A 34-year-old man, originally from Colombia, habitually residing in Spain, smoker and cocaine user, with known HIV infection since 2013 and acquired sexually (MSM), went to the accident and emergency department due to intense proctalgia, discharge and rectal tenesmus for four days. In addition, he had a low-grade fever, the appearance of several perianal lesions and some pruritic papules distributed over his trunk, arms and palms. As an important piece of information, he reported unprotected sexual intercourse with a healthy man during the prior two weeks. In the anamnesis, he denied contact with animals or ill people and having recently travelled abroad.
At his last check-up, the patient reported that he had good adherence to antiretroviral treatment (DTG + 3TC) and good immunovirological control.
On physical examination, he manifested an acceptable general condition and stable vital signs (BP: 113/65; HR: 72; Temp.: 36.9 °C; SatO2: 98%). At the cutaneous level, perianally-dispersed pustular lesions with a necrotic centre and raised edges were observed, some suppurative (Fig. 1) and isolated papules on the trunk and upper limbs (Fig. 2), including palms. Furthermore, bilateral inguinal lymphadenopathies with a reactive appearance were palpable, anoscopy revealed an inflamed, intensely ulcerated and friable mucosa with abundant pus and bleeding, and a biopsy of one of the perianal lesions was obtained (Fig. 3).
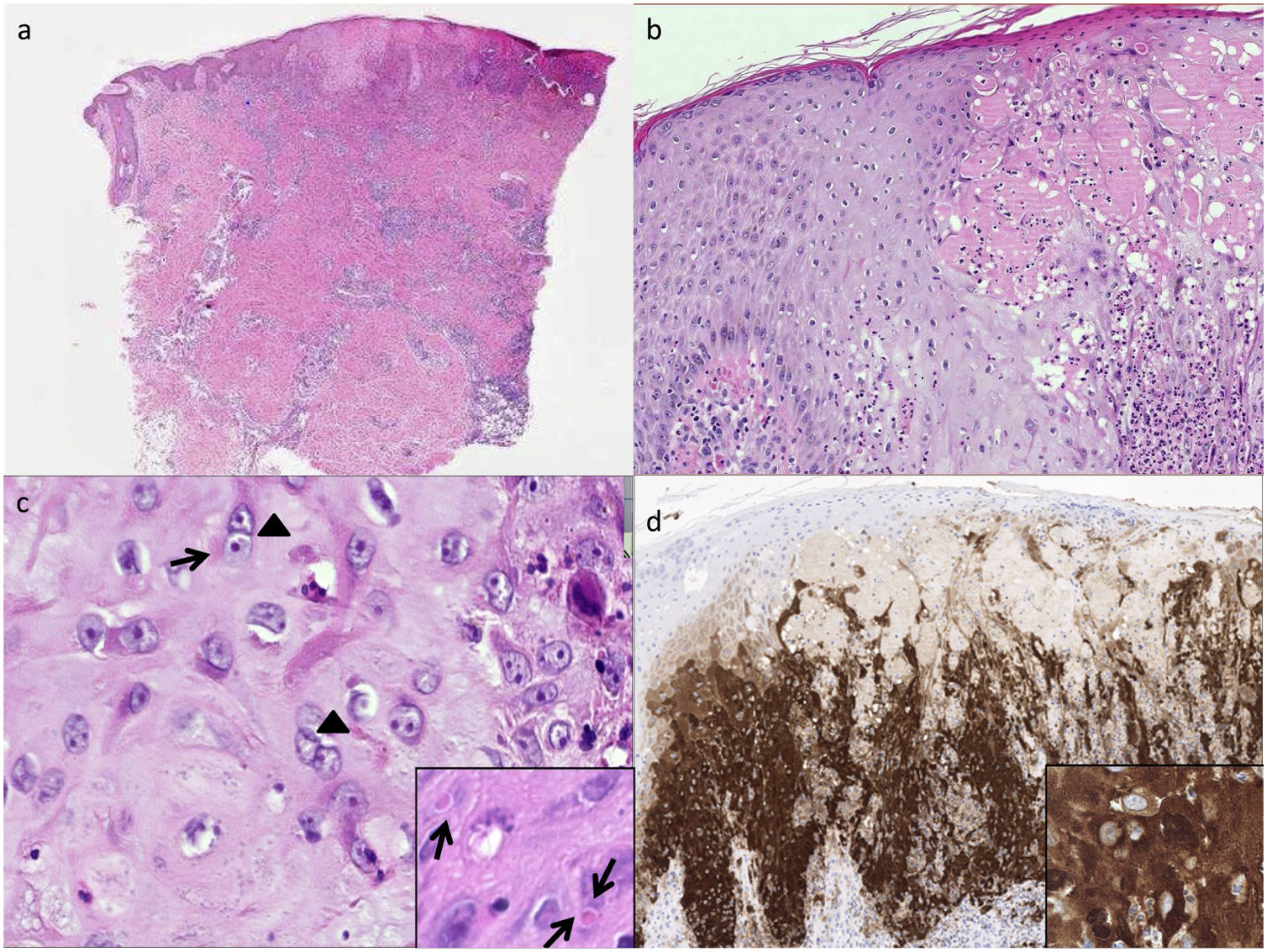
a) Skin showing an ulcerated area; b) The epidermis showing mild acanthosis, mixed-type exocytosis and debris; c) “ballooned” keratinocytes, with multinucleation (with 2 and 3 nuclei — arrowheads). A “basophilic halo” is observed in the nucleus of some keratinocytes. In greater detail Guarnieri bodies (indicated with arrows); d) Vaccinia immunohistochemistry.
Nontreponemal study/testing completed for syphilis was negative, as well as for Epstein-Barr virus, varicella zoster and herpes simplex virus I and II. A sample was collected to carry out a multiplex polymerase chain reaction (PCR) test, which ruled out herpes zoster, cytomegalovirus, Haemophilus ducreyi, Chlamydia trachomatis, Treponema pallidum and herpes simplex virus I and II. The anal exudate collected was negative for all the microorganisms tested, as well as the blood cultures obtained during the patient’s febrile phase. Finally the PCR for monkeypox (Orthopoxvirus) was positive for the monkeypox virus and the pathology study (Fig. 3) described skin with an ulcerated area, epidermis with mild acanthosis, mixed-type exocytosis and debris, “ballooned” keratinocytes, with multinucleation; a “basophilic halo” was observed in the nucleus of some keratinocytes.
With the microbiological and pathological diagnosis of the infection, it was decided to isolate the patient, and thus avoid contact with other people. Analgesia was administered, achieving progressive clinical improvement. Ten days later, the skin lesions disappeared, after going through a phase with a scabbed appearance, and the clinical signs and symptoms of proctitis resolved. Secondary to this condition, seroconversion of hepatitis C serology was observed with a silent increase in transaminases and a detectable hepatitis C virus (HCV) viral load, all of which was consistent with acute hepatitis C.
In conclusion, the monkeypox virus is a zoonotic infection, which has recently affected a multitude of patients around the world in a few days, causing a scientific and health alert.1,2 Its person-to-person dissemination differs from classical smallpox in that it is transmitted through direct contact with sores, scabs or bodily fluids,3 and the lesions it produces may have a similar appearance to the more common infectious rashes, such as those seen in secondary syphilis, herpes simplex infection4 and varicella zoster virus infection.5 The epidemiological factor and the appearance of the lesions are therefore determining factors in diagnosing this infection.6,7