The case of a 53-year-old Caucasian male, with no medical-surgical history of interest, who came to our consultations for a pruritic lesion which appeared two months ago in the left forearm after contact with waste water at home is presented. He reported a previous wound in that area, had no general symptoms and denied contact with dirt, animals or plants. He had been treated with mometasone furoate cream for a month without improvement. On physical examination, an infiltrated purple erythematous plaque with irregular borders measuring 35mm×25mm was observed, with a central ulcer measuring 5mm (Fig. 1).
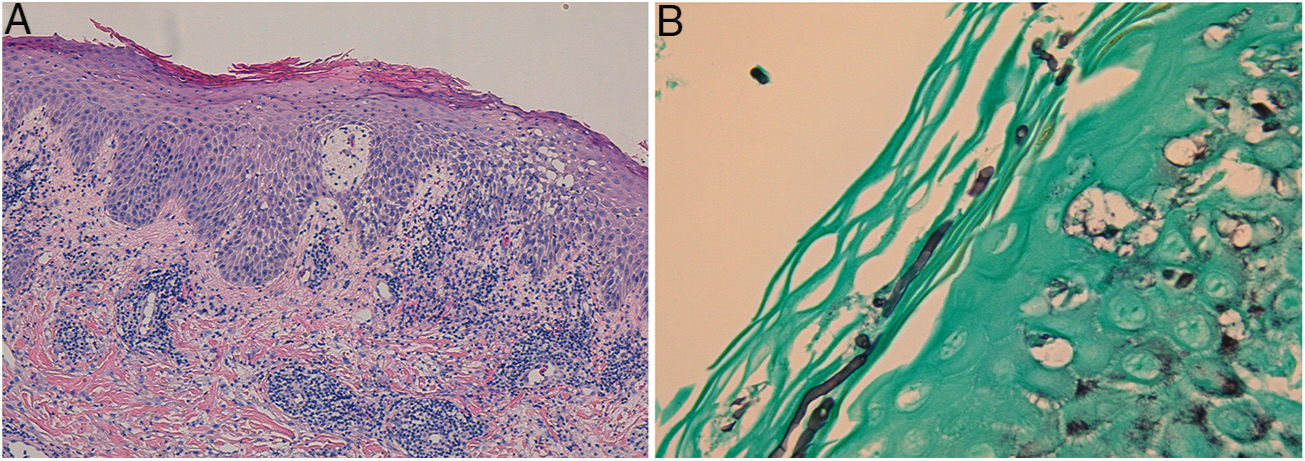
In the direct examination with potassium hydroxide (KOH) and calcofluor white, hyphae were observed. The histological study revealed an epidermis with irregular acanthosis, spongiosis, polymorphonuclear exocytosis and parakeratosis; and a diffuse inflammatory infiltrate that occupied the entire thickness of the dermis, composed of lymphocytes, polymorphonuclear cells, histiocytes, eosinophils and plasma cells (Fig. 2A). Giemsa, FITE and Ziehl–Neelsen stains were negative for microorganisms. Using PAS and Grocott's stains (Fig. 2B) conidia and mycelia were observed in the corneal layer.
A: Epidermis with irregular acanthosis, spongiosis, polymorphonuclear exocytosis and parakeratosis; and a diffuse inflammatory infiltrate occupy the entire thickness of the dermis, composed of lymphocytes, polymorphonuclear cells, histiocytes, eosinophils and plasma cells (haematoxylin-eosin staining). B: Conidia and mycelia in the corneal layer (Grocott's staining).
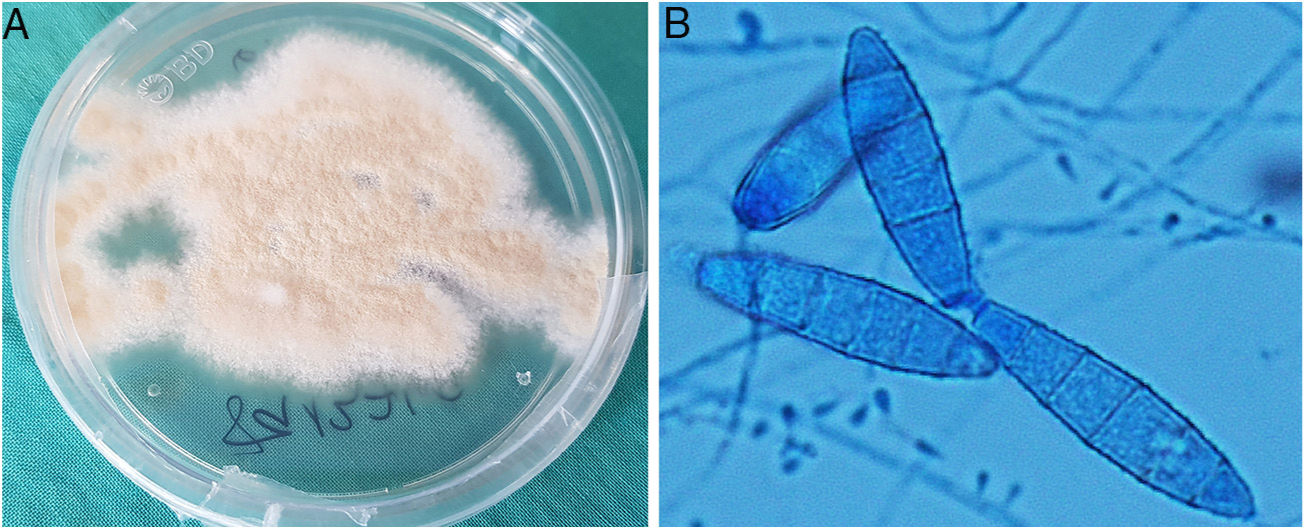
The diagnostic confirmation came from the culture of the biopsy material in Sabouraud agar medium with chloramphenicol and gentamicin at 30°C, in which powdery, flat and light brownish yellow coloured colonies were isolated, which matured after seven days (Fig. 3A). By microscopic examination with lactophenol blue, pyriform microconidia and spindle-shaped macroconidia with rounded, equinulated ends, a thin wall and four to six septa were observed, compatible with Microsporum gypseum (Fig. 3B). The identification of the fungus was confirmed by sequencing the Internal Transcribed Spacer (ITS) region of the rDNA, 100% identical to that of Nannizzia gypsea in GenBank®.
A: Powdery, flat and light brownish yellow coloured colonies, which matured after 7days in Sabouraud agar medium with chloramphenicol and gentamicin at 30̊C. B: Pyriform microconidia and spindle-shaped macroconidia, with rounded, equinulated ends, a thin wall and four to six septa were observed, compatible with Microsporum gypseum (microscopic examination with lactophenol blue).
Given the inflammatory appearance of the skin lesion, it was initially suspected that there could be an invasion of the dermis, so treatment with oral terbinafine 250mg/day and topical ciclopirox olamine two applications/day/for two months was applied, seeking a complete resolution of the cutaneous picture. However, dermal invasion could not be confirmed later on in the histological study.
Final commentM. gypseum, currently called N. gypsea, is part of the M. gypseum complex, which includes the geophilic species N. gypsea, N. fulvum and N. incurvata, practically indistinguishable from each other by morphological studies.1,2 Geophilic dermatophyte infection usually occurs through direct contact with cultivated fertile soil, which is why it occurs more frequently in farmers, gardeners and children. M. gypseum is a rare cause of dermatomycosis, being isolated in Europe, in between 0.04 and 7% of all cases of dermatomycosis.3
Geophilic dermatophyte infection usually presents as a Tinea corporis, with a very intense inflammatory response. Since many other diseases clinically resemble dermatophytoses, examination with KOH and/or culture followed by a morphological, macroscopic and microscopic study of the colonies are necessary to confirm the diagnosis and identify the species. Currently, molecular identification methods based on the sequencing of the ITS region allow the identification of the fungus at the species level.4
As it is an infection limited to the corneal layer, treatment with a topical antifungal is usually sufficient in T. corporis. Systemic antifungal treatment should be used in recurrent or extensive infections, invasion of the dermis and/or subcutaneous tissue, immunocompromised patients or in the event that the scalp is affected.5,6 Recently, dermatoscopic structures that can be observed in the event of an invasion of the hair follicle have been described, such as follicular micropustules and brown spots surrounded by a white-yellowish halo.7
In conclusion, we present a case of N. gypsea (M. gypseum) infection, which is rare in our setting. In spite of the generally benign nature of its clinical manifestations and its low infectivity, it is important to know the existence of this agent to carry out an adequate therapeutic approach. This case report also raises the problem of the inappropriate use of topical corticosteroids, which should only be used after an accurate dermatological evaluation to determine the cause of the skin lesion and the specific treatment for it.
Please cite this article as: Peña Merino L, López Soria L, Acebo Mariñas E, Gardeazabal García J. Infección cutánea tras contacto con aguas residuales. Enferm Infecc Microbiol Clin. 2019;2020:36–37.