either biochemical tests included in the same panel/card or an additional panel/card or through any other method, including MALDI-TOF mass spectrometry. When the automated AST systems are linked to MALDI-TOF mass spectrometry devices, it would be desirable that this information could be also used for epidemiological purposes in the identification of antimicrobial resistance mechanisms and bacterial clones.21
- (b)
Incorporate an informatics application with the capacity to interpret MIC values (or inhibition zones) establishing the S, I and R clinical categories.. This software should apply criteria recommended by EUCAST,18 although it is recommended that it may allow the access to the criteria established by other susceptibility testing committees, such as CLSI,12 or those specifically defined by COESANT (Supplementary Tables S1–S9).
- (c)
Incorporate the so-called “expert systems” for antibiogram interpretive reading, able to recognize phenotypes of resistance to multiple antibiotics from the same or different families and inferring the underlying resistance mechanisms.19,20
- (d)
Allow a bidirectional connection with the Laboratory Informatics System (LIS), required not only for the transference of AST data but also to receive the necessary information for the management of results, particularly with the aim of conducting epidemiological analysis, infection control studies, and antimicrobial stewardship programs.7 Ideally, these systems should be compatible for the connection to national and international surveillance databases. The incorporation of these “expert” programs facilitates daily work and decreases the workload. Moreover, these devices should also be able to connect with programs using databases for infection control programs.
The inclusion of antimicrobials in the panels of automated susceptibility testing systems is mainly conditioned by their clinical interest. However, other points should also be considered, such as the type of microorganism or the need of interpretation of resistance mechanisms. In our document, the selection of the different compounds was performed considering the following criteria:
Microbiological criteriaThe antimicrobials to be included in the AST panels, regardless of the type of automated system, are those required for the interpretive reading of the susceptibility pattern and for the inference of underlying resistance mechanisms.22–24 The selection of antimicrobials is also intended to contribute to the inference of complex phenotypes causing multidrug-resistant profiles, such as those derived from the simultaneous presence of different resistance mechanisms affecting various members of a unique family, e.g. β-lactam antibiotics.19,25 Moreover, certain antimicrobials, such as tetracycline or chloramphenicol, have been mainly selected for epidemiological monitoring purposes.
In the case of antimicrobials belonging to families with several members, e.g. cephalosporins and fluoroquinolones, selected compounds are considered as representative of the antimicrobial activity of the group, additionally allowing the deduction of the activity of those that are not included in the panels as well as the assumption of the presence of resistance mechanisms.23 The only purpose of including certain antimicrobials, in some cases without clinical use such as nalidixic acid, is to act as a marker of a primary resistance step which indicates the presence of mutations that can preclude the use of fluoroquinolones in subsequent rounds of topoisomerase mutations.25 Similarly, kanamycin resistance alerts for the presence of some aminoglycoside-modifying enzymes affecting amikacin while the association of clavulanic acid with a third or fourth generation cephalosporin helps to identify the presence of an extended-spectrum-β-lactamase.26 Another example is cefoxitin in panels for the study of Enterobacterales, which help to predict the presence of AmpC β-lactamases (either chromosomally or plasmidic encoded) and/or a deficit in outer membrane permeability.24,27 In the case of staphylococci, cefoxitin has been included as it performs better than oxacillin as a marker for detecting the presence of the mec genes causing methicillin resistance.28
The emergence and sudden dispersion of a resistance mechanism may increase the interest for the study of a particular compound. This is the case of the acquired carbapenemases in gram-negative bacilli that have raised interest in aztreonam as an indicator of the presence of metallo-β-lactamases, particularly when the study is simultaneously performed with ceftazidime, the combination of ceftazidime-avibactam and carbapenems.29 Additionally, tigecycline, a glycylcycline derivative of minocycline, has been included as it can be a therapeutic option against some multidrug-resistant gram-negatives.30
In the case of staphylococci, the simultaneous presence of a concentration of erythromycin together with one of clindamycin in the same well is intended to detect inducible macrolide-clindamycin resistance.31 Moreover, daptomycin and linezolid have been included as they represent last-resort line therapeutic options against gram-positive cocci.32 More recently, certain panel/card manufacturers have also included ceftaroline, a new cephalosporin with activity against methicillin-resistant Staphylococcus aureus.33
Pharmacokinetic/pharmacodynamic (PK/PD) criteriaEUCAST uses PK/PD Monte Carlo simulations as a key component of its breakpoints’ setting process for old and new antimicrobials. The PK/PD breakpoint is the MIC value considered necessary to achieve a probability of target attainment of >95% and applies to specific dosage regimens.34 The PD targets predicting maximum efficacy of the antimicrobial, for example 50% for the percentage of the dosing interval during which the serum concentration exceeds the MIC (%T>MIC) of a β-lactam, 100% for an area under the concentration-time curve/MIC ratio (AUC24/MIC) of a fluoroquinolone, or 10 times for peak plasma concentration/MIC ratio (Cmax/MIC) of an aminoglycoside, expressed as a function of the unbound drug concentration.
The magnitude of the PD target can vary among bacterial species.35 A clinical breakpoint setting process requires knowledge of the wild-type distribution of MICs, assessment of the pharmacokinetic/pharmacodynamic (PK/PD) parameters, and study of the clinical outcome of the infected patient when the antimicrobial agent is used.34,36 The use of PK parameters in the simulations considering different populations (healthy volunteers or critically ill patients with different degrees of renal function), various dose regimens and multiple infection sites (urinary concentrations of antimicrobial agents are higher than serum concentrations over a dosing interval) will result in different breakpoints. EUCAST has defined several breakpoints which are only valid for isolates from uncomplicated urinary tract infections (e.g. amoxicillin-clavulanic acid MIC breakpoint S ≤32mg/L for Enterobacterales).21
PK/PD data and MIC distributions comprise the primary data to support decisions concerning revised breakpoints. For β-lactam antimicrobials and P. aeruginosa, susceptible and I (susceptible, increased exposure) breakpoints are established to ensure optimal exposures with specific dosage regimens.17 Additionally, the MIC and associated breakpoints are a better means for guiding selection of therapy for individual patients.37–39
It is important to consider that accuracy of the automated susceptibility tests depends, among other factors, on the concentration of the antibiotics, as the lower the concentration, the higher the error rates.40
Clinical criteriaInformation about the bacterial susceptibility pattern is essential to guide the selection of antibiotic treatment. Furthermore, it is well known that there are many important host factors determining the clinical outcome. Several clinical data demonstrate that an in vitro susceptible result often predicts therapeutic success. However, even in patients with sepsis due to a microorganism with an in vitro resistant result, resistance in vivo with concomitant clinical failure cannot be always predicted.41,42 Therefore, and from a clinical point of view, the most commonly used antibiotics or at least one representative of the antibiotic family that predicts the activity of the other members, should be included in the routine susceptibility report as occurs with first generation cephalosporins. This surrogated use is also claimed in the case of new antimicrobials when they are not yet included in testing devices. This is the case of tedizolid and linezolid or dalbavancin and vancomycin.
In addition, when the MIC is high but within the susceptibility range suggesting the presence of a specific low-level resistance mechanism, or when clinical data indicate worse outcome when the MIC is high, alternative antibiotics should be tested. For instance, when MICs of carbapenems for Klebsiella spp. or E. coli are high, suggesting the presence of a carbapenemase, alternative antibiotics including colistin, tigecycline or fosfomycin should be tested. A similar approach might occur when considering MICs of vancomycin >1 and ≤2mg/l for S. aureus causing bacteremia, which has been associated to a worse outcome in some studies,44,43 it is recommended to report data concerning the susceptibility status of possible alternatives.
Nowadays, new antimicrobials, such as ceftazidime-avibactam or ceftolozane-tazobactam for gram-negatives as well as dalbavancin, telavancin or oritavancin for gram-positives, have been included in testing devices. AST of these compounds are recommended not only to obtain information of new therapeutic alternatives but also to generate routine epidemiological data.
Criteria for the selection of antimicrobial concentrationsThe selection of the concentrations proposed for each antimicrobial agent has been made with the objective of covering the breakpoints used for defining clinical categories (susceptible, intermediate and resistant) established by EUCAST.17 For certain antimicrobials, specific COESANT recommendations have been considered (specified in the supplementary tables of this document). In addition, since the number of wells available in the different panels or cards varies from one manufacturer to another, more concentrations are also recommended. All these concentrations are classified in different groups. The first one (indicated in bold in (Supplementary Tables S1–S9).) includes the concentrations that would be essential to respond to the previous objective (covering EUCAST breakpoints) and therefore, should always be included in the susceptibility testing panels. This range is mainly intended to include the concentration defining the resistance breakpoint and one dilution below the susceptible breakpoint. In addition, there are other concentrations (not indicated in bold) that could be added to encompass the ECOFF value to detect wild-type populations or to facilitate epidemiological surveillances, especially of microorganisms with low-level resistance mechanisms. This approach also contributes to a better interpretive reading of the antibiogram.19,20
Definition of categories and groups of antimicrobial agents tested in the antibiogramFive different categories of antimicrobials have been established (A to E) with the recommendation of inclusion in the panels and selective reporting depending on the clinical relevance of the antimicrobial tested, type of patient or type of infection. Moreover, these recommendations also consider the interest of the antimicrobials for the interpretive reading of the antibiogram and the inference of resistance mechanisms (Table 1). A specific category (category D) has been defined for antimicrobials that are recommended to be routinely studied and reported in urine isolates. These antimicrobials normally have clinical breakpoints specifically adapted for non-complicated urinary tract infections,12,21 and some manufacturers offer specific panels for microorganisms involved in these infections.
The last category (category E) is exclusively established for those antimicrobials recommended to be studied but not reported. They are useful for the detection of antimicrobial resistance mechanisms, such as nalidixic acid and gyrA and topoisomerase IV mutations in gram-negative organisms, application of an expert rule or inference of a resistance mechanism, such as the combinations of third or fourth generation cephalosporins with clavulanic acid, or as subrogated markers of the susceptibility result of other antimicrobials.19,20,25,26 Overall, they are not relevant for clinical purposes.
Concluding remarksSpain is a country where automated susceptibility testing systems are widely distributed and every day, thousands of AST data are produced by clinical microbiology laboratories. These data, as it is quoted in a European survey and in quality control studies performed in Spain, are selectively reported by an important number of laboratories using EUCAST breakpoints.8–10,14 All these data are mainly used for clinical purposes for patients’ treatments. Moreover, they should also be useful for surveillance and for tracking the evolution of antimicrobial resistance at local or national level if compiled in a common database, which is an objective of the Spanish National Plan against Antimicrobial Resistance (PRAN).13 However, its development might be complex due to the lack of homogeneity in the number of antibiotics tested for each microorganism and also, importantly, in the concentrations tested for each antimicrobial, which precludes not only fully implementation of the EUCAST breakpoints but also data compilation.
Considering the criteria explained in the previous paragraphs, we propose those antimicrobial agents and concentrations to be used in the study of in vitro susceptibility of the different microorganisms when automated systems are used (Supplementary Tables S1–S9). Different manufacturers and users should consider this proposal when designing or using new panels. We believe that with this approach, the implementation of EUCAST breakpoints will be easier, increasing the quality of data and their microbiological interpretation.44,45 Finally, it will benefit epidemiological surveillances as well as the clinical use of antimicrobials aligned with the stewardship programs.
FundingThis document did not have any specific funding. COESANT activities are partially funded by the Agencia Española de Medicamentos y Productos Sanitarios (AEMPS) and the Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica (SEIMC).
Scientific and research activities of RC, AO, GB, JC, JC, MAD, FFC, LLC, FM, MIM, JOI, AP, MPV, JV and LM-M are Supported by Plan Nacional de I+D+i 2013–2016 and Instituto de Salud Carlos III, Subdirección General de Redes y Centros de Investigación Cooperativa, Ministerio de Economía, Industria y Competitividad, Spanish Network for Research in Infectious Diseases (REIPI) (RD16/0016/0001; RD16/0016/0002; RD16/0016/0003; RD16/0016/0004; RD16/0016/0005; RD16/0016/0006; RD16/0016/0007; RD16/0016/0008; RD16/0016/0010; RD16/0016/0011; RD16CIII/0004/002) – cofinanced by European Development Regional Fund “A way to achieve Europe”, Operative program Intelligent Growth 2014–2020 and of CT by Plan Nacional de I+D+i 2013–2016, Ministerio de Economía, Industria y Competitividad, Spain (SAF2016-76571-R).
Conflict of interestRC has participated in educational activities sponsored by BD and bioMérieux and in clinical validation studies of in vitro diagnostic medical devices from bioMérieux. AC has participated in educational activities sponsored by BD. MAD has participated in educational activities sponsored by Beckman Coulter. GB, NL and JV have participated in educational activities sponsored by bioMérieux. LMM has participated in educational activities sponsored by bioMérieux and an advisory board meeting with BD Switzerland. Other authors declare no conflict of interest.