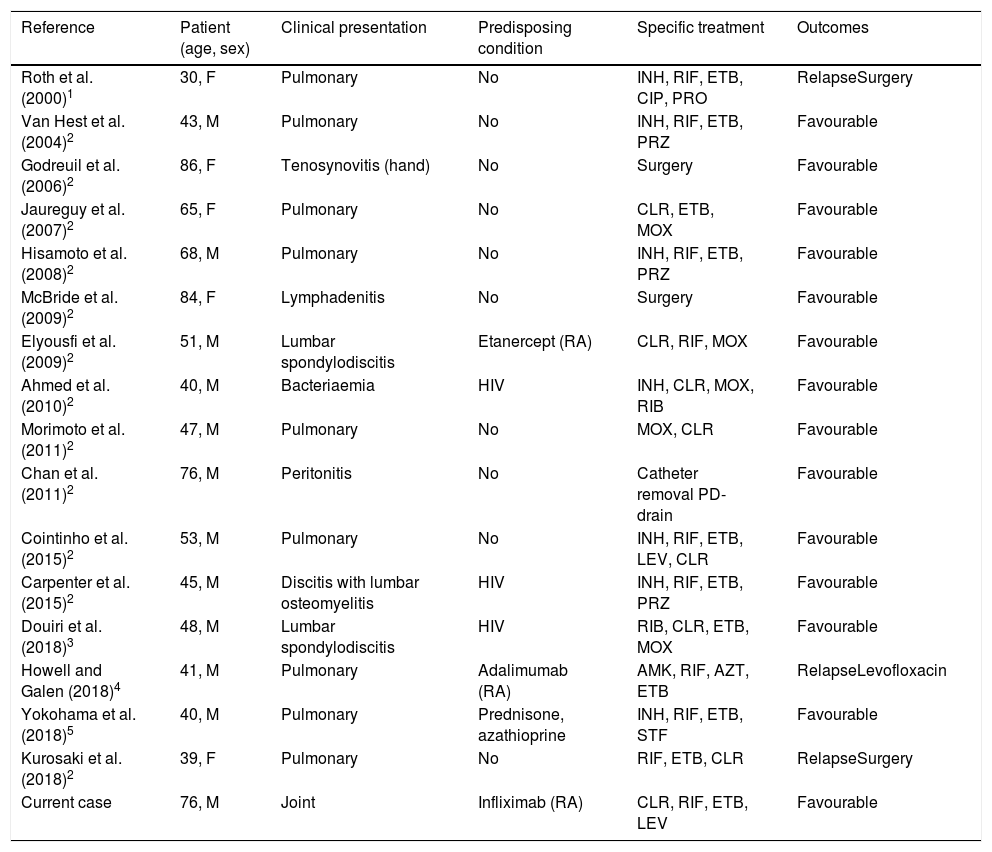
Mycobacterium heckeshornense is a slow-growing, scotochromogenic non-tuberculous mycobacterium, first isolated in a sputum sample from an immunocompetent female in the year 2000.1 There are few documented episodes in the literature related to M. heckeshornense with sporadic cases of pulmonary involvement, tenosynovitis, lymphadenitis, spondylodiscitis, bacteraemia and peritonitis having been published since that first study2–5 (Table 1), adding to a total of 16 patients. We present a case of joint affectation in a patient with rheumatoid arthritis treated with infliximab and methotrexate. To our knowledge, it is the first in which this mycobacterium has been isolated in a joint fluid sample.
Summary of cases of documented infections by M. heckeshornense.
| Reference | Patient (age, sex) | Clinical presentation | Predisposing condition | Specific treatment | Outcomes |
|---|---|---|---|---|---|
| Roth et al. (2000)1 | 30, F | Pulmonary | No | INH, RIF, ETB, CIP, PRO | RelapseSurgery |
| Van Hest et al. (2004)2 | 43, M | Pulmonary | No | INH, RIF, ETB, PRZ | Favourable |
| Godreuil et al. (2006)2 | 86, F | Tenosynovitis (hand) | No | Surgery | Favourable |
| Jaureguy et al. (2007)2 | 65, F | Pulmonary | No | CLR, ETB, MOX | Favourable |
| Hisamoto et al. (2008)2 | 68, M | Pulmonary | No | INH, RIF, ETB, PRZ | Favourable |
| McBride et al. (2009)2 | 84, F | Lymphadenitis | No | Surgery | Favourable |
| Elyousfi et al. (2009)2 | 51, M | Lumbar spondylodiscitis | Etanercept (RA) | CLR, RIF, MOX | Favourable |
| Ahmed et al. (2010)2 | 40, M | Bacteriaemia | HIV | INH, CLR, MOX, RIB | Favourable |
| Morimoto et al. (2011)2 | 47, M | Pulmonary | No | MOX, CLR | Favourable |
| Chan et al. (2011)2 | 76, M | Peritonitis | No | Catheter removal PD-drain | Favourable |
| Cointinho et al. (2015)2 | 53, M | Pulmonary | No | INH, RIF, ETB, LEV, CLR | Favourable |
| Carpenter et al. (2015)2 | 45, M | Discitis with lumbar osteomyelitis | HIV | INH, RIF, ETB, PRZ | Favourable |
| Douiri et al. (2018)3 | 48, M | Lumbar spondylodiscitis | HIV | RIB, CLR, ETB, MOX | Favourable |
| Howell and Galen (2018)4 | 41, M | Pulmonary | Adalimumab (RA) | AMK, RIF, AZT, ETB | RelapseLevofloxacin |
| Yokohama et al. (2018)5 | 40, M | Pulmonary | Prednisone, azathioprine | INH, RIF, ETB, STF | Favourable |
| Kurosaki et al. (2018)2 | 39, F | Pulmonary | No | RIF, ETB, CLR | RelapseSurgery |
| Current case | 76, M | Joint | Infliximab (RA) | CLR, RIF, ETB, LEV | Favourable |
AMK: amikacin; RA: rheumatoid arthritis; AZT: azithromycin; CIP: ciprofloxacin; CLR: clarithromycin; ETB: ethambutol; F: female; INH: isoniazid; LEV: levofloxacin; M: male; MOX: moxifloxacin; PRO: procainamide; RIB: rifabutin; RIF: rifampicin; PRZ: pyrazinamide; STF: sitafloxacin; HIV: human immunodeficiency virus.
76-year-old male patient, gardener, diagnosed with non-erosive rheumatoid arthritis in 1996, positive rheumatoid factor and negative anti-citrullinated peptide antibody (ACPA). He received initial treatment with gold salts, discontinued due to ineffectiveness, and has been on methotrexate since 2002. Over the course of the disease, the patient presents with several polyarticular outbreaks predominantly in the carpus and elbows that require corticosteroids in a decreasing regimen.
Due to poor control, treatment with prednisone 30mg is started in a decreasing regimen and with infliximab in combination with methotrexate 7.5mg weekly. Improvement of the joint symptoms occurs, but he presents with right elbow flexion continuously on physical examination, the presence of active synovitis being confirmed with joint ultrasound. Arthrocentesis is carried out on the right elbow with growth of M. heckeshornense in mycobacterial culture from the synovial fluid. Treatment with infliximab is discontinued, a chest X-ray is performed, which is normal, and empirical treatment with clarithromycin is started 500mg every 12h, rifampicin 600mg/24h, ethambutol 1200mg/24h and moxifloxacin 400mg/24h. A further arthrocentesis is carried out 2 months later, and the culture is negative. At 4 months ethambutol is discontinued, maintaining triple therapy for one year and the patient is asymptomatic after 10 months of follow-up.
The microbiological study of the sample included auramine staining, MGIT (Becton Dickinson, UK) culture, Löwenstein–Jensen solid medium culture (LJ) (Becton Dickinson, UK) and PCR for Mycobacterium tuberculosis complex (XpertMTB/Rif, Cepheid, Sunnyvale, CA, USA). Auramine staining and PCR were negative. The MGIT culture was positive 12 days after incubation, confirming the presence of acid-alcohol fast bacilli by Zhiel-Nielssen staining. The LJ medium culture could not be interpreted because it was contaminated. Identification by MALDI-TOF MS (Bruker Daltonics Inc., Germany) with a score of 1909 was M. heckeshornense. The strain was sent to the National Micobacteria Centre (Instituto Carlos III [Carlos III Institute], Majadahonda, Madrid) to confirm its identification by molecular methods and to carry out antibiotic susceptibility studies using the proportion method.
Identification was carried out through PRA of the hsp65 gene and digestion with BstEII and HaeIII enzymes. The pattern that was obtained was 3 bands 235/120/100 after digestion with the first enzyme and 3 other bands after digestion with HaeIII 160/105/60. This presumptive identification was confirmed by 16S rRNA gene sequencing. The strain with which 100% homology was presented in the GenBank was with the M. heckeshornense strain S369 (NR_028759), comparing 1360 pb. The antibiotic susceptibility test was carried out using MIC in solid medium; the strain was sensitive to cycloserine, ethionamide, rifampin, capreomycin, streptomycin and kanamycin, and resistant to ethambutol, isoniazid, PAS, pyrazinamide, TCH, and thiosemicarbazone.
Isolation of non-tuberculous mycobacteria in synovial fluid is unusual, preferentially occurring in immunosuppressed patients. In our case, as in the work of Yokohama et al.,5 identification by MALDI-TOF was conducted, which is why it can be considered a quick, cost-effective and accurate tool for the identification of M. heckeshornense. We presented a fifth case of osteoarticular involvement in addition to a case of tenosynovitis2 and 3 of spondylodiscitis.2,3 Males (4 cases) and the existence of any risk factor (2 HIV infections and 2 immunosuppressive treatment) predominated, and all achieved a cure. The association of biological drugs used in rheumatoid arthritis and the increased risk of serious infections provide controversial evidence. According to a meta-analysis published in TheLancet,6 biological medicines showed a significant increase in the risk of serious infections at usual doses compared to disease-modifying antirheumatic drugs (DMAD), with the combination of biological drugs presenting the highest risk.
Please cite this article as: Nicolás-de Blas R, Garijo-Bufort M, Nebreda-Mayoral T, Guerra-Laso JM. Sinovitis por Mycobacterium heckeshornense en paciente con artritis reumatoide en tratamiento con infliximab. Enferm Infecc Microbiol Clin. 2020;38:448–449.