A 35-year-old man was brought to the emergency department after having been found on the street with a decreased level of consciousness. He was a black patient with no available medical history, apart from a history of alcoholism and drug dependence.
On arrival, the patient had hypotension (80/40 mmHg), tachypnoea (30 bpm), tachycardia (138 bpm) and a fever of 38 °C. The patient reported pain in the right side of the chest along with haemoptysis and abdominal pain. Physical examination revealed that the patient had a Glasgow scale score of 12 points, blood remnants in the oropharynx and crepitations in both lung fields. It was unknown how long he had been in this condition. A few minutes after he arrived in the emergency department, he presented a sudden deterioration of his level of consciousness, down to a Glasgow scale score of 3, such that he required emergency orotracheal intubation and admission to the intensive care unit. The patient's brief prior medical history indicated that he was from Guinea, had not recently travelled to that country and was currently living in an immigration centre.
Laboratory testing showed the following clinical chemistry abnormalities: glucose 19 mg/dl (74–106), creatinine 4.2 mg/dl (0.7–1.2), sodium 129 mmol/l (135–145), GOT 138 U/l (5–40), LDH 390 U/l (135–225) and elevated acute phase reactants (C-reactive protein 34 mg/dl and procalcitonin >100 ng/mL). It also showed severe neutropenia of up to 200 cells/μl, as well as moderate lymphopenia and thrombocytopenia. Venous blood gas revealed severe mixed acidosis: pH 6.7; pCO2 91 mmHg; pO2 31 mmHg; bicarbonate 6.7 mmol/l and lactate 25 mmol/l.
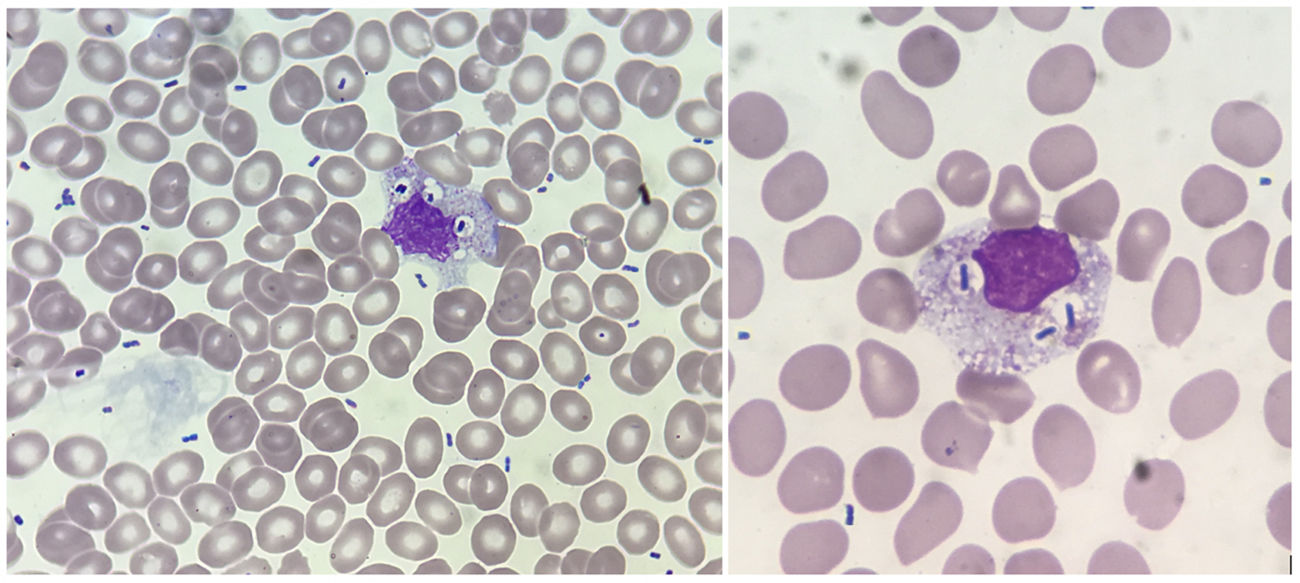
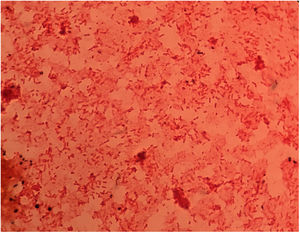
A peripheral blood smear was ordered in which multiple free bacilli were observed throughout the smear, some phagocytosed by monocytes and neutrophils (Fig. 1). The absence in the smear of elements in a “seal-ring” shape, along with the negative result for the thick smear and Plasmodium spp. antigen, ruled out malaria.1
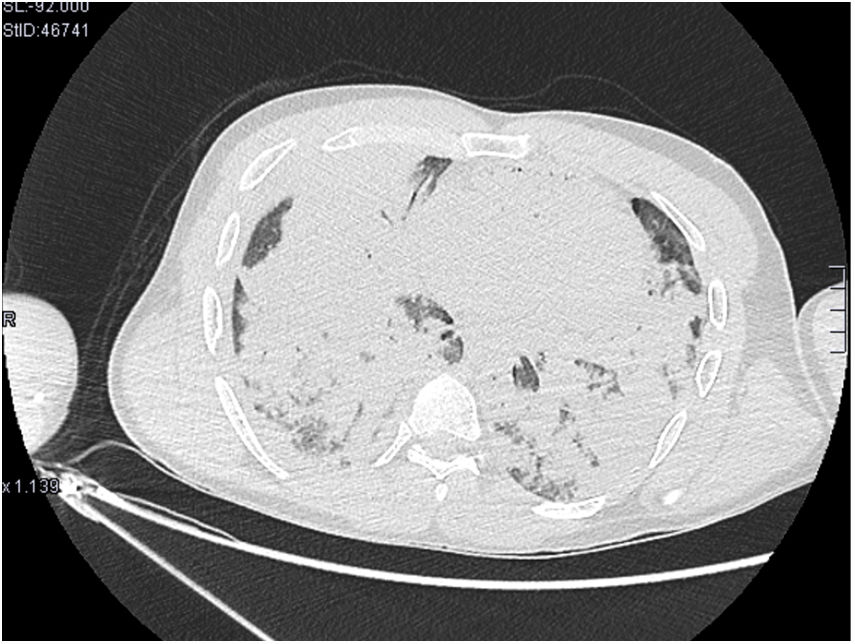
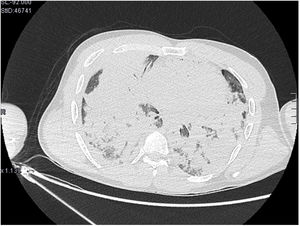
A CT scan of the chest showed multiple bilateral pulmonary consolidations. These were predominantly in the lower lobes, and some had a rounded morphology. It also showed complete collapse of the right upper lobe (Fig. 2).
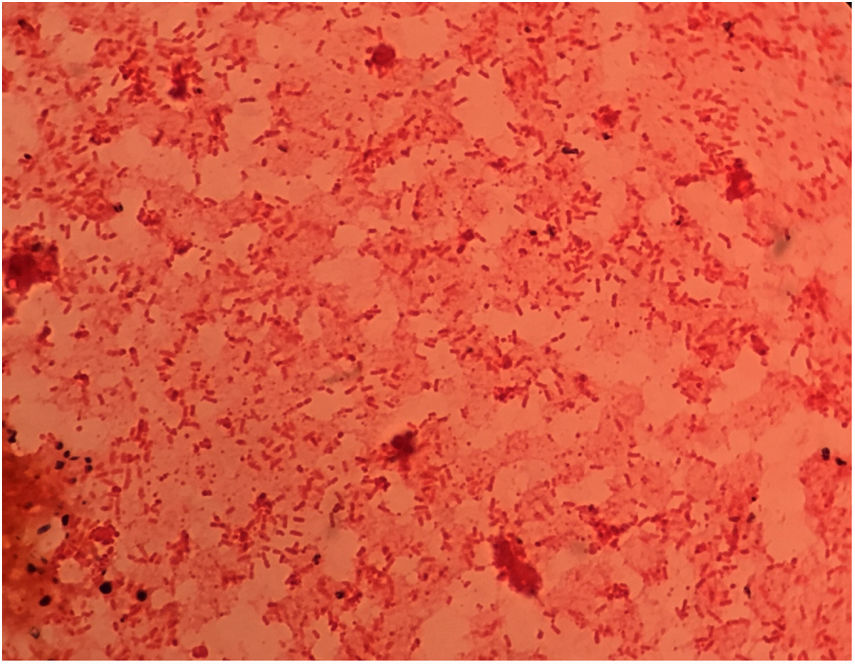
Clinical courseThe patient was started on empirical antibiotic therapy with piperacillin/tazobactam. In less than two hours, the microbiology department reported growth in blood cultures of numerous Gram-negative bacilli (Fig. 3); therefore, antibiotic coverage was broadened with amikacin. A Gram stain of the peripheral blood smear was also performed to confirm that these elements seen on the smear corresponded to Gram-negative bacilli.
The patient went into cardiorespiratory arrest. Advanced cardiopulmonary resuscitation manoeuvres were performed without success, and the patient died four hours after being admitted to the hospital.
The next day, the Gram-negative bacilli were identified as pan-susceptible Klebsiella pneumoniae in the blood culture and sputum. Chronic hepatitis B virus infection was also determined (positive result for hepatitis B surface antigen, with positive anti-HBe and anti-HB IgG core antibodies as well as negative IgM antibodies) and positive Treponema pallidum serology with a negative rapid plasma reagin (RPR) test.
All the other microbiological tests performed (culture for mycobacteria and serologies for HIV, HCV, CMV, Leptospira interrogans, Borrelia spp., dengue, Entamoeba spp. and Leishmania spp.) were negative.
Final remarksKlebsiella pneumoniae is an aerobic Gram-negative bacillus belonging to the Enterobacteriaceae family. In general, it colonises the mucosal surfaces of the oropharynx and gastrointestinal tract of human beings, and may show different degrees of virulence and resistance to antibiotics and invade different tissues. Typically, it affects patients with chronic obstructive pulmonary disease, diabetes, alcoholism or immunosuppresion in general. Despite early administration of antibiotic therapy, pneumonia due to K. pneumoniae presents a high mortality rate (30%–50%),2,3 especially if it is associated with bacteraemia, and has a worse prognosis in alcoholic patients, having a mortality rate in these cases of up to 64%.4 Respiratory failure is usually the cause of death in patients with pneumonia due to K. pneumoniae, particularly when there is rapid dissemination to multiple pulmonary lobes or progression towards acute respiratory distress syndrome.
The finding of bacilli on a peripheral blood smear is very unusual. There are few reported cases in the literature1,5–7; most reported cases correspond to patients who have died. Therefore, visualisation of bacilli on a smear, along with clinical data, should prompt the clinician to suspect an extremely serious infection.
Please cite this article as: Navarro-Almenzar B, López Castaño F, Hurtado Oliver B. Paciente de Guinea con shock séptico fulminante. Enferm Infecc Microbiol Clin. 2020;38:341–342.