In the pre-vaccine era, Haemophilus influenzae (Hi) was the second leading cause of pneumonia, septicaemia and bacterial meningitis in children under five years of age1. Its incidence decreased dramatically in Spain following the introduction of the Hi conjugate vaccine in 2001. The vaccines available in Spain use polysaccharide polyribosylribitol phosphate, most of which is conjugated to tetanus toxoid2.
We report the case of a healthy nine-month-old infant who was fully vaccinated for her age, having received two doses of the Hi conjugate vaccine (two and four months). She was brought to accident and emergency following 48 h of fever associated with vomiting, lack of energy and refusal to feed. She exhibited a poor general condition, with decreased muscle tone and strength, without rash or petechiae. Laboratory testing revealed 25,890 leukocytes/mm3 with neutrophils 83%, elevated C-reactive protein (161.9 mg/l) and elevated procalcitonin (49.03 ng/mL). Her cerebrospinal fluid was cloudy, with 2460 cells/mm3 (95% polymorphonuclear leukocytes) and decreased CSF glucose (19 mg/dL). Treatment was started with cefotaxime, vancomycin and dexamethasone. Hi serotype b (Hib) was isolated from blood culture and cerebrospinal fluid culture. She had persistent fever. Magnetic resonance imaging (MRI) revealed bifrontal, millimetric subdural empyemas. Asplenia was ruled out by abdominal ultrasound. Assessment by Otolaryngology and Neurology ruled out hearing and neurological problems. The patient became afebrile on her 12th day of hospitalisation. Four weeks of intravenous antibiotic therapy were completed.
An immunological study revealed low anti-pneumococcal IgG titres. All other tests, including lymphocyte subpopulations, expression of human leukocyte antigen (HLA) class i and ii molecules, mitogen proliferation, immunoglobulins, response to tetanus vaccination and CH50, were normal. The patient followed a favourable course after discharge, with normal psychomotor development and auditory evoked potentials. MRI at seven weeks revealed complete resolution of the patient's empyemas.
The patient had invasive Hib disease as defined by the European Centre for Disease Prevention and Control, which includes cases of systemic infection with isolation of Hi or detection of Hi nucleic acids from a normally sterile site3.
In this case study, the patient developed septicaemia and meningitis despite being fully vaccinated for her age, representing a true vaccine failure (TVF). This is defined as detection of invasive Hib disease at least two weeks after administering a vaccine dose in infants over one year of age, or at least one week after administering two or more vaccine doses in infants under one year of age4,5, as in this patient.
The incidence of TVF in Hib is very low and has been associated with various factors: prematurity, immunological abnormalities (including humoral immunodeficiencies, delayed maturation of the immune system with low-for-age immunoglobulins and low avidity of anti-polyribosylribitol phosphate antibodies), technical reasons (vaccine administration and/or storage errors, use of different transport proteins), persistent circulation of the microorganism in the community, mobility of populations with imported cases and the influence of genetic and racial factors5–9. In our case, the immunological study was normal, and we did not identify any other causal factor of TVF, although avidity of anti-polyribosylribitol phosphate antibodies could not be studied as the test is not currently available in Spain.
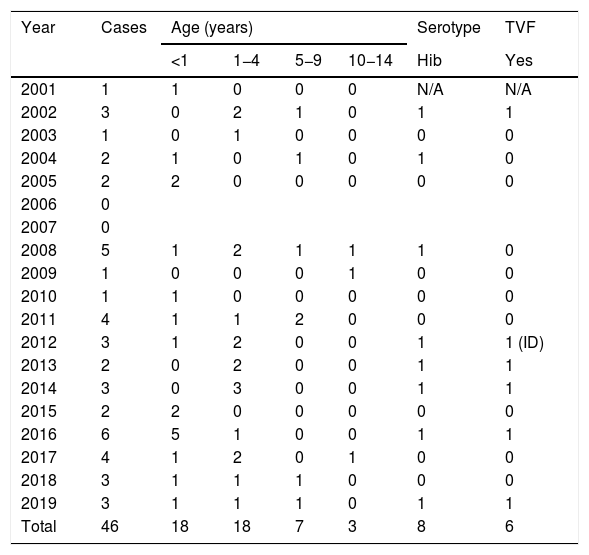
We conducted a review of all cases of invasive Hi disease recorded in the Autonomous Community of Madrid between 2001 and 201910. We identified 202 cases, 156 in adults and 46 in children (Table 1). In total, 78% of the paediatric cases (36/46) affected children under five years of age, eight cases were caused by Hib (17.4%) and six cases, five of which occurred in the last eight years, met criteria for TVF. This amounts to an annual incidence of 0.254 cases of invasive Hi disease and 0.044 cases of invasive Hib disease per 100,000 population in children under 14 years of age.
Summary of cases of invasive Haemophilus influenzae disease in children under the 14 years of age in the Autonomous Community of Madrid from 2001 to 2019.
| Year | Cases | Age (years) | Serotype | TVF | |||
|---|---|---|---|---|---|---|---|
| <1 | 1−4 | 5−9 | 10−14 | Hib | Yes | ||
| 2001 | 1 | 1 | 0 | 0 | 0 | N/A | N/A |
| 2002 | 3 | 0 | 2 | 1 | 0 | 1 | 1 |
| 2003 | 1 | 0 | 1 | 0 | 0 | 0 | 0 |
| 2004 | 2 | 1 | 0 | 1 | 0 | 1 | 0 |
| 2005 | 2 | 2 | 0 | 0 | 0 | 0 | 0 |
| 2006 | 0 | ||||||
| 2007 | 0 | ||||||
| 2008 | 5 | 1 | 2 | 1 | 1 | 1 | 0 |
| 2009 | 1 | 0 | 0 | 0 | 1 | 0 | 0 |
| 2010 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| 2011 | 4 | 1 | 1 | 2 | 0 | 0 | 0 |
| 2012 | 3 | 1 | 2 | 0 | 0 | 1 | 1 (ID) |
| 2013 | 2 | 0 | 2 | 0 | 0 | 1 | 1 |
| 2014 | 3 | 0 | 3 | 0 | 0 | 1 | 1 |
| 2015 | 2 | 2 | 0 | 0 | 0 | 0 | 0 |
| 2016 | 6 | 5 | 1 | 0 | 0 | 1 | 1 |
| 2017 | 4 | 1 | 2 | 0 | 1 | 0 | 0 |
| 2018 | 3 | 1 | 1 | 1 | 0 | 0 | 0 |
| 2019 | 3 | 1 | 1 | 1 | 0 | 1 | 1 |
| Total | 46 | 18 | 18 | 7 | 3 | 8 | 6 |
ID: immunodeficiency; Hib: Haemophilus influenzae type b; N/A: not available; TVF: true vaccine failure.
In conclusion, although the Hib conjugate vaccine is highly effective, TVF can still occur5. In patients in whom it occurs, a full evaluation, including an immunological study, is recommended2. However, in most patients, no underlying humoral immunodeficiency can be identified6 and the cause of vaccine failure cannot be established. This was true in our case and in all cases recorded in the Autonomous Community of Madrid over the last two decades.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: López López S, del Rosal T, Jiménez Bueno S, Baquero-Artigao F. Sepsis y meningitis por Haemophilus influenzae tipo b tras fallo vacunal. Enferm Infecc Microbiol Clin. 2021;39:417–418.