We have read with interest the recent work published in your journal by González-del Castillo et al.,1 in relation to the impact of the emergency department's (ED) inappropriate administration of antibiotic therapy on the efficiency of hospitalisation. We congratulate the authors for their work and for “bringing to the forefront” one of the clearly defined and unresolved areas of improvement for EDs; the early and appropriate administration of antibiotic treatment (AB).2–4 We share many of the views presented in their discussion, as well as their conclusions when it is stated that, in their experience, the inappropriate prescribing of empiric AB treatment in patients admitted from the ED leads to prolonged stays. But we cannot agree when they say that there is no increase in complications, readmissions or even mortality. Thus, in line with this statement, we would like to present some comments about the need to implement programs to optimise the use of AB (PROA)2 in EDs, and thus move away from a possible deceptive message of relaxation for the clinician that may have made him think that “things are being done correctly”, when, in fact we must assume that the rate of inappropriateness of antibiotic therapy in both primary care,5 and in some EDs, is significant.6 And this has to be improved, to ensure that the result is efficiency, but also efficacy and effectiveness, both for the system and for the patient's progression (and here we include both those who are admitted and those who do not need to be admitted.6 And in order to do this, there are experiences and strategies that have shown a very significant improvement in the overall care of the patient with infection in the ED from their triage7 and, in particular, in the increase of appropriate (empirical indication according to local guidelines and resistance, route of administration, dosage, no need for later change of AB, etc.) and early (in the ED itself in the first hour if the patient has severity criteria or when making the clinical diagnosis in the remainder) administration.8,9
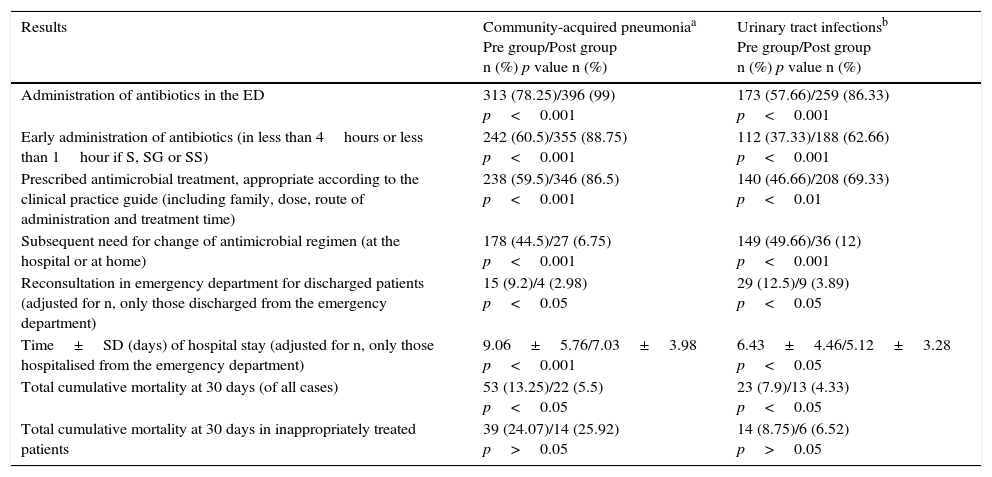
We think that the study by González-del Castillo et al.1 has an intrinsic characteristic, recognised by the authors themselves, that determines its results, and which restricts its external validity. It shows an inappropriate AB treatment in only 10% of patients (not comparable to the 80% published in primary care5 or approx. 40% in various EDs).6 However, this fact is specifically due to the excellent results of implementing therapeutic guides in their own ED, agreed with a multidisciplinary team (from the Infection Commission), and training activities included in the PROAs, in which ED representatives are involved. The bad news is that unfortunately in many centres the variability in the prescription of antimicrobials is very high and the adherence to the guides of the scientific societies could be significantly improved.4 However, the good news is that when guidelines adapted to epidemiological patterns and local resistance are implemented, disseminated and accompanied by training activities in a centre using the PROA, proper and early administration of AB is significantly increased,6,8 and thus, in addition to improving the hospital stay, many other outcome variables are improved as well, as we have seen in the two most frequent infectious processes, and that greater AB admissions and treatments are needed in the ED; urinary tract infections (UTIs) and community acquired pneumonia (CAP). To do this, using the databases of two previously conducted studies,6,10 we compared the results and the management in relation to AB therapy before and after the implementation of a PROA for both CAP and UTIs. To this end, two prospective observational, single-blind studies were designed, where two independent observers reviewed the histories of the groups defined as pre-PROA (where AB treatment was administered according to the freely-taken decisions of the attending physician) and post-PROA (after the implementation of treatment protocols). Some results are shown in Table 1, which shows how inappropriate AB therapy (whose key factor is the lack of adherence to the recommended guidelines) can be related to the hospital stay, but also to patient morbidity and mortality rates.
Related factors and indicators of antibiotic management in patients with community-acquired pneumonia and urinary tract infections in the emergency department.
| Results | Community-acquired pneumoniaa Pre group/Post group n (%) p value n (%) | Urinary tract infectionsb Pre group/Post group n (%) p value n (%) |
|---|---|---|
| Administration of antibiotics in the ED | 313 (78.25)/396 (99) p<0.001 | 173 (57.66)/259 (86.33) p<0.001 |
| Early administration of antibiotics (in less than 4hours or less than 1hour if S, SG or SS) | 242 (60.5)/355 (88.75) p<0.001 | 112 (37.33)/188 (62.66) p<0.001 |
| Prescribed antimicrobial treatment, appropriate according to the clinical practice guide (including family, dose, route of administration and treatment time) | 238 (59.5)/346 (86.5) p<0.001 | 140 (46.66)/208 (69.33) p<0.01 |
| Subsequent need for change of antimicrobial regimen (at the hospital or at home) | 178 (44.5)/27 (6.75) p<0.001 | 149 (49.66)/36 (12) p<0.001 |
| Reconsultation in emergency department for discharged patients (adjusted for n, only those discharged from the emergency department) | 15 (9.2)/4 (2.98) p<0.05 | 29 (12.5)/9 (3.89) p<0.05 |
| Time±SD (days) of hospital stay (adjusted for n, only those hospitalised from the emergency department) | 9.06±5.76/7.03±3.98 p<0.001 | 6.43±4.46/5.12±3.28 p<0.05 |
| Total cumulative mortality at 30 days (of all cases) | 53 (13.25)/22 (5.5) p<0.05 | 23 (7.9)/13 (4.33) p<0.05 |
| Total cumulative mortality at 30 days in inappropriately treated patients | 39 (24.07)/14 (25.92) p>0.05 | 14 (8.75)/6 (6.52) p>0.05 |
For the comparative analysis, the program IBM®-SPSS® Statistics v.19 for Windows, was used, with a p value<0.05 considered significant. Fisher's test, Chi-square test for proportions and Student t or Mann–Whitney U test were used to compare the parameters between the 2 groups, as applicable.
SD: standard deviation; S: sepsis; SG: severe sepsis; SS: septic shock; ED: emergency department.
Please cite this article as: Solis-Ovando F, López-Forero WE, Dionisio-Coronel YB, Julián-Jiménez A. Consideraciones sobre la inadecuación de la antibioterapia en el servicio de urgencias. Enferm Infecc Microbiol Clin. 2017;35:396–397.