This study was aimed at assessing general practitioners’ (GP) reliance on patient history, examination findings and the influence of the utilisation of point-of-care tests (POCT) in antibiotic prescribing for sore throat and lower respiratory tract infections (LRTI).
MethodsAudit-based study carried out in 2015. A group of GPs received an intervention six years earlier with provision of POCTs and another group of GPs acted as controls. Odds ratios for clinical variables predicting antibiotic prescribing were calculated by logistic regression analyses.
ResultsA total of 238 GPs included 1906 patients with sore throat and 1970 LRTIs. A negative POCT result was negatively associated with antibiotic prescribing, with odds ratios ranging from 0.09 to 0.23. GPs using POCTs attached less weight to clinical criteria.
ConclusionGPs using rapid tests are mainly influenced by POCT results in the decision to prescribe antibiotics. However, antibiotic prescribing is still observed with negative POCT results.
El objetivo fue evaluar la influencia de la historia clínica, exploración y uso de pruebas de diagnóstico rápido (PDR) por los médicos de familia (MF) en la prescripción antibiótica en la faringitis e infecciones del tracto respiratorio inferior (ITRI).
MétodosEstudio de auditoría realizado en 2015. Un grupo de MF recibió una intervención 6 años antes con provisión de PDR y otro grupo de médicos actuó como control. Se calcularon odds ratios de predicción de prescripción antibiótica para las variables clínicas mediante análisis de regresión logística.
ResultadosUn total de 238 MF incluyeron 1.906 faringitis y 1.970 ITRI. Un resultado negativo de PDR se asoció negativamente con prescripción antibiótica, con odds ratios entre 0,09 y 0,23. Los médicos asignaron menos peso a los criterios clínicos cuando usaron PDR.
ConclusiónLos MF que usan PRD dan más importancia a sus resultados a la hora de prescribir antibióticos. Sin embargo, aún sigue observándose prescripción antibiótica con resultados negativos de las PDR.
Episodes of sore throat and acute cough due to a lower respiratory tract infection (LRTI) are common reasons for consulting in general practice. Diagnosis for the vast majority of outpatients attending Spanish general practitioners (GP) is generally based on history and clinical examination alone. GPs often prescribe an antibiotic for these patients and may support their decision by the presence of specific symptoms and signs. In the HAPPY AUDIT, a European Commission-funded study, a group of Spanish GPs received an intervention six years earlier with the provision of two point-of-care tests (POCT): rapid antigen detection tests (RADT) for group A streptococcus and C-reactive protein rapid testing (CRP).1 Both POCTs are now recommended by current clinical guidelines in Spain,2,3 but their use is uneven in the different Autonomous Communities, although the use of RADTs has significantly increased over the last years. We recently observed that up to 84.5% of the antibiotics given to patients with sore throat and 69.8% given to patients with LRTI could have been saved with the proper use of rapid tests and good adherence to these guidelines.4 We invited this group of GPs to participate in an audit-based registration in January–March 2015 and a new group of GPs from the same areas acted as the control group. In order to gain insight into the actual diagnostic reasoning and therapeutic decision-making process, we studied the influence of an array of clinical factors recorded in the consultations on GPs decisions whether or not to prescribe an antibiotic for sore throat and LRTIs, hypothesising that GPs using POCTs do not rely upon clinical criteria as much as those GPs not using POCTs.
MethodsNational coordinators from eight Autonomous Communities invited local GPs who had participated in this study in 2008 and 2009. They were again invited to participate in a new registration study over a 3-week period in 2015. All these GPs were requested to register individuals aged 14 or older with sore throat (including acute pharyngitis and tonsillitis) and LRTIs by means of a 47-item chart providing relevant information about the infectious disease. On this sheet, the GP attending the patient noted different specific parameters of medical care, including the age and gender of the patient, the number of days with symptoms, presenting signs, infection severity on a 5-item scale (1: mild, 5: very severe), whether the patient requested an antibiotic, performance of tests, antibiotic treatment or not, and referral to another healthcare setting. GPs were trained in the use and interpretation of POCTs six years earlier and they were then advised to use a POCT in cases of doubt and never as a stand-alone test: RADT only in patients with suspected streptococcal pharyngitis (two or more Centor criteria) and CRP in patients with LRTI with uncertain aetiology. We again provided these POCTs to the consultation offices of these GPs in 2015. A new group of GPs from the same areas who had never participated in courses on the rational use of antibiotics with comparable age, gender, type of job and number of years working to the GPs assigned to intervention were also invited to participate in 2015.
Predictors of antibiotic prescribing were evaluated in those using POCTs and those who did not use them with the use of logistic regression models for each condition (sore throat and LRTIs). In a previous study our group observed that RADTs and CRP should be performed in 37.8% of patients with sore throat and 31.2% of all the LRTIs respectively, as stated by current guidelines in primary care.4 We divided the GPs in two groups: those who used the rapid test, either the RADT or the CRP test in at least 15% of the patients with sore throat and LRTIs, respectively. Ethical approval was granted by the Institut d’Investigació en Atenció Primària Jordi Gol i Gurina, Barcelona, reference number 14/106.
ResultsA total of 121 GPs of the 210 GPs who had participated in the first and second registrations in 2008 and 2009 agreed to participate in the third registration and sent the templates correctly completed (57.6%). A total of 117 GPs clinicians acted as the control group. They included a total of 1906 patients with sore throat and 1.970 LRTIs. RADTs were used by 62 GPs in the intervention group (51.2%) and 10 clinicians in the control group (8.5%). The CRP was used by 55 (45.4%) and one (0.9%) GP, respectively. Antibiotics were prescribed for 801 patients with sore throat (42%), but this percentage was greater among those GPs not using or without access to RADTs, as they prescribed antibiotics in 43.8% of these patients compared to the 38.8% observed among those using rapid tests (p<0.001). Antibiotics were prescribed for 1076 patients with LRTI (54.6). Similarly, this percentage was greater among GPs not using or without access to CRP (57.4% vs. 45.7%, respectively; p<0.001).
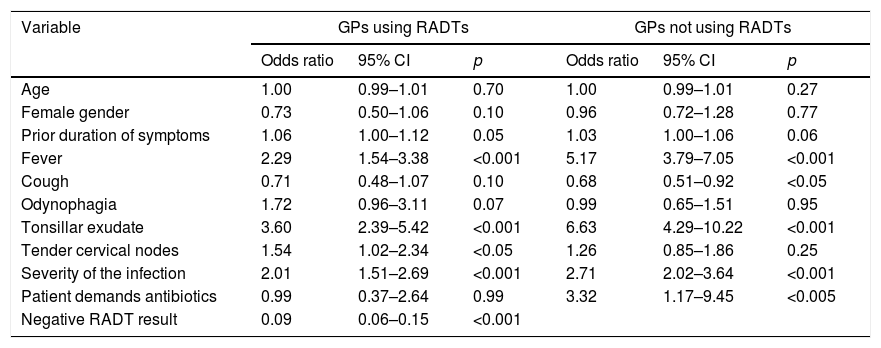
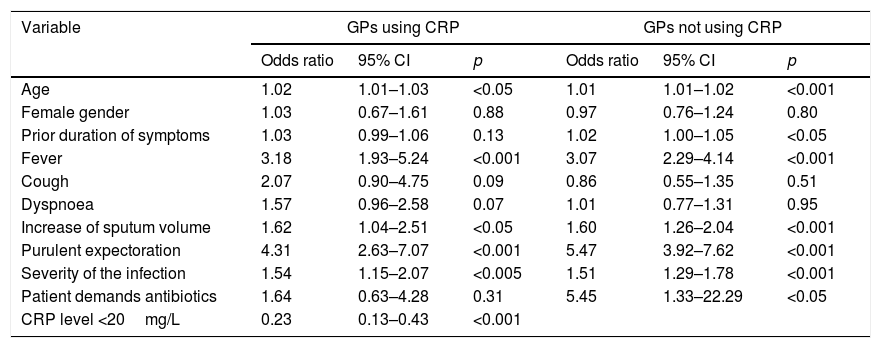
Table 1 describes the predictive value of the different criteria collected in the template on the antibiotic prescribing for patients with sore throat in both group of GPs. The presence of tonsillar exudate was strongly associated with antibiotic prescribing in both groups of physicians, but the association was much stronger among GPs who did not use RADTs. Conversely, a negative RADT result was negatively associated with antibiotic prescribing in the group of physicians using the POCT (OR 0.09). Among GPs using CRP, a low value was the strongest independent predictor of antibiotic prescribing, with an OR of 0.23. The presence of purulent sputum was strongly associated with antibiotic prescribing in both groups of physicians, followed by fever. Interestingly, GPs not using POCT - either RADT or CRP - were more prone to prescribe antibiotics when patients requested an antibiotic compared to their counterparts (Table 2).
Predictors of antibiotic prescribing for patients with sore throat.
| Variable | GPs using RADTs | GPs not using RADTs | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p | Odds ratio | 95% CI | p | |
| Age | 1.00 | 0.99–1.01 | 0.70 | 1.00 | 0.99–1.01 | 0.27 |
| Female gender | 0.73 | 0.50–1.06 | 0.10 | 0.96 | 0.72–1.28 | 0.77 |
| Prior duration of symptoms | 1.06 | 1.00–1.12 | 0.05 | 1.03 | 1.00–1.06 | 0.06 |
| Fever | 2.29 | 1.54–3.38 | <0.001 | 5.17 | 3.79–7.05 | <0.001 |
| Cough | 0.71 | 0.48–1.07 | 0.10 | 0.68 | 0.51–0.92 | <0.05 |
| Odynophagia | 1.72 | 0.96–3.11 | 0.07 | 0.99 | 0.65–1.51 | 0.95 |
| Tonsillar exudate | 3.60 | 2.39–5.42 | <0.001 | 6.63 | 4.29–10.22 | <0.001 |
| Tender cervical nodes | 1.54 | 1.02–2.34 | <0.05 | 1.26 | 0.85–1.86 | 0.25 |
| Severity of the infection | 2.01 | 1.51–2.69 | <0.001 | 2.71 | 2.02–3.64 | <0.001 |
| Patient demands antibiotics | 0.99 | 0.37–2.64 | 0.99 | 3.32 | 1.17–9.45 | <0.005 |
| Negative RADT result | 0.09 | 0.06–0.15 | <0.001 | |||
CI: confidence interval; GP: general practitioner; RADT: rapid antigen detection test.
Predictors of antibiotic prescribing for patients with lower respiratory tract infections.
| Variable | GPs using CRP | GPs not using CRP | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p | Odds ratio | 95% CI | p | |
| Age | 1.02 | 1.01–1.03 | <0.05 | 1.01 | 1.01–1.02 | <0.001 |
| Female gender | 1.03 | 0.67–1.61 | 0.88 | 0.97 | 0.76–1.24 | 0.80 |
| Prior duration of symptoms | 1.03 | 0.99–1.06 | 0.13 | 1.02 | 1.00–1.05 | <0.05 |
| Fever | 3.18 | 1.93–5.24 | <0.001 | 3.07 | 2.29–4.14 | <0.001 |
| Cough | 2.07 | 0.90–4.75 | 0.09 | 0.86 | 0.55–1.35 | 0.51 |
| Dyspnoea | 1.57 | 0.96–2.58 | 0.07 | 1.01 | 0.77–1.31 | 0.95 |
| Increase of sputum volume | 1.62 | 1.04–2.51 | <0.05 | 1.60 | 1.26–2.04 | <0.001 |
| Purulent expectoration | 4.31 | 2.63–7.07 | <0.001 | 5.47 | 3.92–7.62 | <0.001 |
| Severity of the infection | 1.54 | 1.15–2.07 | <0.005 | 1.51 | 1.29–1.78 | <0.001 |
| Patient demands antibiotics | 1.64 | 0.63–4.28 | 0.31 | 5.45 | 1.33–22.29 | <0.05 |
| CRP level <20mg/L | 0.23 | 0.13–0.43 | <0.001 | |||
CI: confidence interval; GP: general practitioner; CRP: C-reactive protein.
The present study demonstrates that GPs using rapid tests pay more attention to the result of the POCT when deciding whether to prescribe or not antibiotics for sore throat and LRTIs. Interestingly, GPs using POCTs are more confident not to prescribe antibiotics when a patient requests an antibiotic.
This study has several limitations. GPs participated on a voluntary basis and their prescribing habits may not represent the average use of antibiotics in our country. A registration such as that used in our study might not have contained all the variables needed for making a therapeutic decision. For instance, auscultation findings were not included in this study. Although crackles and bronchial breathing are traditionally believed to be associated with pneumonia,5,6 recent evidence shows that these findings are also commonly observed in acute bronchitis.7 The strength of our study is its large sample size with detailed documented consultations, which enabled comparison of the predictive value of the different criteria collected in the template between GPs using and not using POCTs.
Diagnostic uncertainty and over reliance on specific clinical criteria have been identified as reasons for antibiotic overprescribing.8 However, systematic reviews of therapeutic trials have demonstrated that possible benefits of antibiotic treatment do not outweigh the disadvantages for most people with sore throat and LRTIs.9,10 One of the striking results is the different weight GPs allocate to the different clinical criteria. Although the Centor rule gives one point for each of the four criteria,11 Spanish GPs consider that some of these criteria are more predictive for streptococcal infection than others, giving more importance to the presence of pharyngeal or tonsillar exudates rather than other criteria. This is shown in both groups of physicians in our study but is more strongly associated among clinicians not using RADTs. Regarding LRTIs, GPs are more prone to consider antibiotic prescribing when sputum purulence is present, also found in both groups of clinicians. Similarly, this association was stronger among those not using CRP, as also shown in other studies.12 This is the result of misunderstandings many GPs still have regarding the different weight of some clinical criteria. However, GPs using POCTs gave more importance to the rapid test results on the decision whether or not to prescribe antibiotics for both sore throat and acute cough due to a LRTI. Notwithstanding, some cases of negative POCT results were associated with unnecessary antibiotic prescribing. This inappropriate antibiotic prescribing has also been observed in other areas such as in Scandinavia, where POCTs have been widely used, but constant interventions targeting GPs has resulted in a significant decrease of unnecessary prescribing.13,14 This gap in the evidence base is important because understanding the influence of clinical factors on antibiotic prescribing and identifying whether or not these factors influence prescribing appropriately could lead to widespread changes in clinical decision making in the direction of more evidence-based antibiotic prescribing.
FundingThis study was funded by TRACE (Translational Research on Antimicrobial resistance and Community-acquired infections in Europe). The funding body had no role in the design, execution or reporting of the study.
Conflict of interestsCL and AM report receiving research grants from Abbott Diagnostics. The other authors have nothing to declare. JMM has received financial support for two studies from GSK and Gilead respectively.