The care plan of a 42-year-old woman with anaphylactic shock, secondary to ingestion of amoxicillin/clavulanic acid, with upper airway involvement due to laryngeal angioedema, is presented. Previously she had had two episodes of angioedema of unknown origin. The incidence of this phenomenon is between 3.2 and 10 cases/100,000 people/year.
Clinical observationAn evaluation was made and three altered necessities stood out: breathing and circulation (she needed mechanical ventilation and noradrenalin perfusion), elimination (she required furosemide to keep an acceptable diuresis time), and hygiene and skin protection (she presented generalised hyperaemia, lip, lingual and oropharyngeal oedema).
The hospital's Clinical Research Ethics Committee requested the patient's informed consent to access her clinical history.
InterventionsAccording to the altered necessities, seven diagnoses were prioritised according to NANDA taxonomy: risk of allergic response, risk of infection, risk of ineffective renal perfusion, decreased cardiac output, impaired spontaneous ventilation, risk of unstable blood glucose level, and risk of dysfunctional gastrointestinal motility.
Discussion and conclusionsScores of outcome criteria showed a favourable evolution after 24h. The development of a standardised NANDA-NOC-NIC language in the clinical case presented allowed us to organise the nursing work, facilitating recording and normalising clinical practice. As a limitation of this case, we did not have serial plasma levels of histamine and tryptase to assess the evolution of anaphylactic symptoms. Highlight the importance of health education in a patient with a history of angioedema.
Se presenta el plan de cuidados de una señora de 42años con shock anafiláctico secundario a la ingesta de amoxiclavulánico, con compromiso de la vía aérea superior por angioedema de laringe. Previamente tuvo 2 episodios de angioedema. La incidencia de este fenómeno oscila entre 3,2 y 10casos/100.000 personas/año.
Observación clínicaSe realizó una valoración donde destacaron tres necesidades alteradas: respiración y circulación (precisó ventilación mecánica invasiva y perfusión de noradrenalina), eliminación (requirió furosemida para mantener diuresis horarias aceptables) e higiene y protección de la piel (presentó hiperemia generalizada, edema labial, lingual y orofaríngeo).
El Comité de Ética de Investigación Clínica del Hospital solicitó el consentimiento informado de la paciente para el acceso a la historia clínica.
IntervencionesDe acuerdo con las necesidades destacadas, se priorizaron siete diagnósticos según la taxonomía NANDA: riesgo de respuesta alérgica, riesgo de infección, riesgo de perfusión renal ineficaz, disminución del gasto cardíaco, deterioro de la ventilación espontánea, riesgo de nivel de glucemia inestable y riesgo de motilidad gastrointestinal disfuncional.
Discusión y conclusionesLos criterios de resultados evidenciaron una evolución favorable pasadas 24h. El desarrollo del lenguaje estandarizado NANDA-NOC-NIC en el caso clínico presentado nos permitió organizar metodológicamente el trabajo enfermero, facilitando el registro y normalizando la práctica. Como limitación, no se dispuso de niveles plasmáticos de histamina y triptasa para valorar la evolución del cuadro anafiláctico. Destacar la importancia de la educación sanitaria en una paciente con antecedentes de angioedema.
There is currently no definition for anaphilaxis1–3 nor is there any consensus about the criteria for diagnosis.1,2 The European Academy of Allergy and Clinical Immunology defines anaphylaxis as a severe, life-threatening generalised or systemic hypersensitivity reaction.1,3 The presence of circulatory instability (anaphylactic shock) is potentially life threatening1,4,5 when it compromises the airways.4,5 The need for artificial ventilation means they need to be admitted to the intensive care unit (ICU).6
The incidence rate ranges from 3.2 to 10 in 100,000 people/year, with a mortality rate that reached 6.5%. Evans and Tippins3 have confirmed that the right knowledge and handling of anaphylaxis can prevent it from escalating into anaphylactic shock.
The main causes of anaphylaxis vary according to age1,5,6: medication among adults, food in paediatric patients and insect stings.1,5 Other documented causes are latex and physical stimuli (exercise or cold).7
In order of prevalence, the affected organs are the following7:
- •
Skin and mucous membranes (80–90% of cases): local or diffuse erythema, itching, rash, hives and/or angioedema.
- •
Respiratory system (70%): itchy and blocked nose, sneezing, itching or pressure in the throat, coughing, wheezing and/or dyspnoea.
- •
Gastrointestinal tract (30–40%): nausea, vomiting, cramp and/or diarrhoea.
- •
Cardiovascular system (10–45%): low blood pressure that can lead to fainting; tachycardia and/or cardiac arrhythmias.
- •
Central nervous system (10–15%): migraines, convulsions and/or changes to the mental state.
- •
Others, less frequent: sudden death, uterine contractions, loss of muscle tone in the sphincter, loss of vision/or ringing in the ears.
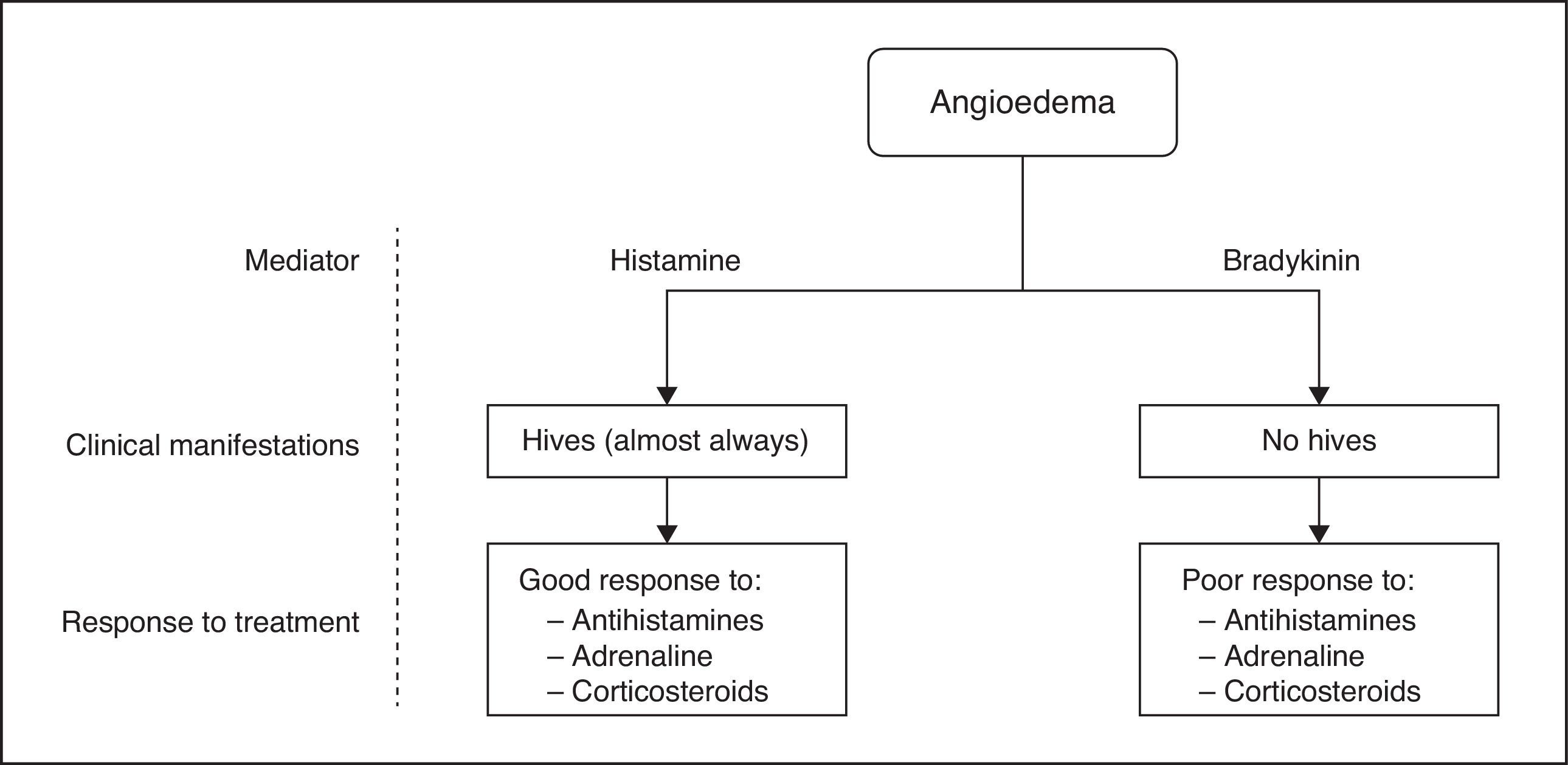
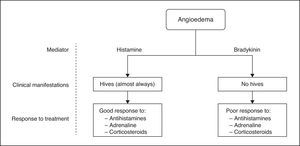
The severity of the anaphylactic reaction is related to the speed at which the symptoms progress, the type of antigen, the route of entry and the affected organs. Factors such as old age, the presence of associated cardiovascular or respiratory conditions (especially asthma), treatment with angiotensin-converting enzyme inhibitors or beta-blockers, or underlying mastocytosis are associated with severe reactions and a higher mortality rate. Severe anaphylaxis is defined by the presence of cyanosis, haemoglobin saturation (HbSat)≤92% (94% in children), low blood pressure, confusion, low muscle tone, loss of consciousness or incontinence. Angioedema (Fig. 1) is the clinical manifestation of anaphylaxis that could potentially have more complications: the sudden and temporary inflammation of some areas of the dermis, subcutaneous tissue and mucous membranes,1,3,5,6,8 after a rise in capillary permeability, which causes liquid to pass from the intravascular space to the interstitial space,5,6,8 and which, if it affects the airways, could compromise their permeability.3–6,8
Presentation of the caseA woman aged 42 admitted to the ICU for anaphylactic shock after ingesting co-amoxiclav due to pharyngitis.
Personal medical historyAngioedema in 2013 (treated with corticosteroids and adrenalin), arterial hypertension treated beta-blockers, iron-deficiency anaemia treated with iron sulphate, underactive thyroid due to Hashimoto's thyroiditis being treated with levothyroxine sodium, Beta-thalassemia and anxiety disorder.
When the ambulance service arrived at her home she showed a 3 on the Glasgow coma scale, low blood pressure and absent peripheral pulse with electrical activity on the monitor. The family reported a situation with a lack of air and fainting after taking the medication. Orotracheal intubation made difficult due to the severe oedema in the glottis, requiring the use of a Fastrach laryngeal mask©. Capillary blood glucose: 97mg/dl. The ambulance service administered intramuscular adrenaline, intravenous corticosteroids and started midazolam infusion. When she arrived at the hospital she needed a noradrenaline infusion. She had hyperaemia, labial, lingual and oropharyngeal oedema, isocoria and photoreactive pupils. HbSat at 98%.
Regular medication: atenolol 50mg c/24h and levothyroxine sodium 175mg c/24h.
Nursing assessmentAssessment of Virginia Henderson's 14 basic needs upon arrival at the ICURespiration and circulationRespiration. The endotracheal tube was changed for a size 7 with subglottic aspiration. Controlled mechanical ventilation. Upper airway stenosis due to angioedema. Poor adaptation to mechanical ventilation, therefore it was necessary to start propofol infusion and muscle relaxant bolus. Blood gases: FiO2 at 0.35; pH: 7.35; PCO2: 47mmHg; PO2: 106mmHg; HCO3−: 25.9Mmol/l; mmol/l; HbSat: 98%. Endotracheal secretions with blood and mucopurulant discharge; the cultures gave a positive result for Escherichia coli, and treatment with levofloxacin was started at 500mg every 24h.
Circulation. Mild sinus tachycardia (103beats/min), requiring noradrenaline infusion at 0.42μg/kg/min to keep average artery pressure above 80mmHg (removed after 48h). Bilateral peripheral pulses present and capillary refill below 2s.
Food and drinkWearing a Salem nasogastric tube curving downwards with bile bag; after 48h, this was replaced with a Silk to start enteral nutrition. She occasionally needed metoclopramide due to gastroparesis.
Arterial blood glucose level: 226mg/dl, rapid-acting subcutaneous insulin started every 6h.
BMI: 31.84kg/m2 (type i obesity).
EliminationWearing a Foley vesical catheter. Due to the persistence of partial hourly diuresis<0.5ml/kg/h 10mg of furosemide were added every 8h.
Movement and maintaining the correct positionLying on her back with cushions beneath her feet to avoid club foot and beneath her arms to avoid oedemas in the downward facing areas.
Sleep and restSedation and analgesia with midazolam and morphine hydrochloride infusions and paracetamol and metamizole alternating every 6h; even still, reacting to physical stimuli. The Richmond Agitation Sedation Scale varies between −4 and −3. Pain assessed by visual analogue scale: not assessable.
After tubes were removed she presented anxiety. Started on 10mg of intravenous clorazepate every 8h.
Maintaining body temperatureNormothermic (36°C). Leucocyte formula changed due to the pharyngitis (leukocytes: 31,000/l; neutrophils: 85%; lymphocytes: 10%; eosinophils: 0%).
Personal hygiene maintenance and skin protectionWarm skin, generalised hyperaemia which went down over the course of some days. Correct hygiene situation, euhydration and without damage. EMINA scale 14.
Risk preventionWhen hospitalised, there was another suspected allergic reaction after administering propofol and atropine (administered due to continued bradycardia) after seeing another episode of generalised hyperaemia.
Needs not assessable due to sedation: dress and undress, communication, worship and personal values.
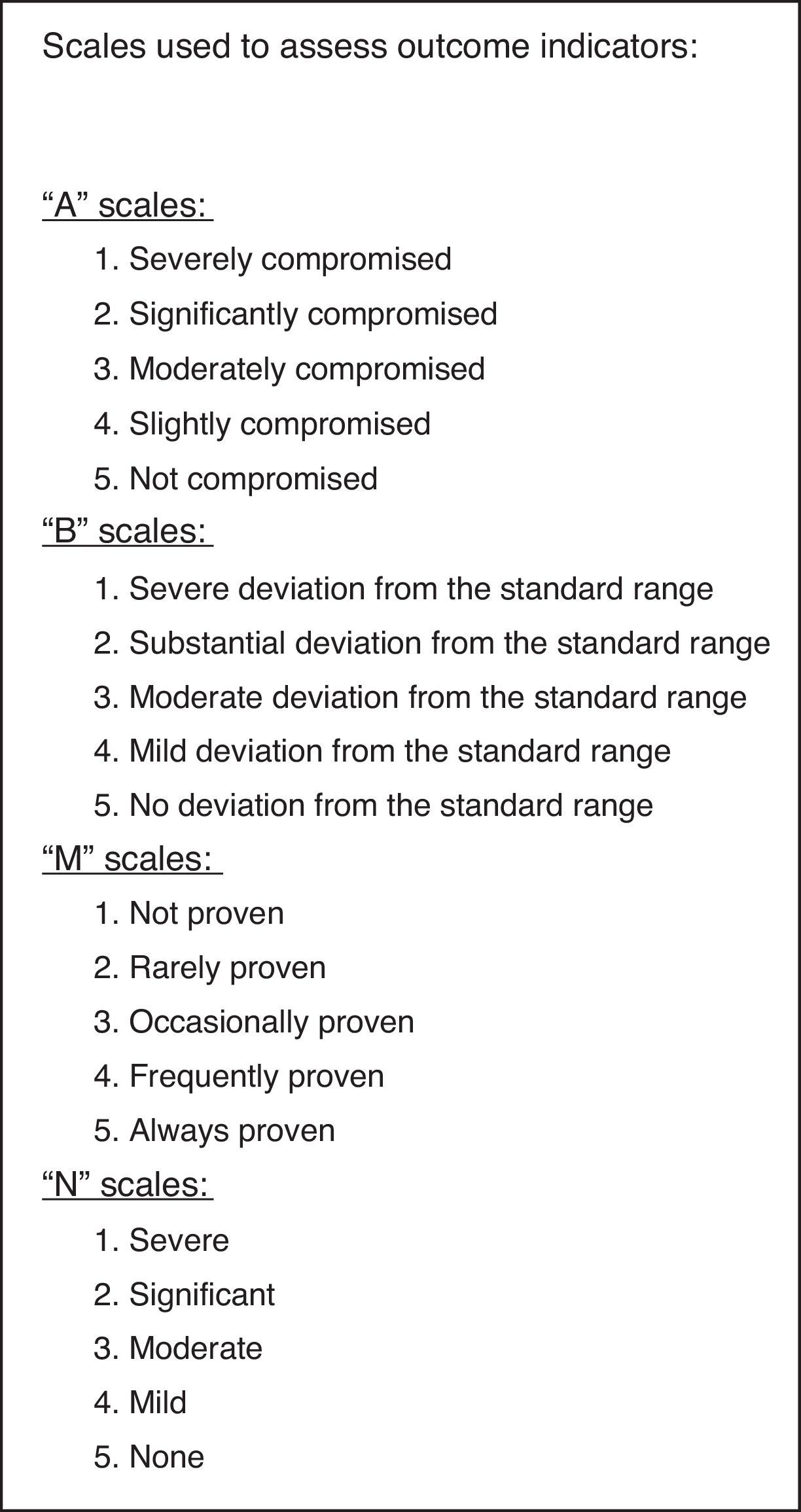
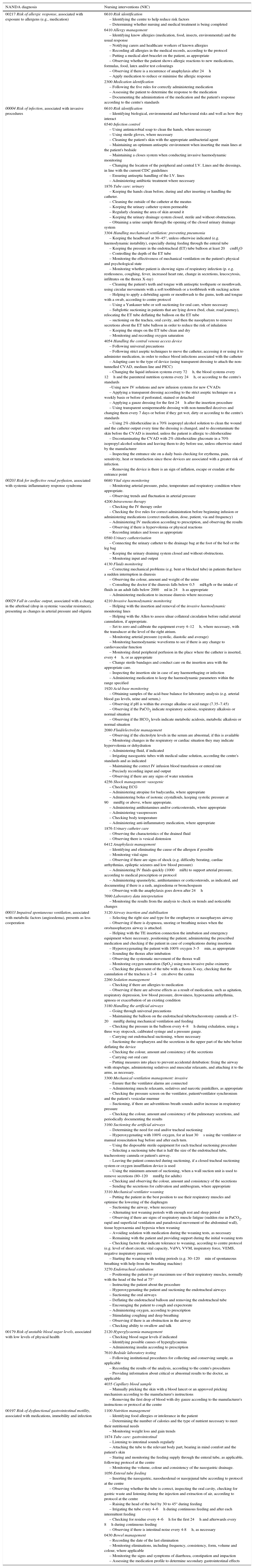
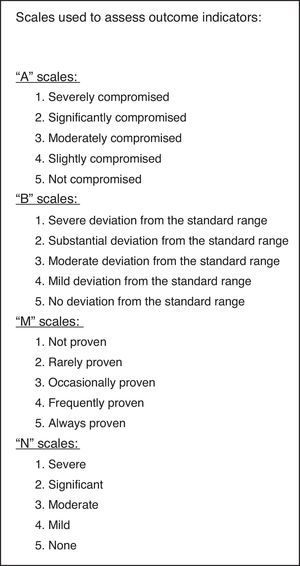
Care planaTable 1 shows the diagnosis labels, actions and nursing activity in the care plan, according to the NANDA and NIC categories. Fig. 2 contains the Likert scales used to assess the indicators in the results. Table 2 shows the relationship between the NANDA, NOC and indicators in the results
Diagnosis, interventions and nursing activity according to NANDA and NIC categorisation.
| NANDA diagnosis | Nursing interventions (NIC) |
|---|---|
| 00217 Risk of allergic response, associated with exposure to allergens (e.g., medication) | 6610 Risk identification – Identifying the centre to help reduce risk factors – Determining whether nursing and medical treatment is being completed |
| 6410 Allergy management – Identifying know allergies (medication, food, insects, environmental) and the usual response – Notifying carers and healthcare workers of known allergies – Recording all allergies in the medical records, according to the protocol – Putting a medical alert bracelet on the patient, as appropriate – Observing whether the patient shows allergic reactions to new medications, formulas, food, latex and/or test colourings – Observing if there is a recurrence of anaphylaxis after 24h – Apply medication to reduce or minimise the allergic response | |
| 2300 Medication identification – Following the five rules for correctly administering medication – Assessing the patient to determine the response to the medication – Documenting the administration of the medication and the patient's response according to the centre's standards | |
| 00004 Risk of infection, associated with invasive procedures | 6610 Risk identification – Identifying biological, environmental and behavioural risks and well as how they interact |
| 6540 Infection control – Using antimicrobial soap to clean the hands, where necessary – Using sterile gloves, where necessary – Cleaning the patient's skin with the appropriate antibacterial agent – Maintaining an optimum antiseptic environment when inserting the main lines at the patient's bedside – Maintaining a closes system when conducting invasive haemodynamic monitoring – Changing the location of the peripheral and central I.V. Lines and the dressings, in line with the current CDC guidelines – Ensuring antiseptic handling of the I.V. lines – Administering antibiotic treatment where necessary | |
| 1876 Tube care: urinary – Keeping the hands clean before, during and after inserting or handling the catheter. – Cleaning the outside of the catheter at the meatus – Keeping the urinary catheter system permeable – Regularly cleaning the area of skin around it – Keeping the urinary drainage system closed, sterile and without obstructions. – Obtaining a urine sample through the opening of the closed urinary drainage system | |
| 3304 Handling mechanical ventilation: preventing pneumonia – Keeping the headboard at 30–45°, unless otherwise indicated (e.g. haemodynamic instability), especially during feeding through the enteral tube – Keeping the pressure in the endotracheal (ET) tube balloon at least 20cmH2O – Controlling the depth of the ET tube – Monitoring the effectiveness of mechanical ventilation on the patient's physical and psychological state – Monitoring whether patient is showing signs of respiratory infection (p. e.g. restlessness, coughing, fever, increased heart rate, change in secretions, leucocytosis, infiltrates on the thorax X-ray) – Cleaning the patient's teeth and tongue with antiseptic toothpaste or mouthwash, using circular movements with a soft toothbrush or a toothbrush with sucking action – Helping to apply a debriding agents or mouthwash to the gums, teeth and tongue with a swab, according to centre protocol – Using a Yankauer tube or soft suctioning for oral care, where necessary – Subglottic suctioning in patients that are lying down (bed, chair, road journey), relocating the ET tube deflating the balloon on the ET tube – suctioning on the trachea, oral cavity, and then the nasopharynx to remove secretions about the ET tube balloon in order to reduce the risk of inhalation – Keeping the straps on the ET tube clean and dry – Monitoring and recording oxygen saturation | |
| 4054 Handling the central venous access device – Following universal precautions – Following strict aseptic techniques to move the catheter, accessing it or using it to administer medication, in order to reduce blood infections associated with the catheter – Adapting care to the type of device (using transparent dressing to attach the non-tunnelled CVAD, medium line and PICC) – Changing the liquid infusion systems every 72h, the blood systems every 12h and the parenteral nutrition systems every 24h, or according to the centre's standards –Using new IV solutions and new infusion systems for new CVADs – Applying a transparent dressing according to the strict aseptic technique on a weekly basis or before if perforated, stained or detached – Applying a gauze dressing for the first 24h after the insertion procedure – Using transparent semipermeable dressing with non-tunnelled deceives and changing them every 7 days or before if they get wet, dirty or according to the centre's standards – Using 2% chlorhexidine in a 70% isopropyl alcohol solution to clean the wound and the catheter output every time the dressing is changed, and to decontaminate the skin before the CVAD is inserted, unless the patient is allergic to chlorhexidine – Decontaminating the CVAD with 2% chlorhexidine gluconate in a 70% isopropyl alcohol solution and leaving them to dry before use, unless otherwise stated by the manufacturer – Inspecting the entrance site on a daily basis checking for erythema, pain, sensitivity, heat or tumefaction since these devices are associated with a greater risk of infection. – Removing the device is there is an sign of inflation, escape or exudate at the entrance point | |
| 00203 Risk for ineffective renal perfusion, associated with systemic inflammatory response syndrome | 6680 Vital signs monitoring – Monitoring arterial pressure, pulse, temperature and respiratory condition where appropriate. – Observing trends and fluctuation in arterial pressure |
| 4200 Intravenous therapy – Checking the IV therapy order – Checking the five rules for correct administration before beginning infusion or administering medications (correct medication, dose, patient, via and frequency) – Administering IV medication according to prescription, and observing the results – Observing if there is hypervolemia or physical reactions – Recording intakes and losses as appropriate | |
| 0580 Urinary catheterisation – Connecting the urinary catheter to the drainage bag at the foot of the bed or the leg bag – Keeping the urinary draining system closed and without obstructions. – Monitoring input and output | |
| 4130 Fluids monitoring – Correcting mechanical problems (e.g. bent or blocked tube) in patients that have a sudden interruption in diuresis – Observing the colour, amount and weight of the urine – Consulting the doctor if the diuresis falls below 0.5ml/kg/h or the intake of fluids in an adult falls below 2000ml in 24h as appropriate – Administering medication to increase diuresis where necessary | |
| 00029 Fall in cardiac output, associated with a change in the afterload (drop in systemic vascular resistance), presenting as changes in arterial pressure and oliguria | 4210 Invasive haemodynamic monitoring – Helping with the insertion and removal of the invasive haemodynamic monitoring lines – Helping with the Allen to assess ulnar collateral circulation before radial arterial cannulation, if appropriate. – Set to zero and calibrate the equipment every 4–12h, where necessary, with the transducer at the level of the right atrium. – Monitoring arterial pressure (systolic, diastolic and average) – Monitoring haemodynamic waveforms to see if there is any change to cardiovascular function – Monitoring distal peripheral perfusion in the place where the catheter is inserted, every 4h, or as appropriate – Change sterile bandages and conduct care on the insertion area with the appropriate care. – Inspecting the insertion site in case of any haemorrhaging or infection – Administering medication to keep the haemodynamic parameters within the range specified |
| 1920 Acid-base monitoring – Obtaining samples of the acid-base balance for laboratory analysis (e.g. arterial blood gas levels, urine and serum,) – Observing if pH is within the average alkaline or acid range (7.35–7.45) – Observing if the PaCO2 indicate respiratory acidosis, respiratory alkalosis or normal situation – Observing if the HCO3 levels indicate metabolic acidosis, metabolic alkalosis or normal situation | |
| 2080 Fluid/electrolyte management – Observing if the electrolyte levels in the serum are abnormal, if this is available – Monitoring changes in the respiratory or cardiac situation they may indicate hypervolemia or dehydration – Administering fluid, if indicated – Irrigating nasogastric tubes with medical saline solution, according the centre's standards and as indicated – Maintaining the correct IV infusion blood transfusion or enteral rate – Precisely recording input and output – Observing if there are any signs of water retention | |
| 4256 Shock management: vasogenic – Checking ECG – Administering atropine for badycardia, where appropriate – Administering bolus of isotonic crystalloids, keeping systolic pressure at 90mmHg or above, where appropriate. – Administering antihistamines and/or corticosteroids, where appropriate – Administering vasopressors – Checking body temperature – Administering anti-inflammatory medication, where appropriate | |
| 1876 Urinary catheter care – Observing the characteristics of the drained fluid – Observing there is vesical distension | |
| 6412 Anaphylaxis management – Identifying and eliminating the cause of the allergen if possible – Monitoring vital signs – Observing if there are signs of shock (e.g. difficulty berating, cardiac arrhythmias, epileptic seizures and low blood pressure) – Administering IV fluids quickly (1000ml/h) to support arterial pressure, according to medical prescription or protocol – Administering spasmolytic, antihistamines or corticosteroids, as indicated, and documenting if there is a rash, angioedema or bronchospasm – Observing with the anaphylaxis goes down after 24h | |
| 7690 Laboratory data interpretation – Monitoring the results from the analysis to check on trends and noticeable changes | |
| 00033 Impaired spontaneous ventilation, associated with metabolic factors (angioedema), presents as less cooperation | 3120 Airway insertion and stabilisation – Selecting the right size and type for the oropharynx or nasopharynx airway – Observing if there is dyspnoea, snoring or breathing noises when the oro/nasopharynx airway is attached. – Helping with the TE insertion connection the intubation and emergency equipment where necessary, positioning the patient, administering the prescribed medication and checking if the patient in case of complications during insertion – Hyperoxygenating the patient with 100% oxygen 3–5min, as appropriate – Sounding the thorax after intubation – Observing the systematic movement of the thorax wall – Monitoring oxygen saturation (SpO2) using non-invasive pulse oximetry – Checking the placement of the tube with a thorax X-ray, checking that the cannulation of the trachea is 2–4cm above the carina |
| 2260 Sedation management – Checking if there are allergies to medication – Observing if there are adverse effects as a result of medication, such as agitation, respiratory depression, low blood pressure, drowsiness, hypoxaemia arrhythmia, apnoea or exacerbation of an existing condition | |
| 3180 Handling the artificial airways – Going through universal precautions – Maintaining the balloon on the endotracheal tube/tracheostomy cannula at 15–20mmHg during mechanical ventilation and feeding – Checking the pressure in the balloon every 4–8h during exhalation, using a three way stopcock, calibrated syringe and a pressure gauge. – Carrying out endotracheal suctioning, where necessary – Suctioning the oropharynx and the secretions in the upper part of the tube before deflating the device – Checking the colour, amount and consistency of the secretions – Carrying out oral care – Putting measures into place to prevent accidental detubation: fixing the airway with straps/tape, administering sedatives and muscular relaxants, and attaching it to the arms, as necessary. | |
| 3300 Mechanical ventilation management: invasive – Ensure that the ventilator alarms are connected – Administering muscle relaxants, sedatives and narcotic painkillers, as appropriate – Checking the pressure screen on the ventilator, patient/ventilator synchronism and the patient's vesicular murmur – Suctioning, if there are adventitious breath sounds and/or increase in respiratory pressure – Checking the colour, amount and consistency of the pulmonary secretions, and periodically documenting the results | |
| 3160 Suctioning the artificial airways – Determining the need for oral and/or tracheal suctioning – Hyperoxygenating with 100% oxygen, for at least 30s using the ventilator or manual resuscitation bag before and after each turn. – Using the disposable sterile equipment for each tracheal suctioning procedure – Selecting a suctioning tube that is half the size of the endotracheal tube, tracheostomy cannula or patient's airway. – Leaving the patient connected during suctioning, if a closed tracheal suctioning system or oxygen insufflation device is used – Using the minimum amount of suctioning, when a wall suction unit is used to remove secretions (80–120mmHg for adults) – Checking and observing the colour, amount and consistency of the secretions – Sending the secretions for cultivation and antibiogram, where appropriate | |
| 3310 Mechanical ventilator weaning – Putting the patient in the best position to use their respiratory muscles and optimise the lowering of the diaphragm – Suctioning the airway, where necessary – Alternating test weaning periods with enough rest and sleep period – Observing if there are signs of respiratory muscle fatigue (sudden rise in PaCO2, rapid and superficial ventilation and paradoxical movement of the abdominal wall), tissue hypoxaemia and hypoxia when weaning – Avoiding sedation with medication during the weaning tests, as necessary – Remaining with the patient and providing support during the initial weaning tests – Checking factors that indicate tolerance to weaning, according to centre protocol (e.g. level of short circuit, vital capacity, Vd/Vt, VVM, inspiratory force, VEMS, negative inspiratory pressure) – Starting the weaning with testing periods (e.g. 30–120min of spontaneous breathing with help from the breathing machine) | |
| 3270 Endotracheal extubation – Positioning the patient to get maximum use of their respiratory muscles, normally with the head of the bed at 75° – Instructing the patient about the procedure – Hyperoxygenating the patient and suctioning the endotracheal airways – Suctioning the oral airways – Deflating the endotracheal balloon and removing the endotracheal tube – Encouraging the patient to cough and expectorate – Administering oxygen, according to prescription – Stimulating coughing and deep breathing – Observing if there is an obstruction in the airway – Checking ability to swallow and talk | |
| 00179 Risk of unstable blood sugar levels, associated with low levels of physical health | 2120 Hyperglycaemia management – Checking blood sugar levels if indicated – Identifying possible causes of hyperglycaemia – Administering insulin according to prescription |
| 7610 Bedside laboratory testing – Following institutional procedures for collecting and conserving sample, as applicable – Recording the results of the analysis, according to the centre's procedures – Providing information about critical or abnormal results to the doctor, as applicable | |
| 4035 Capillary blood sample – Manually pricking the skin with a blood lancet or an approved pricking mechanism according to the manufacturer's instructions – Removing the first drop of blood with dry gauze according to the manufacturer's instructions or protocol at the centre | |
| 00197 Risk of dysfunctional gastrointestinal motility, associated with medications, immobility and infection | 1100 Nutrition management – Identifying food allergies or intolerance in the patient – Determining the number of calories and the type of nutrient necessary to meet their nutritional needs – Monitoring weight loss and gain trends |
| 1874 Tube care: gastrointestinal – Listening to intestinal sounds regularly – Attaching the tube to the relevant body part, bearing in mind comfort and the patient's skin – Staring and monitoring the feeding supply through the enteral tube, as applicable, following protocol at the centre – Monitoring the volume, colour and consistency of the nasogastric drainage. | |
| 1056 Enteral tube feeding – Inserting the nasogastric, nasoduodenal or nasojejunal tube according to protocol at the centre – Observing whether the tube is correct, inspecting the oral cavity, checking for gastric waste and listening during the injection and extraction of air, according to protocol at the centre – Raising the head of the bed by 30 to 45° during feeding – Irrigating the tube every 4–6h during continuous feeding and after each intermittent feeding – Checking for residue every 4–6h for the first 24h and afterwards every 8h during continuous feeding – Observing if there is intestinal noise every 4-8h, as necessary | |
| 0430 Bowel management – Recording the date of the last elimination – Monitoring eliminations, including frequency, consistency, form, volume and colour, where applicable – Monitoring the signs and symptoms of diarrhoea, constipation and impaction – Assessing the medication profile to determine secondary gastrointestinal effects | |
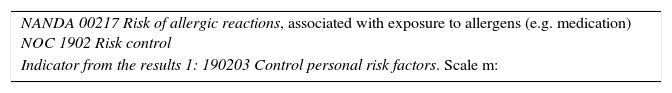
Relationship between NANDA, NOC and indicators in the results.
| NANDA 00217 Risk of allergic reactions, associated with exposure to allergens (e.g. medication) NOC 1902 Risk control |
| Indicator from the results 1: 190203 Control personal risk factors. Scale m: |
| Not shown | Rarely shown | Sometimes shown | Frequently shown | Always shown |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| Indicators from results 2: 190204 Develop effective risk control strategies. Scale m: | ||||
| Not shown | Rarely shown | Sometimes shown | Frequently shown | Always shown |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| NANDA 00004 Risk of infection, associated with invasive procedures NOC 0703 Severity of the infection | ||||
| Indicator from results: 070304 Purulent sputum. Scale n: | ||||
| Severe | Substantial | Moderate | Mild | None |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| NANDA 00203 Risk for ineffective renal perfusion, associated with systemic inflammatory response syndrome (SIRS) NOC 0404 Tissue perfusion: abdominal organs | ||||
| Indicators from results 1: 40402 Diuresis. Scale b: | ||||
| Severe deviation from the normal range | Substantial deviation from the normal range | Moderate deviation from the normal range | Mild deviation from the normal range | No deviation from the normal range |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| Indicators from results 2: 40420 Blood keratinise levels. Scale b: | ||||
| Severe deviation from the normal range | Substantial deviation from the normal range | Moderate deviation from the normal range | Mild deviation from the normal range | No deviation from the normal range |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| NANDA 00029 Fall in cardiac output, associated with a change in the afterload (drop in systemic vascular resistance), presenting as changes in arterial pressure and oliguria. NOC 0400 Effectiveness of the heart pump | ||||
| Indicators from results 1: 40001 Systolic blood pressure Scale b: | ||||
| Severe deviation from the normal range | Substantial deviation from the normal range | Moderate deviation from the normal range | Mild deviation from the normal range | No deviation from the normal range |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| Indicators from results 2: 40020 Urine output. Scale b: | ||||
| Severe deviation from the normal range | Substantial deviation from the normal range | Moderate deviation from the normal range | Mild deviation from the normal range | No deviation from the normal range |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| NANDA 00033 Impaired spontaneous ventilation, associated with metabolic factors (angioedema), presents as less cooperation NOC 0402 Respiratory condition: gas exchange | ||||
| Indicators from results 1: 40208 Partial oxygen pressure in arterial blood (PaO2). Scale b: | ||||
| Severe deviation from the normal range | Substantial deviation from the normal range | Moderate deviation from the normal range | Mild deviation from the normal range | No deviation from the normal range |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| Indicator from the results 2: 40209 Partial carbon dioxide pressure in the arterial blood (PaCO2) Scale b: | ||||
| Severe deviation from the normal range | Substantial deviation from the normal range | Moderate deviation from the normal range | Mild deviation from the normal range | No deviation from the normal range |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| Indicator from the results 3: 40210 Arterial pH. Scale b: | ||||
| Severe deviation from the normal range | Substantial deviation from the normal range | Moderate deviation from the normal range | Mild deviation from the normal range | No deviation from the normal range |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| NANDA 00179 Risk of unstable blood sugar levels, associated with low levels of physical health NOC 2300 Blood glucose level | ||||
| Indicator from results: 230001 Blood glucose concentration. Scale b: | ||||
| Severe deviation from the normal range | Substantial deviation from the normal range | Moderate deviation from the normal range | Mild deviation from the normal range | No deviation from the normal range |
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 |
| NANDA 00197 Risk of dysfunctional gastrointestinal motility, associated with medication, immobility and infection NOC 1015 Gastrointestinal functioning | ||||
| Indicators from results 1: 101501 Tolerance to food. Scale a: | ||||
| Severely compromised | Substantially compromised | Moderately compromised | Mildly compromised |
|---|---|---|---|
| 1 | 2 | 3 | 4 |
| Indicators from results 2: 101503 Frequency of excretions. Scale a: | |||
| Severely compromised | Substantially compromised | Moderately compromised | Mildly compromised |
|---|---|---|---|
| 1 | 2 | 3 | 4 |
The diagnosis of systemic anaphylaxis is based on identifying the specific symptoms (obstruction in the airway, low blood pressure, gastrointestinal symptoms and generalised skin reaction), either isolated or in combination, after exposure to a substance that may cause immediate hypersensitivity and that are caused by the release of chemical mediators from mastocytes to basophils, after interaction between specific IgE antibodies.8
In this case, it can be seen that, with the medical history of angioedema, a study of the patient's allergies may not have been complete, since a potential sensitivity to amoxicillin had not been studied, among other medications, and especially when it is known that allergic reactions to beta-lactam antibiotics are a frequent cause of allergic reaction to medication, through a specific immunological response.3
The care plan presented is intended as a tool for use and streamlined managing, to allow nursing professionals to standardise their actions with patients suffering from anaphylactic shock on the ICU, to be subsequently assessed based on the criteria established in the plan. Furthermore, it is intended to homogenise interventions to reduce variation in how care is provided, increasing safety and the quality of care, as argued by Cuzco and Guasch.10 After reviewing the currently available literature, no similar studies have been found with which to contrast our nursing diagnostics. The indicators in the results from our care plan indicated an improvement, which means they could be taken as a reference point for future research.
Among the main limitations, it should be pointed out that it was impossible to come to a consensus on the aims of nursing actions with sedated patients. The study also did not have serialised information on the histamine and tryptase levels in the plasma to assess the severity and the development of the anaphylactic condition, as some authors recommend.1,5,6 Cardona1 emphasises the importance of health-care training. We should emphasis the important role that nursing professionals play in getting patients to take on board the relevant self-care actions in each case, and in avoiding situations such as adrenaline self-injectors going out-of-date with patients with a history of angioedema.
ConclusionsThe results criteria showed a positive development after 24h. The development of the standard NANDA-NOC-NIC terminology in a clinical case study allowed us to methodologically organise nursing work, providing records and standardising practice.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments have been carried out on human beings or on animals for this research.
Confidentiality of dataThe authors state that they have followed the protocol of their work centre regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or individuals referred to in this article. This document is held by the author in charge of correspondence.
To draw up the plan, we reviewed the online platform NNNConsult.9
Please cite this article as: Zariquiey-Esteva G, Santa-Candela P. A propósito de un caso: intervenciones enfermeras a una paciente con shock anafiláctico en la UCI. Enferm Intensiva. 2017;28:80–91.