Cancer is a leading cause of death in individuals with HIV.
MethodsThe incidence of cancer in HIV patients of the CoRIS cohort in the 2004–2009 and 2010–2015 periods has been analysed and compared to the incidence in the Spanish general population, estimated from data of the Spanish Cancer Registry Network.
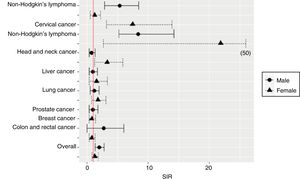
ResultsBetween January 2004 and November 2015, 12,239 patients were included in CoRIS and 338 incident cancer cases were diagnosed. The overall incidence of cancer per 100,000 persons-year (95% CI) was 702.39 (629.51–781.42) with no significant differences between the 2 periods. A 38% of the incident cancer cases were AIDS defining cancers (ADC) and 62% non-AIDS defining cancers (NADC). In the period 2010–2015, there was a significant decrease in the incidence of ADC (standardised incidence ratio [SIR]); 95% CI: 0.38; 0.21–0.66) and NADC predominated. Compared to the general population, the incidence of cancer was double in men with HIV. Higher relative risks were documented (SIR; 95% CI) for Hodgkin's lymphoma in both sexes (males: 8.37, 5.13–14.17; females: 21.83, 2.66–47.79), non-Hodgkin's lymphoma in males (5.30, 2.86–8.45) and cervical cancer (7.43, 3.15–13.87) and head and neck cancer (3.28, 1.21–5.82) in women.
ConclusionsThe overall incidence of cancer in individuals with HIV is higher than in the Spanish general population, and it has remained stable since 2004 with a current predominance of NADC. These data suggest that additional efforts should be made in the prevention and the early detection of cancer in these patients.
El cáncer constituye una causa importante de mortalidad en personas con VIH.
MétodosSe ha analizado la incidencia de cáncer en pacientes con VIH de CoRIS en los períodos 2004-2009 y 2010-2015 y se ha comparado con la de la población general española estimada a partir de los datos de la Red Española de Registros de Cáncer.
ResultadosEntre enero de 2004 y noviembre de 2015 se incluyeron en CoRIS 12.239 pacientes y se diagnosticaron 338 casos incidentes de cáncer. La incidencia global por cada 100.000 personas/año (IC 95%) fue de 702,39 (629,51-781,42) sin diferencias significativas entre los 2 períodos. El 38% de las neoplasias fueron tumores definitorios de sida (TDS) y el 62% no definitorios de sida (TNDS). En el período 2010-2015 se observó un descenso significativo en la incidencia de TDS (cociente de tasas de incidencia estandarizadas [SIR]; IC 95%: 0,38; 0,21-0,66) y predominaron los TNDS. En comparación con la población general, la incidencia de cáncer fue el doble en varones con VIH. Se documentaron riesgos relativos (SIR; IC 95%) más altos de linfoma Hodgkin en ambos sexos (varones: 8,37; 5,13-14,17; mujeres: 21,83; 2,66-47,79), linfoma no Hodgkin en varones (5,30; 2,86-8,45) y cáncer de cérvix (7,43; 3,15-13,87) y cabeza y cuello (3,28; 1,21-5,82) en mujeres.
ConclusionesLa incidencia global de cáncer en personas con VIH es mayor que en la población general española y se mantiene estable desde 2004, con un predominio actual de los TNDS. Estos datos indican que deben realizarse esfuerzos adicionales en la prevención y detección precoz de cáncer en estos pacientes.
Cancer is one of the main complications of immunodeficiency associated with human immunodeficiency virus (HIV) infection.1 Since the onset of the epidemic, Kaposi's sarcoma, non-Hodgkin's lymphoma and cervical cancer have been considered AIDS-defining cancers (ADCs) and their incidence declined substantially with the introduction of combination antiretroviral therapy (ART) in 1996.2 Nevertheless, with the expansion of ART and the increased life expectancy of HIV-positive individuals, a higher incidence of other non-AIDS-defining cancers (NAFC),2 including cancers associated with viral co-infections, such as anal and oropharyngeal cancers associated with human papillomavirus infection, liver cancer associated with hepatitis B and C virus infection and Hodgkin's lymphoma associated with Epstein-Barr virus infection, have been observed. The same is true for lifestyle-related cancers, such as lung cancer associated with smoking.2,3 In the HIV/AIDS Cancer Match study, after the introduction of ART, the proportion of NADCs was observed to increase from 31% to 58% in 2002 and, on analysing the 2003–2010 data, 66% of all cancers were NADCs.1 Most epidemiological studies that have analysed the incidence of NADCs in HIV-infected individuals have documented higher incidence rates than those observed in the general population.4–6
Today, cancer is responsible for a considerable fraction of the cancer incidence and mortality burden among people living with HIV.2,7 In the US, more than 10% of all deaths in people receiving ART between 1995 and 2009 were attributable to cancer.8 In a multi-cohort collaboration (data collection on adverse events of anti-HIV Drugs) on trends in underlying causes of death in people with HIV from 1999 to 2011, the percentage of deaths due to NADCs increased from 9% in 1999–2000 to 23% in 2009–2011 and NADCs were the leading cause of death by the end of the study period.9
Most information available on the incidence of cancer in the HIV-infected population is from high-income countries, particularly the USA, Canada, Switzerland, France and Italy. In Spain, observational studies on malignancies in infected patients10 have been conducted and expert recommendations on the clinical management of NADCs11 have been published, but estimates of total cancer burden or types of cancer in people living with HIV are still not available. Being aware of the incidence of cancer and the distribution of malignancies among this population is important from a public health point of view in order to be able to plan prevention and early diagnosis strategies and thus improve the health outcomes of HIV-infected people in our country.
The aim of this study is to estimate the incidence of cancer in HIV-infected patients in Spain and to study trends from 2004 to 2015 by analysing data from the Spanish AIDS Research Network (CoRIS) cohort and comparing such data with the general population in Spain, estimated from data of the Spanish Cancer Registry Network (REDECAN).
MethodsStudy population and data collectionCoRIS records and REDECAN information have been analysed for this study. The CoRIS database includes clinical, demographic and biological characteristics of HIV-infected patients and various types of clinical events.12 The REDECAN web portal provides information on the incidence of the most common malignancies affecting the Spanish population.
CoRIS is a prospective, open, multicentre cohort of patients diagnosed with HIV infection at HIV/AIDS units of the Spanish Health System who have not received ART and was launched in 2004.12 Up until 30 November 2015, the date when the database was closed for project analysis, a total of 12,239 patients from 34 sites belonging to 13 autonomous communities (Andalusia, Aragon, Asturias, Balearic Islands, Canary Islands, Catalonia, Valencia, Galicia, La Rioja, Madrid, Murcia, Navarre and Basque Country) had been included in CoRIS. Changes in immunological and virological data, treatment and clinical events are updated each year. All diseases from the CDC/WHO 1993 classification of AIDS-defining events and non-AIDS events are included: cardiovascular, renal, hepatic, bone, metabolic, psychiatric and neoplasms not included in the AIDS-defining diseases section.13 Follow-up of each patient finishes when the patient dies or moves to another follow-up site that is not a member of the cohort.
The REDECAN network is the cooperative board of the population-based cancer registries and is one of the main cancer information systems in Spain. It contains data from Albacete, Asturias, Canary Islands, Ciudad Real, Valencia, Cuenca, Gerona, Granada, La Rioja, Majorca, Murcia, Navarra, Basque Country and Tarragona. It was created at the end of 2010 and combines case notification with the active collection of data from primary data sources, generally medical records, to identify and confirm registrable cases of cancer. The REDECAN portal provides data on the incidence of cancer in 2012, 2014 and 2015. Both CoRIS and REDECAN comply with Spanish and European data protection and confidentiality regulations.
Classification of neoplasmsFor the analyses, malignant neoplasms classified according to the International Classification of Diseases, Ninth Revision (ICD-9) were included and grouped according to epidemiological criteria, distinguishing initially between ADCs and NADCs. NADCs were also divided into virus-related and non-virus-related. The ADCs included Kaposi's sarcoma, non-Hodgkin's lymphoma and cervical cancer (excluding cancer affecting other parts of the uterus). The group of virus-related NADCs included liver cancer, anal cancer, head and neck cancer, penile cancer and Hodgkin's lymphoma. The group of non-virus-related NADCs included lung cancer, breast cancer, colorectal cancer (including cases recorded as colon cancer and as rectal cancer), prostate cancer, cancer of the uterus (excluding cervical cancer) and other malignant tumours not included in any of the previous types of cancer. Cases recorded with a diagnosis of cancer or “metastasis”, in which the specific type of neoplasm was unknown, were classified as “undetermined malignancies”. These cases were only taken into account to calculate the overall incidence of cancer.
Statistical analysesEstimated incidence of cancer in HIV-infected people and time trendsIn order to estimate the incidence of cancer in HIV-infected people of the CoRIS cohort, only incident cases diagnosed four months or more after entry into the cohort were included. Cases with any prior diagnosis and those diagnosed within the first 3 months were excluded as these were considered prevalent cases. The incidence rate was calculated as the number of cancer cases divided by the number of persons-follow-up time. The follow-up period was calculated from the day of entry into the cohort to the date of cancer diagnosis, death, loss to follow-up or 30 November 2015, whichever occurred first.
In order to estimate the trend in cancer incidence, the total follow-up time was divided into two 6-year periods: 2004–2009 (from January 1, 2004 to December 31, 2009) and 2010–2015 (From January 1, 2010 to November 30, 2015). The incidence rates for the two periods were compared and the incidence rate ratio was calculated.
Estimated risk of cancer in HIV-infected people compared to the general population in SpainThe incidence of cancer among CoRIS patients was compared with the incidence of cancer in the general population in Spain in 2010–2015 to estimate the relative risk of cancer in HIV-infected people; the incidence rate ratio was then calculated. The incidence of cancer among the general population in Spain in 2010–2015 was estimated from data available in REDECAN. Since this database only contained data from 2012, 2014 and 2015, a linear regression of the incidence rate over time was calculated and the prognosis of this regression was used as the estimated incidence among the general population. In order to compare the incidence among HIV-infected people and the general population in Spain, a normal distribution-based asymptotic p-value was used. If the p-value was less than 0.05, it was considered statistically significant.
To calculate incidence rates, rates were standardised using the European Standard Population, by separately calculating the incidence rate for each age group and then multiplying that number by the specific weight given according to the standardisation criterion.
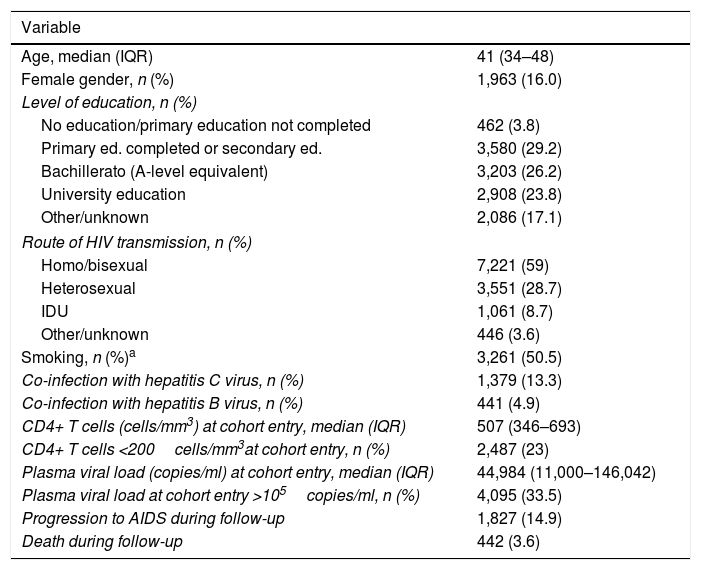
ResultsBetween 1 January 2004 and 30 November 2015, 12,239 patients (48,120 person-years) were included in CoRIS. Their general characteristics are described in Table 1. The median age of the patients included was 41 years and 84% were male. 88% had been infected as a result of sexual relations and 50% were smokers.
General characteristics of patients included in the CoRIS cohort between 2004 and 2015 (n=12,239).
| Variable | |
|---|---|
| Age, median (IQR) | 41 (34–48) |
| Female gender, n (%) | 1,963 (16.0) |
| Level of education, n (%) | |
| No education/primary education not completed | 462 (3.8) |
| Primary ed. completed or secondary ed. | 3,580 (29.2) |
| Bachillerato (A-level equivalent) | 3,203 (26.2) |
| University education | 2,908 (23.8) |
| Other/unknown | 2,086 (17.1) |
| Route of HIV transmission, n (%) | |
| Homo/bisexual | 7,221 (59) |
| Heterosexual | 3,551 (28.7) |
| IDU | 1,061 (8.7) |
| Other/unknown | 446 (3.6) |
| Smoking, n (%)a | 3,261 (50.5) |
| Co-infection with hepatitis C virus, n (%) | 1,379 (13.3) |
| Co-infection with hepatitis B virus, n (%) | 441 (4.9) |
| CD4+ T cells (cells/mm3) at cohort entry, median (IQR) | 507 (346–693) |
| CD4+ T cells <200cells/mm3at cohort entry, n (%) | 2,487 (23) |
| Plasma viral load (copies/ml) at cohort entry, median (IQR) | 44,984 (11,000–146,042) |
| Plasma viral load at cohort entry >105copies/ml, n (%) | 4,095 (33.5) |
| Progression to AIDS during follow-up | 1,827 (14.9) |
| Death during follow-up | 442 (3.6) |
CI: confidence interval; IDU: injecting drug users; IQR: interquartile range.
A total of 749 malignancies were diagnosed in 711 CoRIS patients, representing 5.81% of the people included in the cohort. Two tumours were reported in 38 individuals. A total of 411 cases who had been diagnosed prior to CoRIS entry or within the first 3 months were excluded, resulting in 338 incident cases. The overall incidence of cancer per 100,000 person-years (95% confidence interval [CI]) was 969.07 (652.96–1,285.17) in males and 353.68 (230.9–476.46) in females.
Of the 338 incident cases, 105 were diagnosed in 2004–2009 (13,725.81 person-years) and 233 were diagnosed in 2010–2015 (34,394.49 person-years), giving a gross incidence rate (95% CI) of 765.02 (625.72–926.11) and 677.44 (593.23–770.23), respectively. Standardised incidence rates (95% CI) were 952.26 (665.09–1239.42) and 871.69 (596.58–1146.80), respectively. On comparing the two periods, no significant differences in the overall incidence of cancer in CoRIS were observed (standardised incidence ratio [SIR]; 95% CI: 0.91; 0.8–1.05; p=0.18).
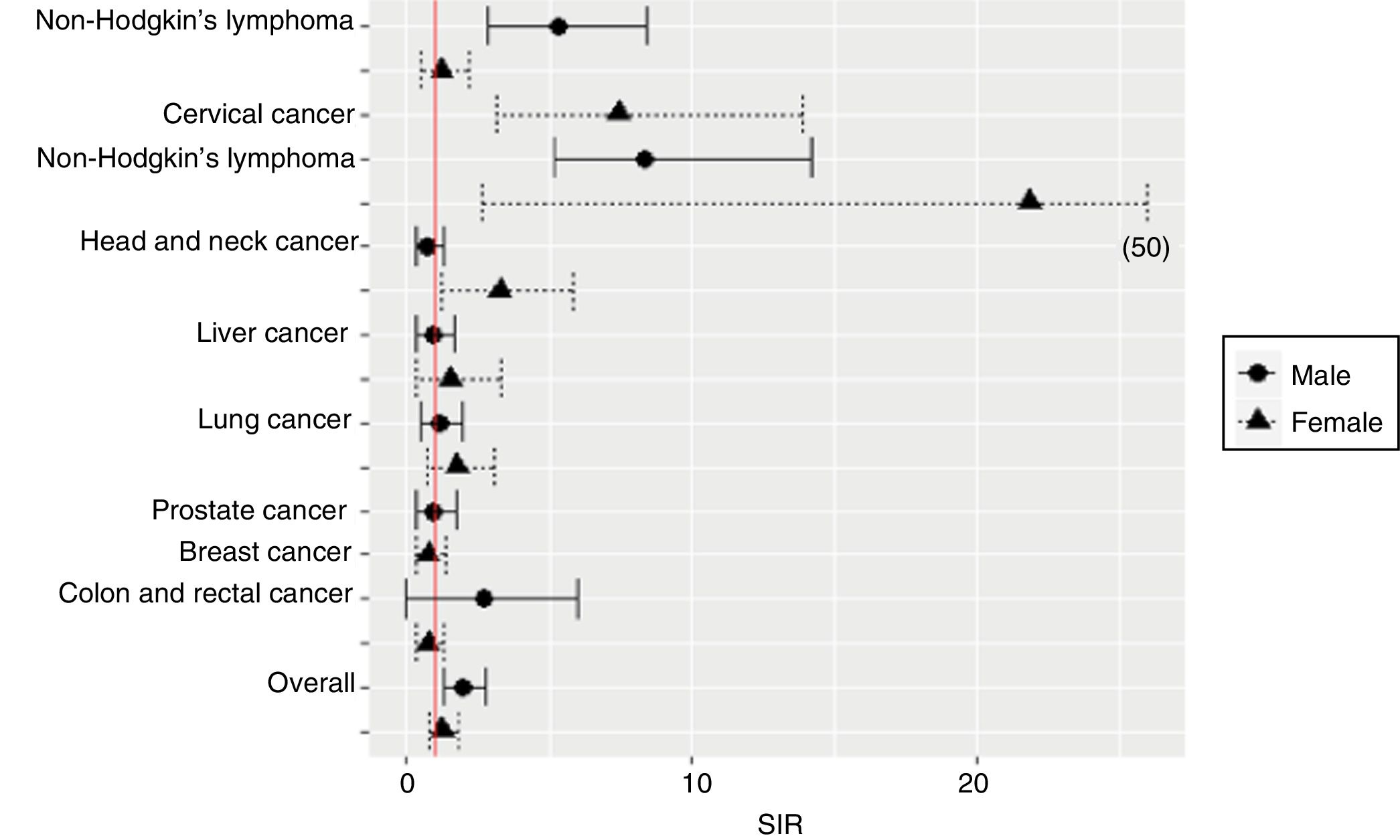
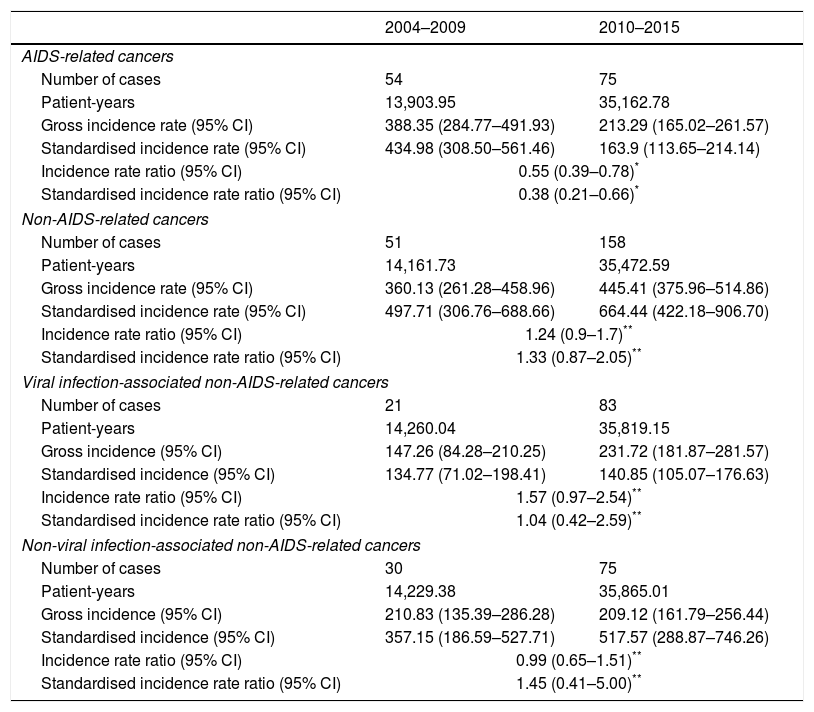
38.2% of the malignancies were ADCs and 61.8% were NADCs. The incidence rates of ADCs and NADCs in each period are shown in Table 2. The ten most common cancers were: cervical cancer, Kaposi's sarcoma, anal cancer, non-Hodgkin's lymphoma, breast cancer, Hodgkin's lymphoma, lung cancer, prostate cancer, liver cancer and colorectal cancer. The incidence rates of these cancers in males and in females are shown in Table 3 and Fig. 1.
Incidence of AIDS-defining cancers and non-AIDS-defining cancers in CoRIS in 2004–2009 and 2010–2015.
| 2004–2009 | 2010–2015 | |
|---|---|---|
| AIDS-related cancers | ||
| Number of cases | 54 | 75 |
| Patient-years | 13,903.95 | 35,162.78 |
| Gross incidence rate (95% CI) | 388.35 (284.77–491.93) | 213.29 (165.02–261.57) |
| Standardised incidence rate (95% CI) | 434.98 (308.50–561.46) | 163.9 (113.65–214.14) |
| Incidence rate ratio (95% CI) | 0.55 (0.39–0.78)* | |
| Standardised incidence rate ratio (95% CI) | 0.38 (0.21–0.66)* | |
| Non-AIDS-related cancers | ||
| Number of cases | 51 | 158 |
| Patient-years | 14,161.73 | 35,472.59 |
| Gross incidence rate (95% CI) | 360.13 (261.28–458.96) | 445.41 (375.96–514.86) |
| Standardised incidence rate (95% CI) | 497.71 (306.76–688.66) | 664.44 (422.18–906.70) |
| Incidence rate ratio (95% CI) | 1.24 (0.9–1.7)** | |
| Standardised incidence rate ratio (95% CI) | 1.33 (0.87–2.05)** | |
| Viral infection-associated non-AIDS-related cancers | ||
| Number of cases | 21 | 83 |
| Patient-years | 14,260.04 | 35,819.15 |
| Gross incidence (95% CI) | 147.26 (84.28–210.25) | 231.72 (181.87–281.57) |
| Standardised incidence (95% CI) | 134.77 (71.02–198.41) | 140.85 (105.07–176.63) |
| Incidence rate ratio (95% CI) | 1.57 (0.97–2.54)** | |
| Standardised incidence rate ratio (95% CI) | 1.04 (0.42–2.59)** | |
| Non-viral infection-associated non-AIDS-related cancers | ||
| Number of cases | 30 | 75 |
| Patient-years | 14,229.38 | 35,865.01 |
| Gross incidence (95% CI) | 210.83 (135.39–286.28) | 209.12 (161.79–256.44) |
| Standardised incidence (95% CI) | 357.15 (186.59–527.71) | 517.57 (288.87–746.26) |
| Incidence rate ratio (95% CI) | 0.99 (0.65–1.51)** | |
| Standardised incidence rate ratio (95% CI) | 1.45 (0.41–5.00)** | |
Rates expressed as 100,000persons/year.
95% CI: 95% confidence interval.
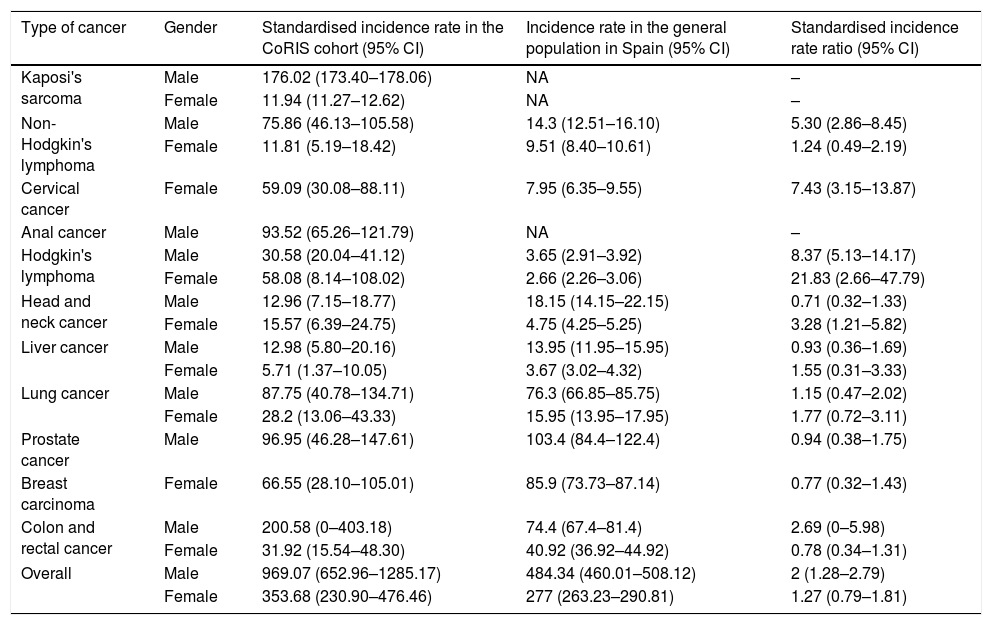
Incidence rates of malignancies in HIV-infected patients included in CoRIS and in the general population in Spain during 2010–2015.
| Type of cancer | Gender | Standardised incidence rate in the CoRIS cohort (95% CI) | Incidence rate in the general population in Spain (95% CI) | Standardised incidence rate ratio (95% CI) |
|---|---|---|---|---|
| Kaposi's sarcoma | Male | 176.02 (173.40–178.06) | NA | – |
| Female | 11.94 (11.27–12.62) | NA | – | |
| Non-Hodgkin's lymphoma | Male | 75.86 (46.13–105.58) | 14.3 (12.51–16.10) | 5.30 (2.86–8.45) |
| Female | 11.81 (5.19–18.42) | 9.51 (8.40–10.61) | 1.24 (0.49–2.19) | |
| Cervical cancer | Female | 59.09 (30.08–88.11) | 7.95 (6.35–9.55) | 7.43 (3.15–13.87) |
| Anal cancer | Male | 93.52 (65.26–121.79) | NA | – |
| Hodgkin's lymphoma | Male | 30.58 (20.04–41.12) | 3.65 (2.91–3.92) | 8.37 (5.13–14.17) |
| Female | 58.08 (8.14–108.02) | 2.66 (2.26–3.06) | 21.83 (2.66–47.79) | |
| Head and neck cancer | Male | 12.96 (7.15–18.77) | 18.15 (14.15–22.15) | 0.71 (0.32–1.33) |
| Female | 15.57 (6.39–24.75) | 4.75 (4.25–5.25) | 3.28 (1.21–5.82) | |
| Liver cancer | Male | 12.98 (5.80–20.16) | 13.95 (11.95–15.95) | 0.93 (0.36–1.69) |
| Female | 5.71 (1.37–10.05) | 3.67 (3.02–4.32) | 1.55 (0.31–3.33) | |
| Lung cancer | Male | 87.75 (40.78–134.71) | 76.3 (66.85–85.75) | 1.15 (0.47–2.02) |
| Female | 28.2 (13.06–43.33) | 15.95 (13.95–17.95) | 1.77 (0.72–3.11) | |
| Prostate cancer | Male | 96.95 (46.28–147.61) | 103.4 (84.4–122.4) | 0.94 (0.38–1.75) |
| Breast carcinoma | Female | 66.55 (28.10–105.01) | 85.9 (73.73–87.14) | 0.77 (0.32–1.43) |
| Colon and rectal cancer | Male | 200.58 (0–403.18) | 74.4 (67.4–81.4) | 2.69 (0–5.98) |
| Female | 31.92 (15.54–48.30) | 40.92 (36.92–44.92) | 0.78 (0.34–1.31) | |
| Overall | Male | 969.07 (652.96–1285.17) | 484.34 (460.01–508.12) | 2 (1.28–2.79) |
| Female | 353.68 (230.90–476.46) | 277 (263.23–290.81) | 1.27 (0.79–1.81) |
Rates expressed as 100,000persons/year.
95% CI: 95% confidence interval.
In comparison with the 2004–2009 period, a significant decline in the incidence of ADCs was observed in 2010–2015 (SIR; 95% CI: 0.38; 0.21–0.66; p<0.0001). Therefore, in the more recent period, the standardised incidence of NADCs was 4 times higher than the standardised incidence of ADCs (Table 2).
No significant differences in the overall incidence of viral infection-related and non-viral infection-related NADCs were observed between the 2 periods (Table 2).
Estimated risk of cancer in HIV-infected people compared to the general population in SpainIn 2010–2015, the standardised incidence rates (95% CI) of ADCs and NADCs per 100,000 person-years were 163.90 (113.65–214.14) and 664.44 (422.28–906.70), respectively. Compared with the general population in Spain, in 2010–2015, the overall incidence of cancer was two times higher in HIV-infected men than in men not infected with HIV (Table 3). Significantly higher relative risks were documented for non-Hodgkin's and Hodgkin's lymphoma, cervical cancer and head and neck cancer (Table 3 and Fig. 1). The risk (SIR; 95% CI) of Hodgkin's lymphoma was higher in HIV-infected people of both genders (males: 8.38; 5.13–14.17; females: 21.83; 2.66–47.79), while the risk of non-Hodgkin's lymphoma was higher in males (5.30; 2.86–8.45). HIV-infected females were at a higher risk of cervical cancer (SIR; 95% CI: 7.43; 3.15–13.87) and head and neck cancer (SIR; 95% CI: 3.28; 1.21–5.82) (Table 3).
DiscussionThis is the first national study on the incidence of cancer in HIV-infected people in Spain. The data observed are in line with other contemporary cohorts that have analysed trends in cancer diagnosis following increased use of ART and have stated that the incidence of malignancies is higher in HIV-infected people than among the general population and a gradual reduction in the frequency of ADCs is occurring, with a predominance of non-AIDS-defining cancers currently observed.1,14,15
Although this study has confirmed a significant decline in ADCs, the risk of non-Hodgkin's lymphoma and cervical cancer in the more recent period is still much higher in HIV-infected patients than among the general population. Earlier diagnosis and treatment of HIV infection are expected to reduce immunological damage and help decrease the incidence of ADCs further over the next few years.
There are discrepancies regarding the impact of ART on NADCs.16–19 Although an increased incidence of NADCs has been observed during the ART era in some cohorts14 and receiving ART has been reported to reduce the risk of NADCs and is associated with a more favourable clinical outcome,18 variable standardised incidence rate have been reported for various NADCs: from increases to declines.19 In the HIV/AIDS Cancer Match Study, a progressive increase in the incidence of anal cancer, liver cancer and prostate cancer was observed between 1996 and 2010, while there was a decline in lung cancer and no change in breast cancer and colorectal cancer rates over time.1 In the D:A:D Study, the incidence of NADCs did not change substantially between 2004 and 2010 after adjusting for age.20 The three most common cancers were lung cancer, Hodgkin's lymphoma and anal cancer. No upward or downward trend in the incidence of these three cancers was observed.
In this study, the incidence of the various types of cancer from 2004 to 2015 was analysed, and no significant differences in the overall incidence of NADCs over time were documented. During the more recent period, 2010–2015, the incidence of non-viral infection-related NADCs was higher than the incidence of viral infection-related NADCs, and the highest incidence rates observed were for lung, prostate, colorectal and breast cancer. Unlike prostate and breast cancer, the incidence rates for lung cancer and colorectal cancer tended to be higher among HIV-infected patients than among the general population in Spain, although the differences were not statistically significant. These cancers are among the most common in HIV-infected patients;1 lung cancer, in particular, is the most common NADC and is a major cause of morbidity and mortality in HIV-infected people.8 Lung cancer is closely linked to cigarette smoking and there is a very high prevalence of tobacco use among HIV-infected people.21,22 However, HIV infection itself may also increase susceptibility to lung cancer through various mechanisms, including impaired immune surveillance and an associated pulmonary and systemic proinflammatory state.22
50% of HIV-infected patients included in this study were smokers, a similar percentage to that reported in previous studies based on CoRIS23 and other cohorts of HIV-infected people living in high-income western countries,22,24 which is twice the prevalence of smoking among non-HIV-infected individuals.25 Therefore, smoking cessation strategies must be prioritised to reduce the risk of lung cancer. It has been documented that the incidence of lung cancer among HIV-infected patients is still very high five years after smoking cessation, indicating that the oncogenic potential of smoking may remain for a much longer period and surveillance is required years after quitting smoking.22
The most common viral infection-related NADC was Hodgkin's lymphoma, followed by anal cancer, head and neck cancer and liver cancer. With regard to the general population, a higher relative risk of Hodgkin's lymphoma in HIV-infected people of both genders and a higher risk of head and neck cancer in women were documented. The higher risk of Hodgkin's lymphoma, an Epstein-Barr virus-related neoplasm, was an expected finding, in line with other cohorts.15 The high incidence of anal cancer and head and neck cancer observed in CoRIS patients is consistent with prior studies conducted in this same cohort. These studies had revealed a high frequency of high-risk human papillomavirus infections26 involved in the development of anal and oropharyngeal cancer. As in other cohorts,2 the incidence of anal cancer was higher than the incidence of head and neck cancer, a finding that may be related to the different prevalence of anal and oral infection with high-risk human papillomavirus genotypes27 and anatomical site.
Liver cancer was the fourth most common viral infection-related NADC and accounted for 5.48% of all NADCs. The incidence rate observed was lower than that described in France between 2005 and 200928 and, unlike other studies, its incidence was not higher than that of the general population.1,19,6 The lower incidence of liver cancer observed in CoRIS patients may be partly due to the fact that CoRIS is a contemporary cohort with a declining prevalence of HCV co-infection29 and to recent improvements in antiviral therapy for hepatitis C.
The main limitations of the study are due to the low incidence of many of the cancers studied, which limits the accuracy of the estimates. Despite being a national study with 10 years of follow-up, the number of incident cases was often inadequate to reach firm conclusions regarding time trends and the relative risk for the general population. Although CoRIS is a prospective cohort with strict quality controls, the participating sites are entirely responsible for reporting all cases and therefore cases may have been underreported.
There are no official data on the incidence of cancer in Spain expressed on an ongoing, annual basis throughout our study period. REDECAN was created at the end of 2010 and has published data on cancer incidence and survival rates in Spain in 2012, 2014 and 2015. Therefore, a linear regression was required to calculate the incidence of the general population. Another limitation of the REDECAN records is the fact that it contains no data on the incidence of uncommon cancers among the general population, such as Kaposi's sarcoma or anal cancer, which has hindered estimates of the relative risk of these cancers. It is also a registry that only includes data from provinces in 11 autonomous communities of Spain, and although a lot of the data are consistent with the data included in the CoRIS cohort, this is not always the case. This difference between the two registries is a limitation when comparing the populations, particularly in cancers with incidence rates that may vary according to geographical area.
To conclude, the overall incidence of cancer in HIV-infected people included in the CoRIS cohort is higher than that of the general population in Spain. The relative risk of malignancies is higher for various cancers, including Hodgkin's and non-Hodgkin's lymphoma, cervical cancer and head and neck cancer. The incidence of AIDS-related cancers continues to decline and non-AIDS-related cancers are currently more prevalent, with an incidence that is 4 times higher than AIDS-related cancers. These data indicate that additional efforts focusing on the prevention and early detection of cancer in HIV-infected patients in Spain must be made.
FundingThe RIS cohort (CoRIS) is funded by ISCIII through the Red Temática de Investigación Cooperativa en Sida (Network of AIDS Research Centres) (RD06/0006/0027; RD12/0017/0023 and RD16/0025/0038) as part of the National R & D + I Plan co-funded by the European Regional Development Fund (ERDF). The authors of this study have received funding from the ISCIII-National R & D + I Plan (FIS: PI08/893, PI13/02256, PI16/01740, PI18/01861; research activity intensification agreement INT 14/00207; Río Hortega agreement CM15/00187) and FISABIO (UGP-14-197 and predoctoral agreement UGP-15-152).
Conflicts of interestThe authors declare that they have no conflicts of interest.
This study would not have been possible without the assistance of all the patients, medical and nursing staff and data administrators who participated in the project (see Annex I).
See Annex I with the list of all participating centers and researchers.
Please cite this article as: García-Abellán J, del Río L, García JA, Padilla S, Vivancos MJ, del Romero J, et al. Riesgo de cáncer en personas con VIH en España, 2004-2015. Estudio de la cohorte CoRIS. Enferm Infecc Microbiol Clin. 2019;37:502–508.