In the context of community transmission of the virus, the impact of the pandemic on health-care systems, mainly on intensive care units (ICU), was expected to be devastating. Vall d’Hebron University Hospital (HUVH) implemented an unprecedented critical patient-care planning and management of resources.
MethodsWe describe a cohort of critically ill patients during the first two months of the pandemic (from March 3, 2020, to May 2, 2020) in HUVH, Barcelona.
In this manuscript, we report our previsions, strategies implemented, and the outcomes obtained.
ResultsThree-thousand and thirty-three patients were admitted to the HUVH Critical Care Units. Throughout the study period, the proportion of patients on IMV or IMV and ECMO remained above 78%. Most patients were men (65%); the most common age group was 60–70 years. Twenty-three patients received ECMO, and eighteen were cannulated at another center and transferred to HUVH. At the end of the study, fourteen patients were successfully decannulated, three patients died, and the rest of the patients were still on ECMO. Eight pregnant women have been treated in the ICU, with a survival rate of 100%. The ICU mortality of patients younger than 60 years was 3.2%. The mean ICU stay of both survivors and nonsurvivors was 14 days.
ConclusionThe adequate preparation for resource expansion for critically ill patients care, main challenges, and overall positive results can serve as a precedent for similar future scenarios.
En un escenario de circulación comunitaria del virus el impacto de la pandemia sobre el sistema sanitario y en las unidades de cuidados intensivos (UCI) se preveía devastador. El Hospital Universitario Vall d’Hebron (HUVH) ha desplegado un dispositivo de atención a pacientes críticos sin precedentes.
MétodosSe describen las previsiones realizadas, las medidas tomadas y los principales resultados en una cohorte de pacientes críticos durante los primeros dos meses (3 de marzo al 2 de mayo del 2020) de la pandemia por COVID-19 en el HUVH de Barcelona.
ResultadosEn el periodo de estudio, ingresaron en las Unidades de Críticos del HUVH 333 pacientes. El porcentaje de los pacientes en VMI o VMI y ECMO se mantuvo constantemente por encima del 78%. La mayoría de pacientes han sido hombres (65%); el grupo de edad más frecuente entre 60 y 70 años. Veintitrés pacientes recibieron ECMO, 18 de los cuales fueron canulados en otro centro y trasladados al HUVH. A fecha de cierre del estudio, 14 pacientes se decanularon satisfactoriamente, 3 pacientes fallecieron y el resto siguen en soporte con ECMO. Han sido atendidas en UCI 8 gestantes, con una supervivencia del 100%. La mortalidad en UCI de los pacientes menores de 60 años fue el 3,2%. La estancia media en UCI de las altas y los fallecimientos ha sido de 14 días.
ConclusionesLas estrategias de organización de la expansión de recursos para la atención de pacientes críticos, sus principales retos y los resultados obtenidos, pueden servir de clave para futuros escenarios similares.
On 11th March 2020, Tedros Adhanom Ghebreyesus, WHO Director-General, declared the coronavirus outbreak (COVID-19) a pandemic. The first recorded COVID-19 case in Spain was diagnosed on 31st January 2020. It was a mild and imported case involving a German patient who was admitted to hospital in La Gomera, Canary Islands. The first cases on the Iberian peninsula were reported on 24th February. After this, the virus spread exponentially across the different provinces and lockdown was imposed on the population on 13th March.
Inspired by the slogan “Hope for the best, prepare for the worst”1, and based on the Contingency Plan of the Spanish Society of Intensive Care and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias, SEMICYUC)2, Hospital Universitario Vall d’Hebron (HUVH) has developed an unprecedented healthcare device for critically ill patients. The mortality of the outbreak would depend more on the healthcare system’s ability to respond than on the treatments administered3. This manuscript describes the organisation, challenges and outcome of the expansion of critical area capacity and resources in response to the pandemic, which may be a key factor in similar future scenarios.
MethodologyThis manuscript describes the predictions made, the measures taken and the main outcomes in a cohort of critically ill patients during the first two months (3rd March to 2nd May 2020) of the COVID-19 pandemic at HUVH in Barcelona.
Pandemic predictions for the HUVH healthcare areaHUVH started to prepare the transformation strategy on 31st January, three weeks before the first non-imported case was diagnosed in Spain. The epidemic in China was monitored using WHO data4 from 22nd January 2020 and various predictive scenarios were analysed to adjust available hospital resources to the number of COVID-19 cases diagnosed at our hospital.
HUVH is the community hospital of the Barcelona Nord area, which comprises five districts with a population of more than 439,654 people5,6. It is a tertiary referral hospital for the whole Autonomous Community of Catalonia for multiple specialties and pathologies, including with extracorporeal membrane oxygenation (ECMO) support therapy and obstetrics.
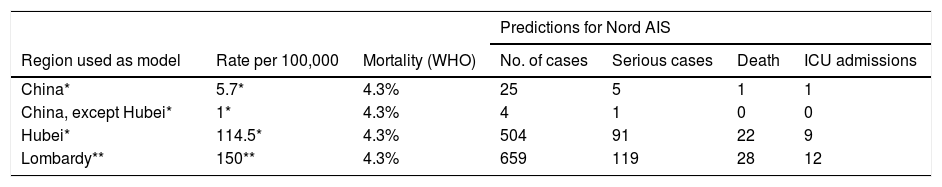
Predictions madeThe cumulative cases (cumulative incidence) in the Barcelona Nord area were predicted. Three incidence rates were taken into consideration: the mean rate in China (5.7 cases/100,000 inhabitants or 0.0057%); the average rate of the provinces with the lowest incidence rate (all, except Hubei), with 1 case/100,000 inhabitants (0.001%); and the Hubei rate on 11th March 2020, with 114.5 cases/100,000 inhabitants (0.1145%)4. Based on a report by WHO and the Italian Ministry of Health on the incidence rate in Lombardy7, a fourth rate of 150 cases/100,000 inhabitants was considered.
The same proportion of serious cases was taken into account, according to WHO data (18%), and 10% of these were considered to require ICU admission. Table 1 shows the predicted serious cases and cases requiring ICU admission for the population of the Nord Integral Healthcare Area (Área Integral de Salud, AIS) with these four incidence rates.
Predictions made for the HUVH referral region (Nord Integral Healthcare Area [AIS] = 439,654 inhabitants) based on data from China and Lombardy (source of data, WHO).
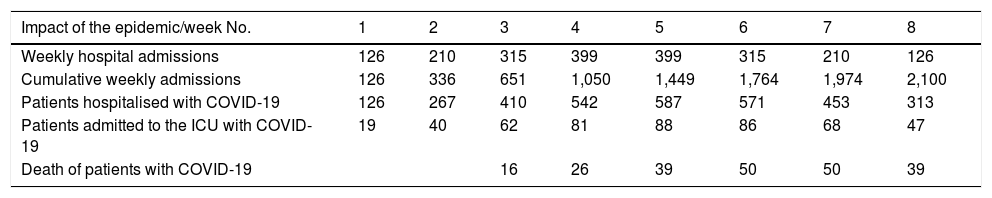
The Epidemiology Department of our hospital estimated the impact of an epidemic wave of SARS-CoV-2 infections on the HUVH referral region, with an attack rate (cumulative incidence) of 2.5% (Table 2). This prediction also estimates the epidemic outbreak in eight weeks time and distributes cases according to a possible epidemic curve, which allows a better estimate of necessary resources (Table 2).
Attack rate of 2.5% (2,500 cases/100,000) over eight weeks. Estimated weekly admissions during the epidemic period.
| Impact of the epidemic/week No. | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Weekly hospital admissions | 126 | 210 | 315 | 399 | 399 | 315 | 210 | 126 |
| Cumulative weekly admissions | 126 | 336 | 651 | 1,050 | 1,449 | 1,764 | 1,974 | 2,100 |
| Patients hospitalised with COVID-19 | 126 | 267 | 410 | 542 | 587 | 571 | 453 | 313 |
| Patients admitted to the ICU with COVID-19 | 19 | 40 | 62 | 81 | 88 | 86 | 68 | 47 |
| Death of patients with COVID-19 | 16 | 26 | 39 | 50 | 50 | 39 |
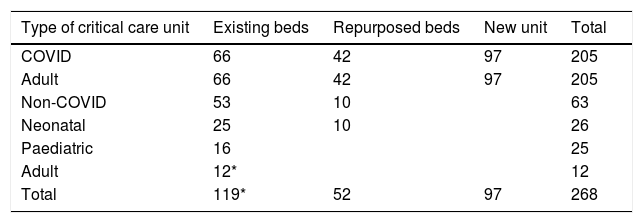
To optimise resources, a plan was drafted in advance to progressively increase the hospital’s critical care bed capacity using the following criteria:
- 1
Prioritisation according to ease of implementation, resource needs and impact on the organisation (e.g., involvement of the surgical programme, transplant programme, etc.);
- 2
Incorporation of existing repurposed devices;
- 3
Incorporation of new devices that need to be adapted. Bright isolated spaces fitted with temporary medicinal gas supplies and the corresponding electrical fittings were created.
It was possible to expand the critical care facilities to 268 ICU beds (initial provision 123 beds; repurposed units 52 beds; and new units 97 beds). Four paediatric beds were used for adults (Table 3). These beds were allotted as follows: 205 beds for COVID-19 patients, 26 beds for other diseases and 37 for Paediatrics and Neonatal Care. The beds were sent to 13 units distributed throughout three buildings.
A Respiratory Intermediate Care Unit, run by the Pneumology Department, was created to allow early discharge from the Critical Care Units.
This expansion forced us to reduce scheduled surgical activities and organ donation and transplantation programme activities.
Adaptation of human resourcesThe Intensive Care Medicine Department’s regular staff is not adequate to take on all the activity generated as a result of the resource expansion plan. Up to 40% of the professionals are unlikely be unable to work at different times as a result of contracting the disease (at work or in the community) and work routines would need to be organised to take into consideration breaks. Three-day shifts have been organised with 24 h on duty and 48 h off.
It has been necessary to reincorporate all intensive care medicine doctors working outside the ICU (teaching, transplant coordination) and also recently retired professionals. Multidisciplinary teams of professionals from critical areas (Anaesthesia and Resuscitation, cardiologists and paediatricians from the paediatric ICU and neonatal ICU) have been created, supervised and coordinated by the ICU. In total, 250 professionals are coordinated online. The teams are complemented by medical professionals with little or no ICU training who are assigned tasks such as clinical documentation, safety protocols, information for family members and consent requests. High-risk professionals (elderly and approaching retirement, retired, pregnant, clinically significant chronic respiratory diseases and immunocompromised professionals) have been given the role of managing patients with other diseases.
To guarantee the psychological and mental health of professionals, specific support programmes have been set up by the HUVH Psychiatry and Psychology Departments.
Coordination, communication and training coordinationCoordinationAn operating committee (heads of the Intensive Care Medicine and Anaesthesiology departments, HUVH Critical Care coordinator and the coordinators of the various units) was created. Every morning these individuals report the number of admissions/discharges per unit from the previous day and the expected number of discharges. A healthcare coordinator is also responsible for sending professionals each day to the areas experiencing the highest work overload on a day-by-day basis.
CommunicationInternal communication is possible on two levels using online tools. The operating committee meets every day between 2.00 p.m. and 3.00 p.m. using Zoom (Zoom Video Communications Inc., San José, California). These meetings allow the committee to discuss healthcare coordination, changes in protocols, difficult clinical decisions, patient rounds and troubleshooting. Communication with other professionals who are members of the ICU-COVID team is possible by instant messaging (WhatsApp Inc., Mountain View, California), thereby ensuring homogeneous healthcare and the daily updating of the progress of inpatients. An on-call intensive care medicine doctor is also available 24 h a day for consultation purposes.
TrainingTraining was provided on personal protective equipment (PPE), including simulations to ensure correct use, donning and removal of PPE, proning and the different ventilators. A webinar has been given on a weekly basis on updates for treating critically ill patients with COVID-19 pneumonia.
EquipmentThe equipment required most frequently has been mechanical ventilators. With the expansion of the different critical care areas, different types of ventilators have been used: ICU ventilators, anaesthetic machines (AM), repurposed non-invasive ventilation (NIV) ventilators and transport ventilators.
AMs have been modified to an open system. To do this, it was necessary to: (1) adjust the fresh gas flow to a minimum of 1.5 times the minute volume delivered to the patient; (2) bypass the soda lime on those AMs that permitted this (inspired and expired CO2 was monitored to rule out the presence of rebreathing); and (3) humidify the inspired air to prevent endotracheal tube occlusion.
Each new ICU bed had a bedside monitor with centralised alarms on a central monitor and four infusion pumps. Each new unit was equipped with a gas analyser. The number of extrarenal clearance monitors has been increased from 18 to 25. However, only 5.6% of critically ill patients have required extrarenal clearance techniques and therefore this increase in devices has not been required.
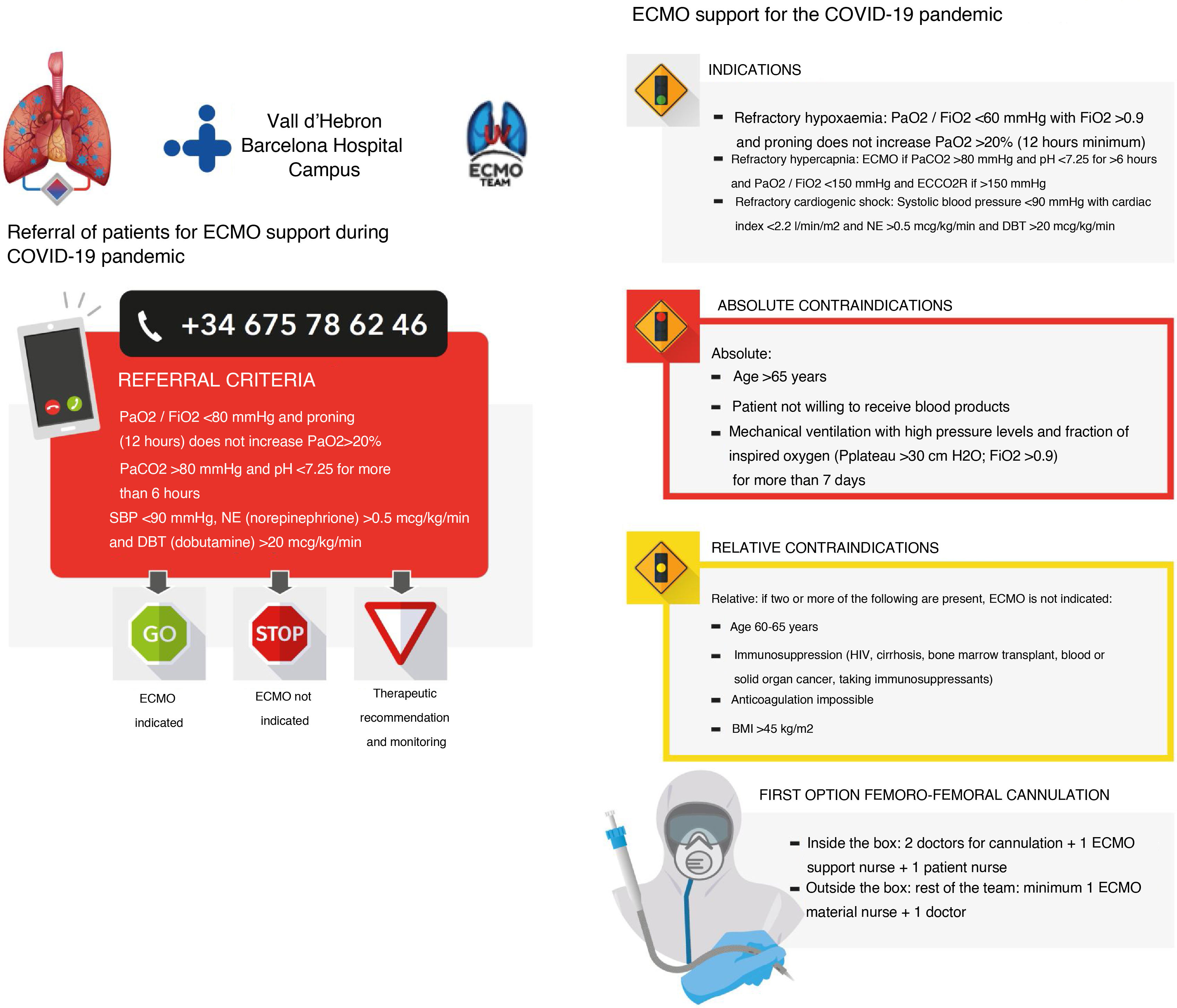
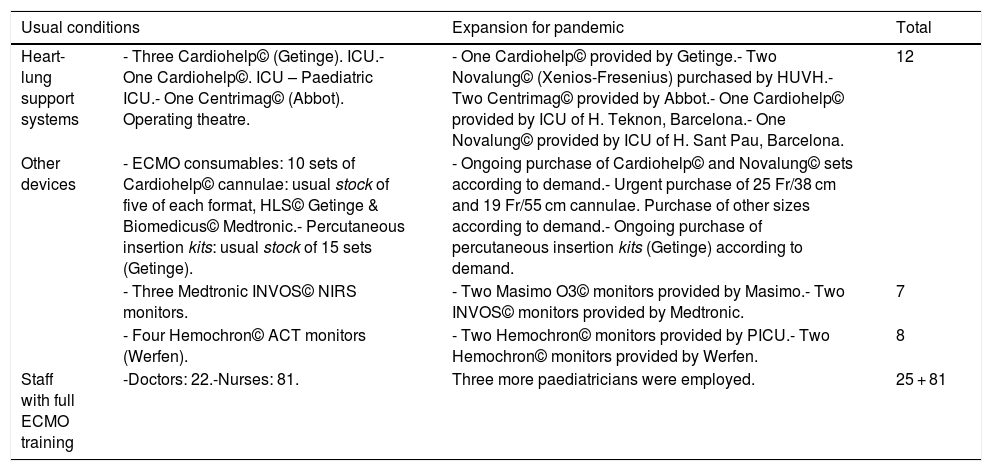
Extracorporeal membrane oxygenation (ECMO) equipmentThe Department of Health (Departament de Salut) identified HUVH as an ECMO Centre, a referral hospital for ECMO-based respiratory care for COVID-19 patients. Calculations were therefore done to determine the number of referrals we would receive. Using the FluSurge platform, it was determined that 5–8 patients admitted to the HUVH ICU would need ECMO therapy during the pandemic. It was also calculated that we would receive 55 referrals from other sites during the pandemic with eight referrals/week at the peak of the pandemic. After considering this data, the amount of material required was adjusted as shown in Table 4. Criteria for the indication and contraindication of ECMO in COVID-19 patients were adjusted after taking into consideration prior experience during the H1N1 pandemic, the little known about the pathophysiology of the disease and the potential lack of resources. Posters outlining these criteria and the HUVH team’s ECMO referral variables were sent to all the country’s ICUs (Fig. 1).
Summary of material and staff adjustments made for the HUVH ECMO programme.
| Usual conditions | Expansion for pandemic | Total | |
|---|---|---|---|
| Heart-lung support systems | - Three Cardiohelp© (Getinge). ICU.- One Cardiohelp©. ICU – Paediatric ICU.- One Centrimag© (Abbot). Operating theatre. | - One Cardiohelp© provided by Getinge.- Two Novalung© (Xenios-Fresenius) purchased by HUVH.- Two Centrimag© provided by Abbot.- One Cardiohelp© provided by ICU of H. Teknon, Barcelona.- One Novalung© provided by ICU of H. Sant Pau, Barcelona. | 12 |
| Other devices | - ECMO consumables: 10 sets of Cardiohelp© cannulae: usual stock of five of each format, HLS© Getinge & Biomedicus© Medtronic.- Percutaneous insertion kits: usual stock of 15 sets (Getinge). | - Ongoing purchase of Cardiohelp© and Novalung© sets according to demand.- Urgent purchase of 25 Fr/38 cm and 19 Fr/55 cm cannulae. Purchase of other sizes according to demand.- Ongoing purchase of percutaneous insertion kits (Getinge) according to demand. | |
| - Three Medtronic INVOS© NIRS monitors. | - Two Masimo O3© monitors provided by Masimo.- Two INVOS© monitors provided by Medtronic. | 7 | |
| - Four Hemochron© ACT monitors (Werfen). | - Two Hemochron© monitors provided by PICU.- Two Hemochron© monitors provided by Werfen. | 8 | |
| Staff with full ECMO training | -Doctors: 22.-Nurses: 81. | Three more paediatricians were employed. | 25 + 81 |
It is not possible to give specific therapeutic recommendations for coronavirus (SARS-CoV-2). Recommendations have been based on knowledge gained during other viral pandemics (e.g., flu, severe acute respiratory syndrome due to other coronaviruses [SARS], Middle East respiratory syndrome [MERS]), on improved evidence on the respiratory management of patients with acute respiratory distress syndrome (ARDS) and on recent relevant publications on COVID-19. It is vitally important that recommendations are coordinated and designed in accordance with each hospital’s capabilities and the patient's individual characteristics. The resulting document has been periodically updated according to new relevant evidence, incorporating all local experiences. It includes criteria for admission, invasive mechanical ventilation (IMV), antiviral and immunomodulatory therapy (drugs and extracorporeal options), anticoagulation, kidney and heart disease control, airway management (intubation, tracheotomy) and ECMO in refractory cases.
ConsumablesA contingency plan was drafted with recommendations for the rational use of PPE based on the prioritisation of care and difficulties restocking material due to supply shortages8. A mask can be reused provided that it is intact (unsoiled and undamaged) and not wet. The nursing supervisor of each unit is responsible for high-filtration masks: FPP3 mask (for intubation, tracheotomy, fibrobronchoscopy) and/or FPP2 mask. These are reused for the entire shift, protected by a surgical mask. They are then resterilised at the end of each shift with hydrogen peroxide. Safety goggles are reused after washing with enzymatic cleaner. Fluid-resistant gowns are reused and resterilised with hydrogen peroxide, provided that their structure is intact and there are no secretions or macroscopic fluids.
The use of disposable fibrobronchoscopes (Ambú© aScope 4 Broncho Regular) has been prioritised and reuse in the same patient throughout his/her ICU admission is preferable.
Treatment of special populations during the pandemic: children and pregnant womenThis is based on the following premises: 1. Need to maintain the ability to provide care for critically ill children but setting aside a few beds for adult patients; 2. Need to collaborate with the care system for critically ill adult patients infected with COVID-19 from the HUVH campus; 3. Need to provide top-quality care to pregnant women infected with COVID-19, as a referral hospital for these patients, by organising care for critically ill obstetric patients with COVID-19 or other obstetric disorders.
Method: 1. Four semi-critical care beds have been added in the area adjacent to the Paediatric Intensive Care Unit (PICU), which is usually used as a post-anaesthesia recovery area, and all non-urgent surgical procedures have been cancelled, with the exception of the paediatric solid organ transplantation programmes; 2. Pregnant women requiring admission to the ICU have been admitted to the PICU. The advantage of this option is its proximity to the Obstetrics team, Neonatology team and delivery room, which are all located on the same floor just a few metres from the Unit.
Plan for communication with family members and bioethicsAt this stage, we have had to work with patients who have been forcibly isolated from their family unit, families who are in crisis situations far away from their loved ones and individuals who are potentially in a situation where they will get sick (or are already sick). These situations have required that we communicate via electronic systems (mainly the phone and video calls). We have created infographics, made available on the hospital’s website, as an aid for families to help them understand even the most complicated medical information. End-of-life visits have been kept as short as possible and limited to one relative.
Decisions regarding admissions and ceiling of care have been made based on the recommendations of the SEMICYUC9 and specific recommendations of the hospital's Bioethics Committee at the request of the Intensive Care Medicine Department.
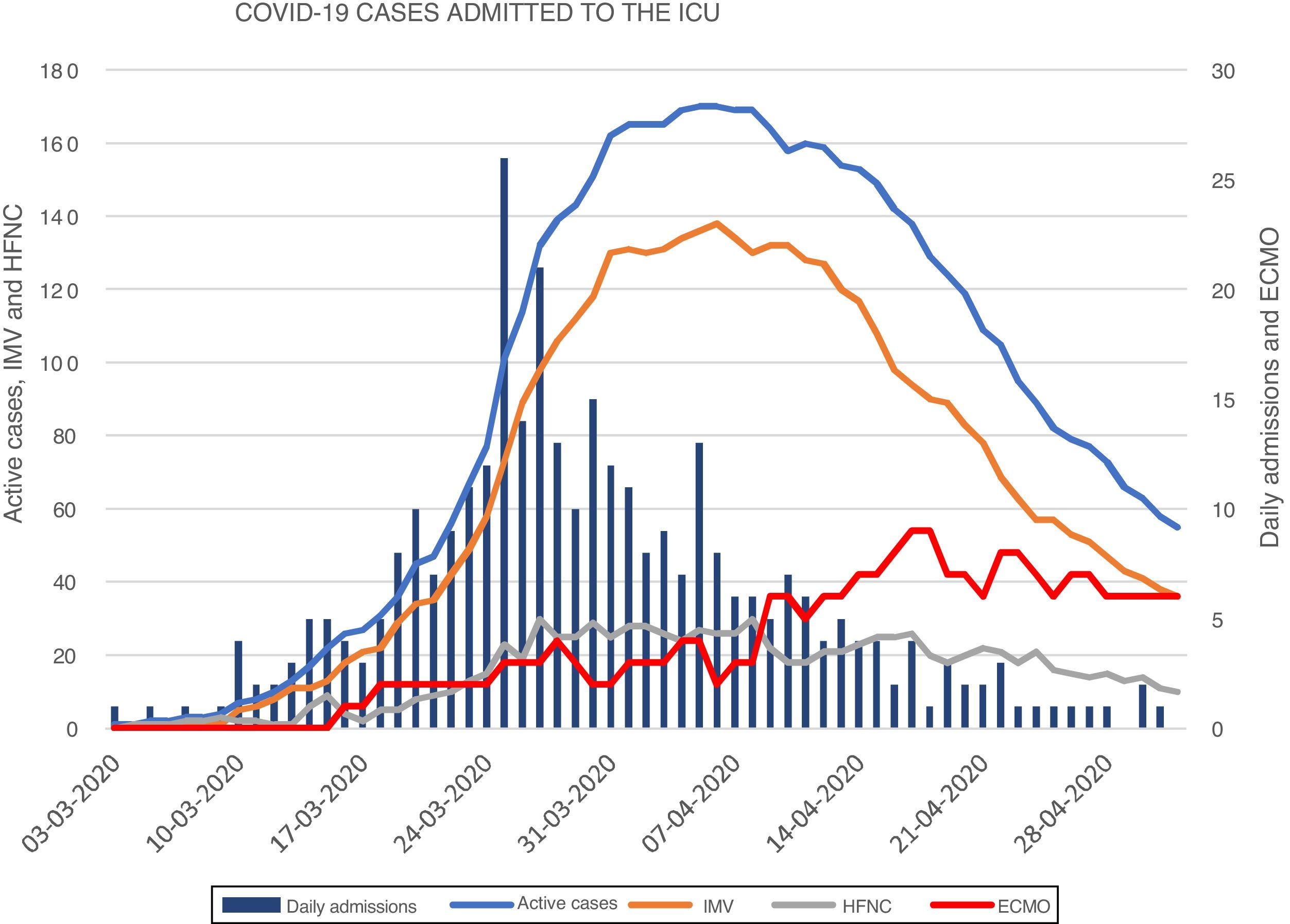
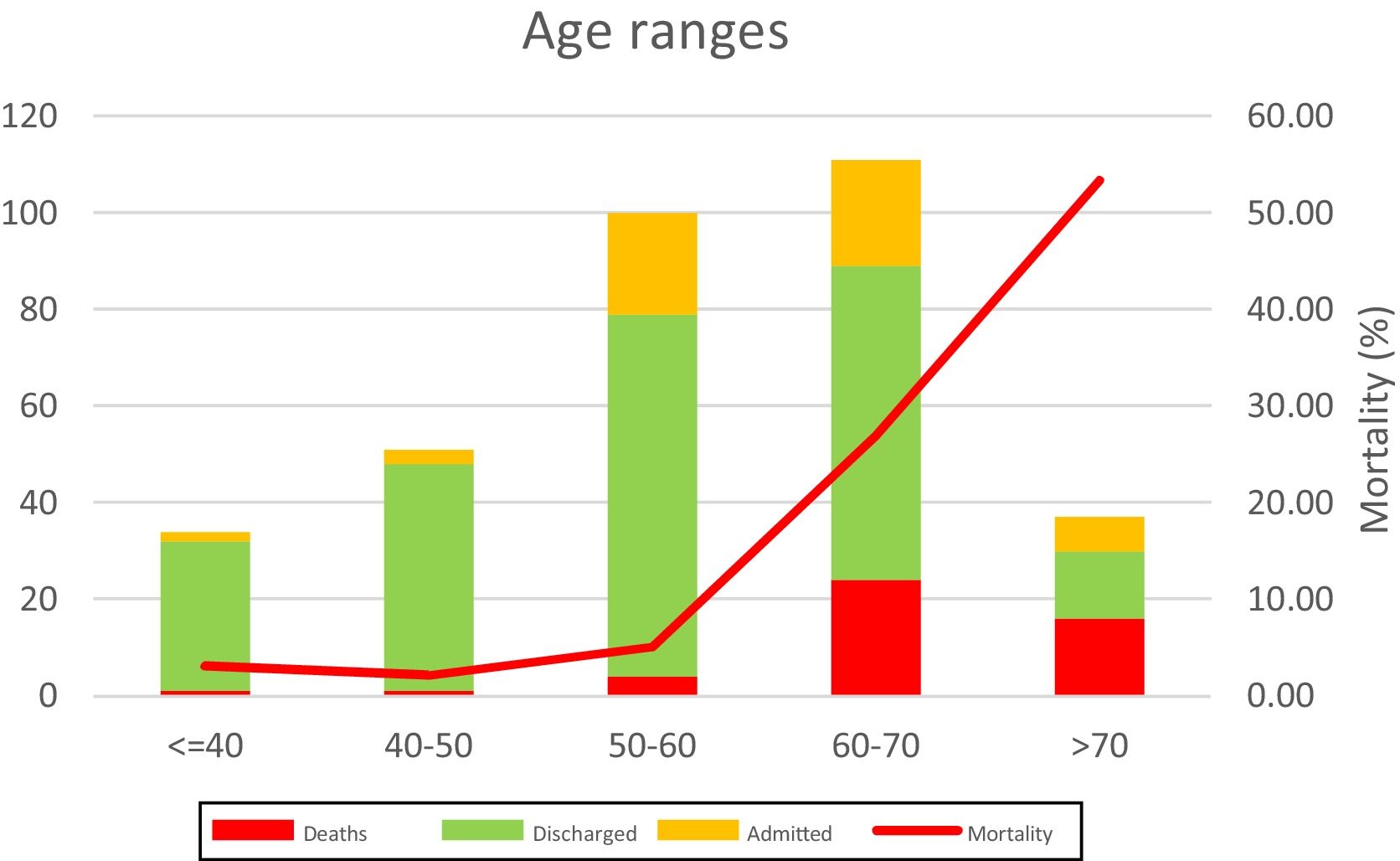
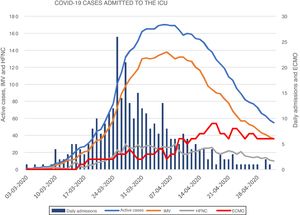
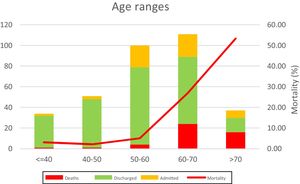
Change in ICU admissions and overall resultsBetween 3rd March and 2nd May 2020, 333 patients were admitted to the Critical Care Units at HUVH (Fig. 2). The number of new cases peaked on 25th March with 24 cases a day, while the number of admissions peaked on 6th April with 170 cases in the different ICUs. In addition, the number of cases requiring ECMO support peaked on 18th April with 9 concomitant cases. During these two months, the percentage of patients on IMV or IMV and ECMO remained at all times above 78%. Sixty days after the first patient with COVID-19 pneumonia was admitted to the ICU, 55 patients were still hospitalised. Most patients have been men (65%) and the most common age group has been 60–70 years.
During the study period, 23 patients received ECMO support and 18 of these patients were cannulated at another hospital and transferred to HUVH. On the study closeout date, 14 patients had had their cannulas removed satisfactorily, 3 patients had died and all other patients remained on ECMO support.
During the study period, eight pregnant women were admitted to the ICU, including one woman expecting twins with pneumonia. Three pregnant women required high-flow oxygen therapy and five required IMV. Four patients required caesarian sections resulting in five healthy babies. All other pregnant women are continuing with their pregnancy. The survival rate of this population has therefore been 100%.
ICU mortality rates for the different age groups (Fig. 3) show increasing mortality with age and the ICU mortality rate for patients younger than 60 years of age was 3.2%. The mean time in the ICU of all patients who were discharged or died has been 14 days.
DiscussionThe care of patients who were critically ill with COVID-19 pneumonia during the pandemic has been the greatest challenge faced by Intensive Care Medicine departments throughout history1.
By 2nd May 2020, a total of 217,466 cases had been confirmed in Spain. Of these, 118,495 patients required hospitalisation, 10,974 required admission to the ICU and 25,264 died due to complications associated with COVID-19 infection10. In Catalonia, 50,234 cases have been confirmed, making this the second most affected province, with 2844 cases requiring admission to the ICU. As described in this manuscript, HUVH has taken care of 333 critically ill patients (11.7 and 3.0% of the total number of critically ill patients in Catalonia and Spain, respectively). In this manuscript we have described the practical application of Contingency Plans at one of the Spanish hospitals that has seen most patients critically ill with COVID-19 pneumonia.
The clinical outcomes observed at HUVH have been better than those described previously in the literature11,12. These better outcomes cannot be explained by differences in the therapies administered, due to the lack of any one treatment with proven efficacy, but rather by the organisation’s ability to adapt to the pandemic.
Key organisational changes made at HUVH include: (1) Reduction in surgeries and activities of the organ donation and transplantation programme; (2) early increase in critical care beds; (3) training of multidisciplinary teams led by intensive care medicine specialists with suitable work and break times; (4) mobilisation of essential equipment, with any necessary modifications, especially ventilators and ECMO pumps, and consumables; (5) coordination and training of teams using electronic tools; (6) unified criteria for ICU admission, IMV and ECMO; (7) rational use of PPE and adaptation of sedation protocols to available drug supplies; and (8) care of critically ill pregnant women in the PICU.
The data observed has been much better than predicted, which proves that infections due to this outbreak are hard to predict by basing forecasts on other geographical areas. The heterogeneity of the disease in different countries requires close monitoring of the local epidemiology and early decision-making.
Likewise, in the event of future COVID-19 outbreaks, the increase in beds and the need for equipment and professionals should not interfere with the hospital's everyday activities and it is therefore appropriate to keep the increase in care facilities for the time being and adapt the intensive care medicine wards.
ConclusionsPractical application of the contingency plans for the care of critically ill patients with COVID-19 pneumonia is an organisational and healthcare challenge. Despite the very high demand experienced over a short period of time, the early planning of necessary resources at HUVH has allowed us to respond in an adequate manner with good overall results.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ferrer R, Báguena M, Balcells J, Bañeras J, Biarnes A, de Nadal M, et al. Organización de la atención a pacientes críticos en situación de pandemia: Experiencia del Hospital Vall d’Hebron durante el brote de neumonía por SARS-CoV-2. Enferm Infecc Microbiol Clin. 2022;40:71–77.