Patients in the hospital should be treated promptly. It will improve the quality of services and patient safety. The objective of this paper is to investigate factors affecting patient assessment response in nursing practice based on a review of the literature.
MethodA systematic review was utilized. The article was conducted using online databases, reference lists of key articles, and expert advice. Multiple keyword combinations were used. All relevant studies were subsequently appraised for rigorous and quality.
ResultsEleven articles were critically appraised. The results show that there are six factors that affect patient assessment responses: (1) high specific competences; (2) clinical experiences; (3) patient safety culture; (4) education level; (5) team collaboration; and (6) medical systems. High specific competence of nurse is significant affected the patient assessment response.
ConclusionFactors that enhancing nurse's assessment response should be special attention in health care services. Nurses manager have a substantial role in enhancing response assessment of nurses’ practitioner.
Patients in the hospital should be treated promptly. The most frequent hospital health care workers are nurses. The nurse must be able to take action immediately in responding to the patient's presence. The nurse's initial action is patient assessment.1 Assessment is the foundation of effective nursing care, improved patient outcomes may result from any strategy that enhances patient safety.2 An appropriate and rapid assessment will improve patient safety.1,2 It has many challenges in nursing practice, especially to see the complexity of health services in hospitals and the high workload of a nurse.
In addition, to improve patient safety, the assessment will give complete information which is used by nurses to make a decision quickly and accurately.3 It will prevent the occurrence of a medical error. According to Levett-Jones et al., these findings are important because clinical judgment is an imperative, not only in the collection of cues and recognition of changes in the patient, but also in processing information, initiating the medical intervention, and evaluating outcomes.4
Shubert describes three components to patient safety as it relates to failure to rescue events that occur in the hospital: inaccuracy of nursing assessments, lack of detection of clinical abnormalities/changes in patients, and lack of ability to pull the pieces together/problem recognition. In addition, once problems are identified by nurses, the nurse may be slow in reporting the changes to the providers and providers may not act or respond quickly to the information they receive.3 Seeing the importance of patient assessment, the improvement of the patient assessment is required by nurses to keep the quality of services.
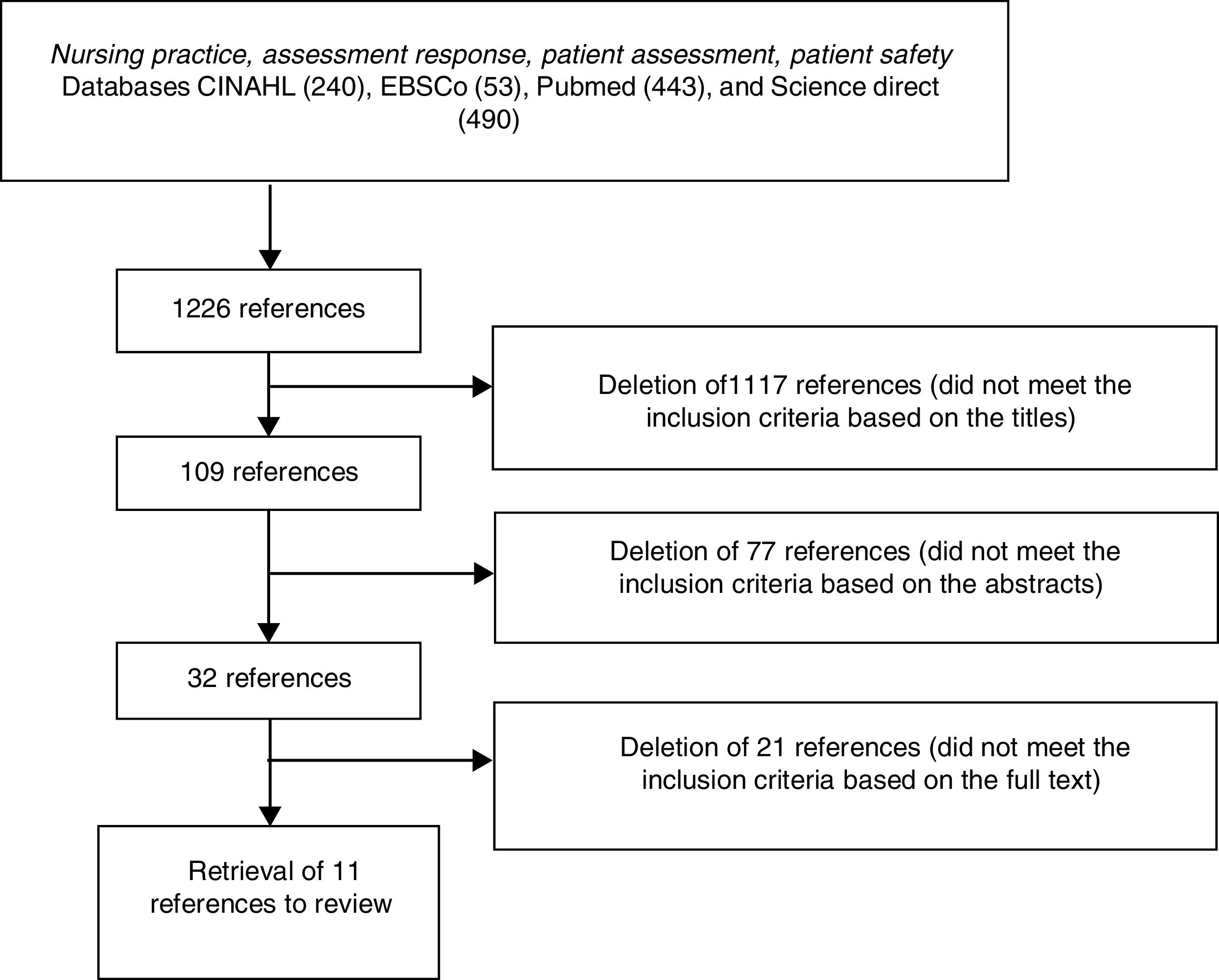
MethodA systematic review was conducted. The articles were conducted using online databases: Cumulative Index to Nursing and Allied Health Literature (CINAHL), EBSCo, Pubmed, and ScienceDirect. A combination of various keyword included assessing, patient assessment, patient safety, nursing practice, assessment response, and nurses’ response.
Literature selection was determined by the following inclusion criteria: (1) focused on patient assessment response, (2) published between 2007 and 2017, (3) published in English, (4) related to the assessment competencies in the study of title and abstract, (5) articles which are the study sample was nurses at hospitals, and (6) the methodology that was used was cross-sectional, cohort, descriptive, exploratory, qualitative, and mixed method. Exclusion criteria were articles that focused on specific or particular competencies, such as cultural, safety, or information technology competencies; and the study sample was anyone other than nurses such as nursing students or doctors.
ResultsInitially, 240 articles in CINAHL, 53 articles in EBSCo, 443 articles in Pubmed, and 490 papers in ScienceDirect were found in the systematic review. The 1226 articles selected during the search, eleven papers found in the inclusion criteria and were subsequently included. Details of the article selection process are shown in Fig. 1.
Table 1 describes the methods and materials of the studies, including in our review. Three studies (27.3%) applied the exploratory design. More than half of them used the quantitative method. In most studies, the data were collected using a questionnaire (n=4, 36.4%).
Characteristics of studies reviewed.
| Item | Characteristic | n | % |
|---|---|---|---|
| Study design | Cross sectional | 2 | 18.2 |
| Development of the questionnaire | 1 | 9 | |
| Exploratory design | 3 | 27.3 | |
| Descriptive design | 3 | 27.3 | |
| Cohort design | 2 | 18.2 | |
| Method | Quantitative | 6 | 54.5 |
| Qualitative | 3 | 27.3 | |
| Mixed | 2 | 18.2 | |
| Data collection | Questionnaire(s) | 4 | 36.4 |
| Structured interview | 3 | 27.3 | |
| Semi-structured interview | 1 | 9 | |
| Several different instruments, 2 or more | 3 | 27.3 | |
| Instrument | Previously validated, literature reference | 4 | 36.4 |
| Previously used, literature reference | 3 | 27.3 | |
| Self-constructed, no mention about pilot study | 2 | 18.1 | |
| No description of the development or quality control of the questionnaire | 2 | 18.1 | |
| Sample size | <50 | 6 | 54.5 |
| 50–100 | 1 | 9.1 | |
| 101–200 | 1 | 9.1 | |
| >200 | 3 | 27.3 | |
The tools used for data collection were previously validated literature reference. Two studies provided no account of how the tool had been developed or from its validity. Study populations of more than 200 respondents were reported in 3 studies (27.3%).
Six factors were found that affect the patient assessment response in nursing practice. Forty percent of the sample indicated that high specific competence influenced patient assessment response.
High specific competence. Four articles specifically describe a nurse's specific competence, it influences assessing the patient,5 establishing nurse–patient relationships,6 and nurturing family–nurse relationships.7 The four explain the impact of specific competencies of nurses that improves nurse assessment response to the patient.
Clinical experience. Two articles suggest that clinical experience will impact on the nurse's response in assessing the patient.8,9 Both of these articles suggest that nurses with longer clinical experience will influence the decision making of a nurse that determines the length of the nurse's response in providing assessments and nursing actions.
Patient safety culture. The safety culture of a patient owned by the nurse affects the nurse's response in providing patient assessments.4 In addition, the patient safety culture of organizations will impact on the prevention of injury to the patient through the assessment which is fast and precise.10 Both of these articles indicate that organizations and employees should support each other in improving quality and patient safety, the better the value will increase the response of nurses in providing assessments to patients.
Education level. The level of education determines nurses to make decisions and has ability rather than the lower education level of nurses.11 The high level of education demonstrates good theoretical and analytical skills.
Teamwork. The defining factor in giving a good services to patients is teamwork between doctors, nurses, and other health workers in hospital.12 Better teamwork will increase assessment response to patients.13
Medical system. Two articles mention that the better and sophisticated medical system owned by a hospital will improve the response time of health workers, especially nurses in giving action. It will also reduce patient mortality and improve service quality.14,15
DiscussionIt was shown in our systematic review that six factors affected the development of nurses’ assessment that takes place in the emergency room, inpatient room, and community health services.
Clinical competency is an important part of safety patient care. One study in Korea asked 335 nurses to complete a questionnaire about their professional quality of life, their clinical competency, and personal characteristics. The results showed that nurses who had high clinical competence also scored high in compassion and satisfaction, and low in professional burnout.16 The high nurses’ clinical competency is significantly impacting when the nurse interacts with the patient. The nurse will be able to foster the relationship to the patient4,6 and nurturing nurse–family relationship.7 Nurtured Nurse–Patient and Nurse–Family relationship will facilitate the nurses in conducting assessments.
A nurse with two to three years of work experience, at least in similar day-to-day situations, can reach the competent stage. Proficient nurses perceive and understand situations as whole parts to improve their decision-making.16 Expert nurses exhibit performance that is fluid, flexible, and highly proficient.17 An experienced nurse finds more clinical problems at the hospital, so the nurse will do calmly and expertly. An experienced nurse will work quickly and capably, able to care for a highly complex both in the emergency room or inpatient room.
Forsberg et al. (2014) said that experienced nurses while finding the same case from previous experience will be easy to decide to act the nursing process. Similarly, when nurses carry out difficult assessments such as when assessing pain in pediatric patients, with experience, nurses will more easily assess the patient.9 Clinical experience will be very useful for the nurse in determining the intervention process.
An organization should have good and correct patient safety culture guidelines.4 The incomplete guideline will cause a nurse to make wrong decisions affecting medical error.18 A good and correct guideline is made by nurses’ manager and officials of the hospital in which it covers all aspects required by the patient in terms, such as patient data. This affects the nurses’ ability to make diagnose decisions and actions to be performed.
A good patient safety culture will grow nurses’ self-awareness to prevent patient injury.10 The safety culture will raise awareness to prevent errors and report any errors.19,20 Implementing a patient safety culture will give some benefits to patients and health care providers. The patient will feel safe at the hospital, and there will be no greater expense due to an extended period of stay. Implementing patient safety culture will prevent medical errors.
Education influences expertise by providing a theoretical and practical knowledge base that can be tested and refined in actual situations16 – nurses whose diploma degree had lower competences than nurses whose bachelor degree.21 Nurses with a Master's degree were well equipped to care for patients compared to those with a Bachelor's or diploma.22 The role of education in developing nurses’ competencies is important in nursing process.23 The high level of education is directly proportional power to analyze and determine the case based on the theory gained during the lecture. In other words, the higher the education, the better the nurse in assessing the patient.
The higher education will have a better mastery of theory and principles enable nurses to ask the right questions to hone in on patient problems to provide safe care and make good clinical decisions.11 The collective education level of staff may impart a unique contribution to the development of expertise in the clinical setting.16 However, many management hospitals that recruited nursing staff still prefer diploma than a bachelor of nursing because of cost efficiency.
Assessment in patients requires good cooperation between health workers in hospitals. Good cooperation between nurse–doctor, nurse–pharmacist, nurse–nutritionist, etc. will shorten the time in the assessment as well as improve the accuracy of the data so that in making decisions far from the risk of injury.12,13 The key of teamwork to prevent medical error is the communication factor. Communication between health workers and other units should be used an open and clear communication. Communication is not only by speak, but in writing also must contain clear information.
The medical systems such as hospital-owned facilities can support the patient's initial documentation process. The medical system that a hospital often uses these decades is technology-based documentation. This innovation will generally improve the response time of a health worker in conducting a rapid assessment of patients, especially patients in emergencies.14,24 Furthermore, in a retrospective study conducted by Blanchard, the technology-based system will reduce mortality rates for emergency patients and prevent injury risk in patients.24
Some of the above factors should become the concern of hospital institutions, especially in terms of patient safety improvement. A substantial role is also required of a nursing manager in implementing and improving the nurse's response assessments, especially in facilitating the nurses to improve their abilities. This will certainly improve the quality of patient safety in health services.
Conflict of interestsThe authors declare no conflict of interest.
This work is supported by Hibah PITTA 2017 funded by DRPM Universitas Indonesia No. 386/UN2.R3.1/HKP.05.00/2017.
Peer-review under responsibility of the scientific committee of the Second International Nursing Scholar Congress (INSC 2018) of Faculty of Nursing, Universitas Indonesia. Full-text and the content of it is under responsibility of authors of the article.