We report the case of a 46-year-old-man, originally from Ghana, who had been living in Spain for 18 months and with no serious illnesses and no history of smoking, drinking or drug abuse. He went to the Emergency Department because of weakness, malaise, fever and a cough without expectoration for a week. He also explained sexual risk behavior 7 years previously with his partner, who was infected with HIV, with both HIV tests (Western Blot (WB) and ELISA) being negative then.
At hospital admission, physical examination revealed cachexia, hepatosplenomegaly and inguinal lymphadenopathy with no other important findings. The chest X-ray was also normal and the blood test showed pancytopenia (Hemoglobin 11g/dL, 55,000platelets/mm3, 800leukocytes/mm3 with 521neutrophils/mm3, 186lymphocytes/mm3 and 70monocytes/mm3), acute renal failure (Glomerular filtrate rate 19mL/min/1.73m2, Creatinine 3.68mg/dL), liver biochemical alterations, LDH 2290IU/L and C-reactive protein (CRP) 51.2mg/dL.
The anemia test revealed very high ferritin levels (>14,683μg/L). Additionally, the patient presented continuous LDH elevation (maximum of 17,800IU/L), very low levels of albumin (0.9g/dL), progressive elevation of lactate and persistent unspecific inflammatory changes such as CRP, procalcitonin and fibrinogen. All blood, sputum, urine and mycobacterium cultures were negative. EBV-IgG and HBV serology were positive, with 94,100,000copies. HIV infection was confirmed by Western Blood (WB) and ELISA and the total amount of CD4 lymphocytes was 10CD4/mm3 (1.4%) and HLA-B*5701 was negative. Entecavir, Ritonavir, Raltegravir, Darunavir and Lamivudine were started as well as prophylaxis with Trimethoprim-Sulfamethoxazole and Ganciclovir.
Abdominal ultrasound showed clinical nephropathy and splenomegaly and a body scan (TC) revealed anasarca with bilateral pleural effusion and pulmonary edema.
The patient was deteriorating becoming anuric, confused and agitated. A new blood test showed high levels of triglycerides (up to 717mg/dL) with progressive deterioration of the liver and renal functions and aggravated pancytopenia, requiring platelets and blood transfusion. These findings, including the persistent fever, suggested a hemophagocytic lymphohistiocytosis (HLH).
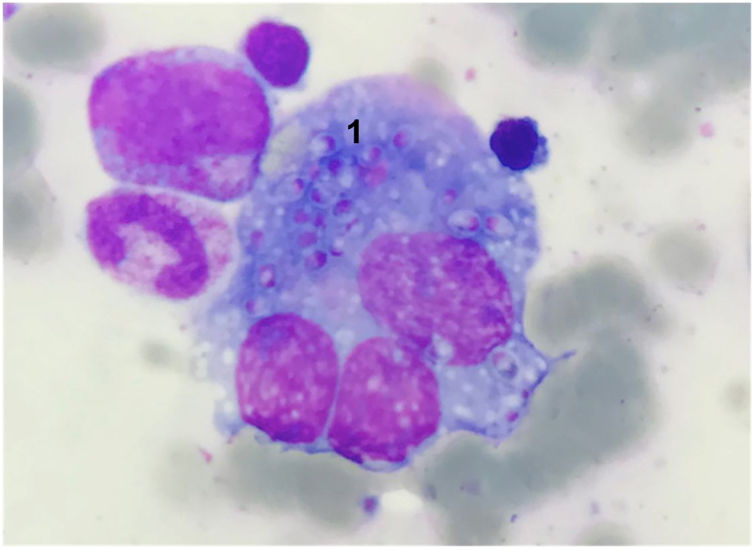
Due to the lack of a causing agent, a bone marrow aspirate was obtained, revealing a large number of oval cells between red blood cells and inside macrophages and granulocytes, suggesting fungal infection (Fig. 1).
A direct polymerase chain reaction (PCR) was performed to amplify the internal transcribed spacer 1 (ITS1) and ITS2. A Histoplasma capsulatum var duboisii was identified when the sequences obtained were analyzed using the BLAST alignment program of the GenBank database (National Institutes of Health) and liposomal amphotericine B by 4mg/kg/day doses were started.
However, the patient deteriorated further, requiring intensive care including hemodialysis, vasoactive drugs (norepinephrine), albumin and K-vitamin. The progression of the disease was very fast causing hepatic liver failure progressing to multiple organ failure (MOF) and, unfortunately, death.
A total of 30 cases of HLH associated with disseminated-histoplasmosis with HIV infection were identified through the Pubmed search, being reported 23 cases reported in Spanish by Gil-Brusola et al.1 Because of this, disseminated histoplasmosis is an uncommon presentation of HIV/AIDS in Spain, where there were 24 cases in HIV+ patients published in bibliography from 1988 to 2004,1 and 19 cases reported in the first decade of this century.2 Despite this, histoplasmosis is the most frequent, imported micosis in Spanish HIV patients, with most cases coming from America, and with only one case from Africa reported, where the most frequent variant is Histoplasma duboisii, as with the current case.1–4
HLH was described in 1939 and is divided into genetic or acquired forms, both characterized by an extreme inflammatory response due to natural killer (NK) cell dysfunction which activates the macrophage system.3,5–7 It is caused by underlying processes such as infections, autoimmune diseases or malignancy. The estimated incidence is 1.2-cases/million inhabitants/year, maybe underestimated.3 The diagnostic of HLH is defined by fulfilling one of the following: a molecular diagnosis consistent with HLH or 5 out of the 8 criteria below: fever, splenomegaly, cytopenia (affecting≥2 lineages in the peripheral blood), hypertriglyceridemia and/or hypofibrinogenemia, hemophagocytosis in bone marrow or spleen or lymph nodes, no evidence of malignancy, low or absent NK cell activity, ferritin≥500μg/L and soluble CD25≥2400U/mL, being the last three considered as new criteria.3,8
The initial management to secondary HLH includes the administration of etoposide and dexamethasone, both of which could be restarted and increased gradually in case of reactivation.3
Additionally, disseminated histoplasmosis is an uncommon opportunistic infection in HIV patients caused by Histoplasma capsulatum fungi, with the Capsulatum variant being more likely in America and the Duboisii variant more likely in Africa.1,4,8 Some cases of HLH due to disseminated histoplasmosis have been described, mostly of them caused by H. capsulatum var. capsulatum, but they are infrequent.
We thank our colleagues from Center de Diagnóstic Biomèdic (CDB), Hospital Clínic (Barcelona), who provided the specific diagnosis and especially to Francesc Marco for useful conversations.