A 36-year-old male, from Romania, who has lived in Almería, Spain, since 2006, doing work related to agriculture (greenhouses) and later in hospitality (waiter). He lives with immunovirologically stable HIV-1 (category A1) with very good adherence to treatment and clinic appointments. Relevant history included syphilis of undetermined date that had been correctly treated, hepatitis A and B, as well as a perforated gastric ulcer treated with surgery and intra-abdominal hydatid cyst previously treated in 2008 in Romania. He was admitted to our centre in March 2021 due to back pain that had been treated on an outpatient basis for about four months with non-steroidal anti-inflammatory drugs, without improvement, and after undergoing an MRI that suggested the possibility of spondylodiscitis.
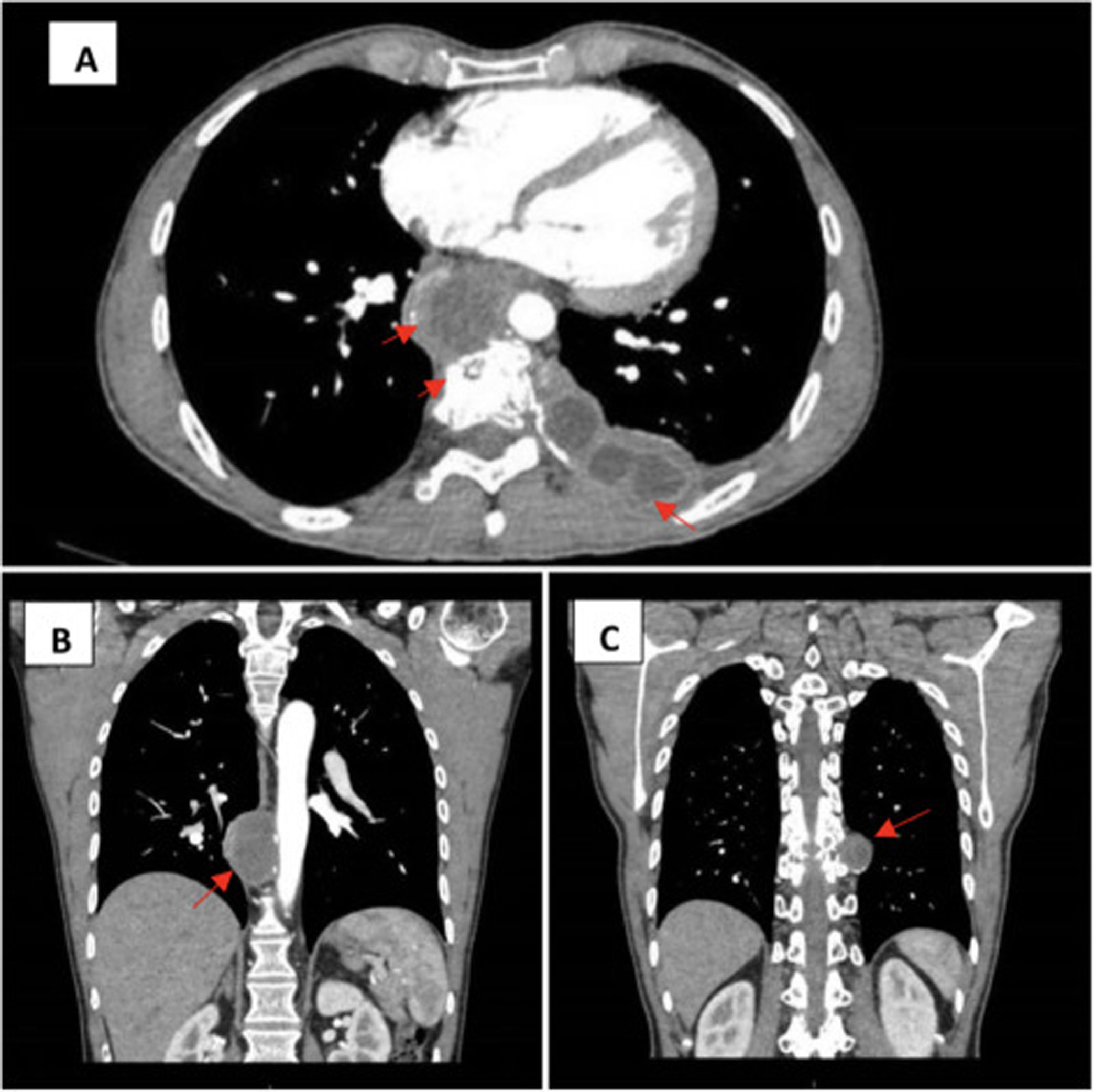
Physical examination revealed low back pain that worsened with movement and on palpation at the T10 level, with the patient afebrile at all times, with no data of haemodynamic instability or other relevant findings except for the scar from a previous laparotomy due to the aforementioned intervention in 2008. An imaging test was performed upon admission: computerised axial tomography (CAT) where collections with loculated content in peri- and paravertebral locations were observed, one of them causing the disappearance of the T9-T10 disc and erosion of vertebral bodies (Fig. 1).
Computerised axial tomography (CAT) with intravenous contrast. (A) Left para-aortic and paravertebral-subpleural collections with erosion of the vertebral body, transverse projection. (B) Para-aortic collection, longitudinal projection. (C) Left paravertebral collection, longitudinal projection.
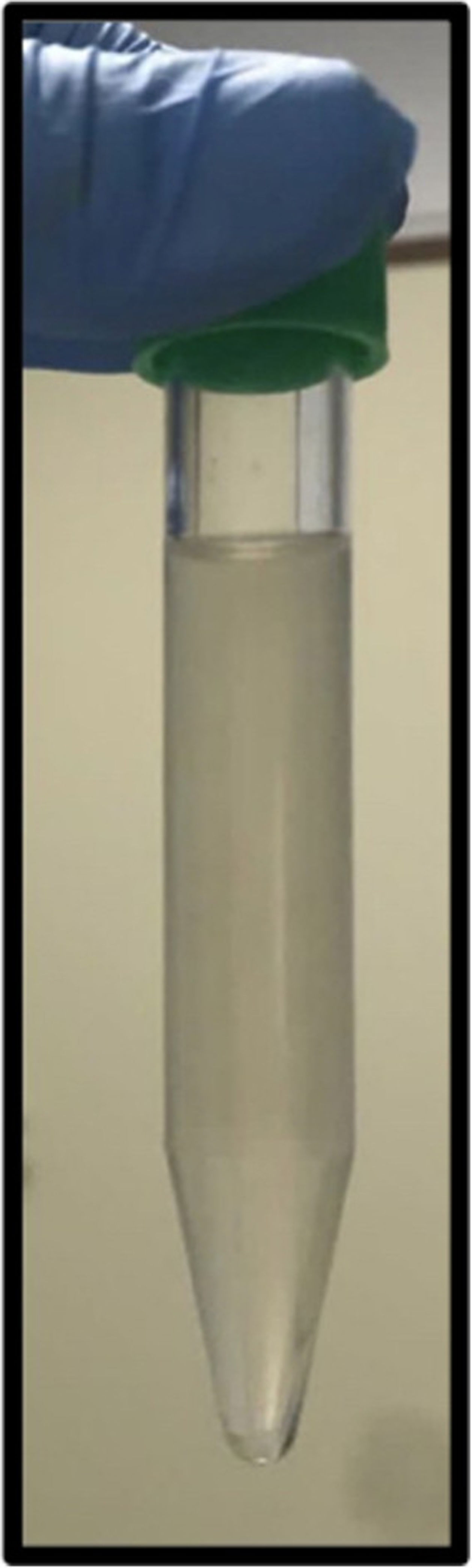
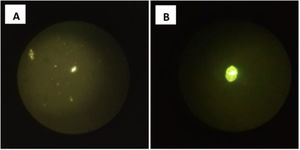
In turn, an ultrasound-guided puncture of the most accessible left posterior paravertebral loculated collection was performed, which oozed a non-purulent clear serous fluid (Fig. 2).
Clinical courseAfter observing the macroscopic characteristics of the aspirated fluid in situ, an extrahepatic hydatid disease was suspected, despite the location and atypical presentation, for which urgent antiparasitic treatment was started combined with albendazole 400mg/12h indefinitely and praziquantel 50mg/kg/day/for two weeks, closely monitoring the patient, who did not present any type of anaphylactic reaction or immediate complication.
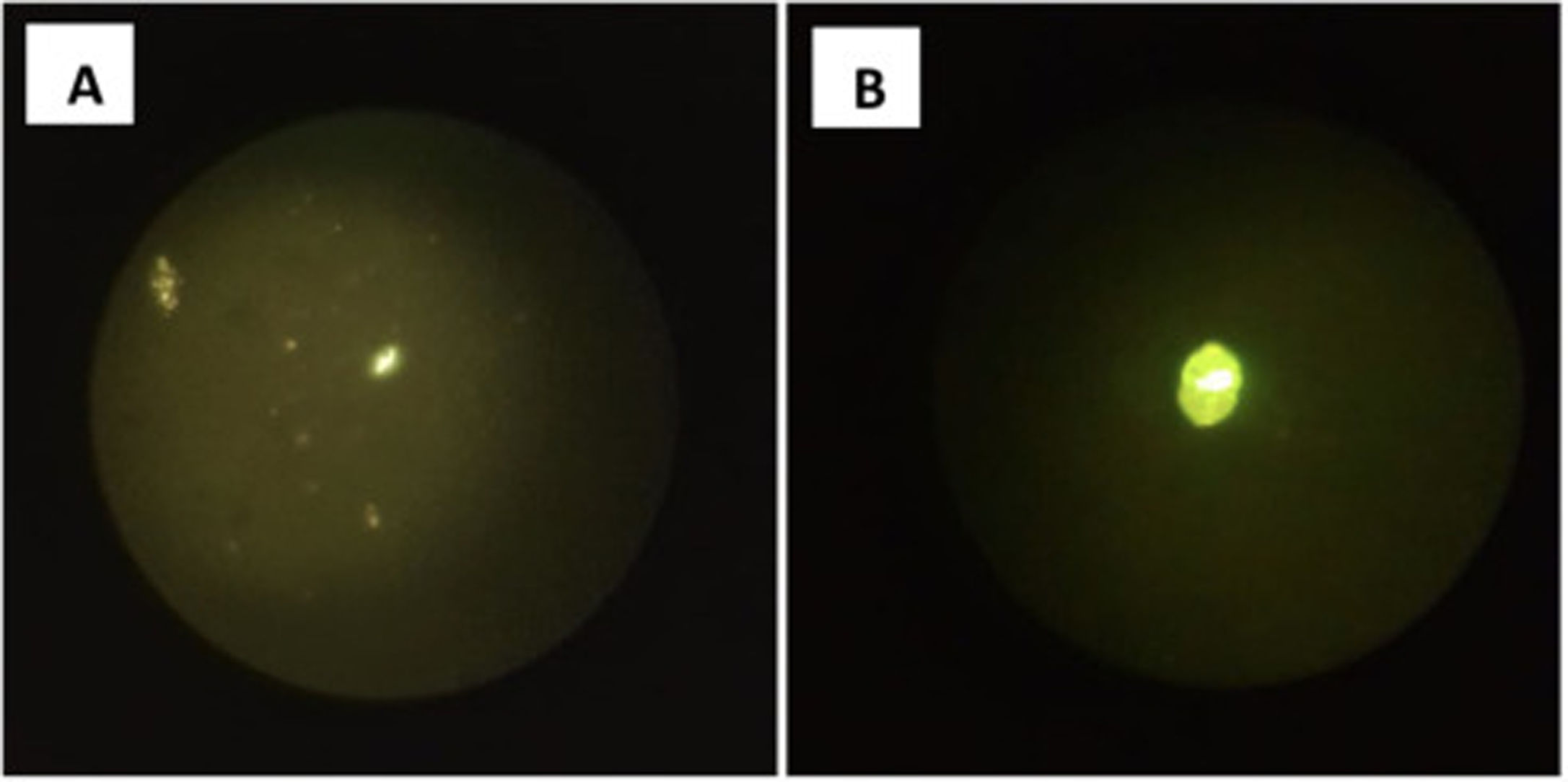
Closing remarksThe microbiological study was morphologically compatible with the larval stage of Echinococcus granulosus (Fig. 3), which was later confirmed by the molecular detection of specific DNA by positive polymerase chain reaction (PCR).
As a complementary study, a gallium-67 scintigraphy was performed with no data of superimposed septic involvement at the bone/vertebral level and also a cranial CAT scan with no evidence of brain lesions. The rest of the microbiological cultures (standard culture, Auramine staining, Löwenstein-Jensen culture of the aspirate and blood cultures) were negative.
Hydatidosis or cystic echinococcosis is a zoonosis caused by the genus Echinococcus, the species responsible being E. granulosus. There are other species that also cause disease in humans, including E. multilocularis, which causes alveolar echinococcosis, a much less common disease. Western China, Central Asia, South America, Eastern Africa and some Mediterranean countries are considered to be highly endemic areas.1
Traditionally included in the list of neglected tropical diseases, the difficulty in its diagnosis and clinical management lies in the lack of prior standardisation, motivating in 2020 the preparation of a consensus document where the available scientific evidence is evaluated, serving as a guide for professionals who are faced with a case of hydatidosis.2
Hydatid cysts can occur anywhere in the body, although the most frequently affected organ is the liver (75% of cases).3 Bone involvement is very rare but possible, representing a real clinical challenge for its diagnosis.4 The incidence of bone involvement is estimated at between 0.5% and 4% of all cases of hydatid disease, of which up to 60% have been diagnosed in European countries such as Spain, with a documented series at the Hospital Ramón y Cajal [Ramón y Cajal Hospital], in Madrid, with bone involvement in 26% of the cases analysed over almost three decades.5
In our case, the disc and bone involvement, together with the epidemiological context (endemic area), supported the more likely diagnosis of tuberculosis, which is why an ultrasound-guided sample was taken from the loculated lesion that showed a dense content on ultrasound. After objectifying the macroscopic characteristics of the liquid, not purulent at all, but rather a whitish aqueous liquid, and with the patient's history of treated hydatid disease, the aforementioned antiparasitic treatment was urgently started which had a favourable clinical outcome. At the present time, the patient has been evaluated for thoracic surgery for definitive surgical treatment of the cysts, while maintaining albendazole indefinitely, after having completed the first two weeks with combined therapy with praziquantel, remaining clinically and radiologically stable.
In general, the treatment of hydatid disease includes anthelmintic therapy combined, when possible, with surgical resection of the cyst or percutaneous aspiration and instillation of scolicidal agents depending on the site and size. This disease is very difficult to treat correctly, especially when it occurs with bone involvement, about which little scientific evidence is currently available.5–7
It is vitally important, when hydatid cyst is suspected both in surgery and in puncture aspiration, to administer antiparasitic treatment with albendazole±praziquantel from 2 to 4 weeks prior until 1–3 months after surgery to minimise the risk of parasite propagation in case of accidental rupture or dissemination of the cyst.1,8
FundingWe did not receive any funding for the drafting of the manuscript.
To Dr F. García and Dr R. Varela (Radiology Unit) for their helpful collaboration.
Please cite this article as: Ferra Murcia S, Cabezas Fernández MT, Fernández Fuertes E, Collado Romacho AR, Dorsolumbalgia y colecciones paravertebrales con afectación ósea de etiología inesperada, Enferm Infecc Microbiol Clin. 2022;40:396–398.