Streptococcus equi (S. equi), subspecies zooepidemicus, is a micro-organism belonging to Lancefield group C beta-haemolytic streptococci. It is an opportunistic bacteria, particularly in horses, although it has also been isolated in cattle, pigs, rabbits and dogs.1 It can cause serious bacterial infections in humans such as septic arthritis, meningitis, pneumonia and endocarditis following contact with colonised or sick animals or due to consumption of their derivative products.2 We report the case of a previously healthy 12-year-old girl who presented with palpebral oedema and oedema in her legs for 48h plus gross haematuria. Two weeks earlier, she had presented with a throat infection, which was treated with oral amoxycillin for 10 days. She lives in a rural location and looks after horses; she also rides horses as a regular sporting activity. Physical examination revealed peripheral oedema, ascites, bilateral crackles and blood pressure 159/100 mmHg (95th percentile for the patient's age, gender and height 121/78mmHg). Blood testing yielded values consistent with acute renal failure (Table 1). A lung ultrasound confirmed bilateral pleural effusion. Streptococcus equi was isolated in a throat culture. She was treated with salt and water restriction, intravenous furosemide 2mg/kg/day/for 3 days and oral amlodipine 0.1mg/kg/day. Her condition followed a favourable course with improved kidney function (Table 1) and normal blood pressure (115/63mmHg) at discharge after 7 days of hospitalisation. She is currently continuing follow-up with outpatient appointments at the Paediatric Nephrology department with good kidney function, no haematuria or proteinuria and no anti-hypertensive treatment (amlodipine was stopped after two months had elapsed since she was admitted). S. equi is a nephritogenic toxin-producing bacteria, although it does not always produce haemolysin of the streptolysin O type, meaning that anti-streptolysin O (ASO) antibodies may not be elevated; in this way, it differs from other members of the genus Streptococcus. However, it does usually cause an increase in anti-DNase levels, which can be useful in its diagnosis. Microscopically, glomerular deposition of plasminogen receptor has been seen, which explains secondary nephritis.1 Most reported cases of acute glomerulonephritis (AGN) caused by S. equi have been in outbreaks in an adult population secondary to consumption of unpasteurised dairy products; there are few data on the link to horses seen in the case of our patient. Between December 1997 and July 1998, 253 cases (134 of which were microbiologically confirmed) of AGN caused by S. equi were reported in Nova Serrana (Brazil) following consumption of unpasteurised dairy products. In 94% of all the cases, the patients were over the age of 15. Regarding kidney function, 5 cases required dialysis during the acute phase. In the 5-year follow-up, 30% had persistent hypertension and 15% had some degree of chronic kidney disease (defined as a glomerular filtration rate below 60ml/min/1.73m2).3 Between December 2012 and February 2013, there was another similar outbreak in Monte Santo de Minas (Brazil) among 175 patients, 4 of whom required acute haemodialysis.4 To date, multiple cases of S. equi infection have been reported, primarily in the adult population; the infection is considered rare in the paediatric population. In the literature, we found a single isolated published case, in addition to the paediatric patients included in the above-mentioned outbreaks.5 Therefore, we find it interesting that our case is described as the first paediatric case reported in Spain, and that it also does not form part of any outbreak associated with consumption of unpasteurised products. Unlike S. pyogenes, AGN caused by S. equi is more commonly associated with hypertension and chronic kidney disease. Even so, with early detection and treatment, the prognosis is usually favourable as with our patient, although it should be highlighted that it started with a hypertensive crisis, which is very rare in AGN caused by other members of the Streptococcus genus. Therefore, we must highlight the importance of taking a medical history that covers consumption of unpasteurised products and contact with animals, particularly horses, which may be carriers of S. equi, in cases of acute post-infectious glomerulonephritis, since this will allow for suitable treatment with particular attention to the possible acute complications and long-term sequelae that may occur in these patients.
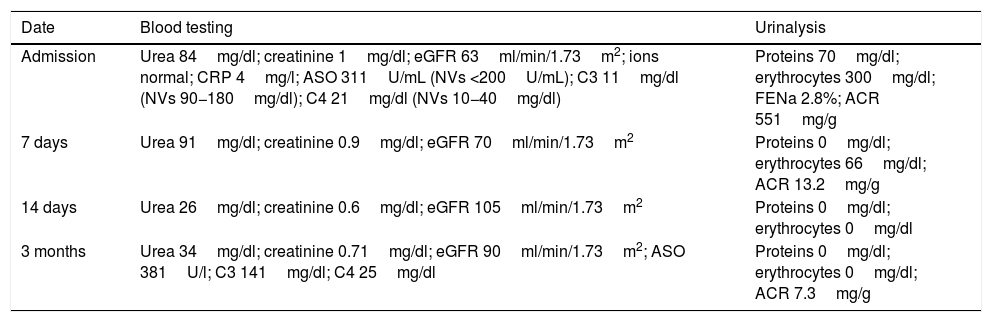
Changes in our patient’s laboratory results.
| Date | Blood testing | Urinalysis |
|---|---|---|
| Admission | Urea 84mg/dl; creatinine 1mg/dl; eGFR 63ml/min/1.73m2; ions normal; CRP 4mg/l; ASO 311U/mL (NVs <200U/mL); C3 11mg/dl (NVs 90−180mg/dl); C4 21mg/dl (NVs 10−40mg/dl) | Proteins 70mg/dl; erythrocytes 300mg/dl; FENa 2.8%; ACR 551mg/g |
| 7 days | Urea 91mg/dl; creatinine 0.9mg/dl; eGFR 70ml/min/1.73m2 | Proteins 0mg/dl; erythrocytes 66mg/dl; ACR 13.2mg/g |
| 14 days | Urea 26mg/dl; creatinine 0.6mg/dl; eGFR 105ml/min/1.73m2 | Proteins 0mg/dl; erythrocytes 0mg/dl |
| 3 months | Urea 34mg/dl; creatinine 0.71mg/dl; eGFR 90ml/min/1.73m2; ASO 381U/l; C3 141mg/dl; C4 25mg/dl | Proteins 0mg/dl; erythrocytes 0mg/dl; ACR 7.3mg/g |
ACR: albumin-to-creatinine ratio; ASO: a n ti -streptol ysin O; FENa: fractional excretion of sodium; eGFR: estimated glomerular filtration rate according to Schwartz’s formula (2009 update); NVs: normal values.
This study has received no specific funding from public, private or non-profit organisations.
Please cite this article as: Sánchez-Códez MI, Castellano-Martinez A, García-Ojanguren A, Rodríguez-González M. Glomerulonefritis aguda postinfecciosa por Streptococcus equi en paciente pediátrico. Enferm Infecc Microbiol Clin. 2021;39:50–51.