Weaning from invasive mechanical ventilation (IMV) is influenced by physiological and psychological factors, the latter being the least studied. The aim was to identify, through the literature, patients’ experiences during weaning from IMV and report its influencing factors.
MethodThe literature search was conducted using the Pubmed, CINAHL and PsycINFO databases. The search terms were: “patient”, “experience” and “ventilator weaning”. The research limits were: age (>19years) and language (English, Spanish and Finnish).
ResultsFifteen publications were analyzed. The main results were grouped into three main categories according to patient's perceptions, feelings and experiences, influence of professionals’ attention and determinants for successful weaning. Patients remember IMV weaning as a stressful process where they experience anxiety, frustration, despair or uncertainty. Nurses have a key role in improving communication with patients and foreseeing their needs. Family support and the care provided by the caregivers were shown as essential during the process. The patient's self-determination, self-motivation and confidence are identified as important factors to achieve successful IMV weaning.
ConclusionsPsychological care, in addition to physical and technical care, is important at providing holistic care. Interventional studies are needed to improve the care during the weaning experience.
La retirada de la ventilación mecánica invasiva (VMI) es un procedimiento en el que influyen factores fisiológicos y psicológicos, siendo estos últimos los menos estudiados. El objetivo fue identificar en la literatura, las experiencias de los pacientes durante la retirada de la VMI y cómo intervienen en dicho proceso.
MétodoSe realizó una búsqueda bibliográfica en las bases de datos Pubmed, CINAHL y PsycINFO. Los términos de búsqueda fueron: «patient», «experience» y «ventilator weaning». Los límites fueron la edad (>19años) y el idioma (inglés, español y finlandés).
ResultadosSe analizaron 15 publicaciones. Los principales resultados se agruparon en tres grandes temas según las percepciones, sentimientos y experiencias del paciente, la influencia de la atención de los profesionales y los factores determinantes para la retirada exitosa de la VMI. Los pacientes recuerdan la retirada de la VMI como un proceso estresante y experimentan ansiedad, frustración, desesperación o incertidumbre. Las enfermeras tienen un papel fundamental en la mejora de la comunicación con el paciente y en la anticipación a sus necesidades. El soporte familiar y el cuidado proporcionado por los profesionales se destacan como fundamentales durante el proceso. Para conseguir una retirada exitosa de la VMI se identifica la importancia de la autodeterminación, la automotivación y la confianza de los pacientes.
ConclusionesLa atención psicológica, además de la física y la tecnológica, es importante durante la retirada de la VMI para proporcionar un cuidado holístico. Son necesarios estudios de intervención para lograr mejorar la atención a los pacientes durante dicho proceso.
According to the Weaning Continuum Model of the AACCN, the results of the process of withdrawing the invasive mechanical ventilation is directly related to the emotional sphere and changes in the patient's mood. Through this paper we intend to know the psychological repercussion that the weaning process has on the patient. This will make us aware of its importance, reflect on the role of the nurse, and determine the specific strategies to respond to the needs of the patient that will favour holistic assessment and care.
IntroductionInvasive mechanical ventilation (IMV) is frequently provided to patients in the intensive care units (ICUs). It is a technological breakthrough that provides ventilatory support in life-threatening situations of respiratory failure. However, the disconnection process of IMV, through which the patient regains his/her spontaneous and effective ventilation (also known as weaning), is a complex process and is influenced by the patient's physiological and psychological factors, the latter being the least studied.1
The Weaning Continuum Model (WCM) of the American Association of Critical Care Nurses (AACCN)2,3 poses weaning as a continuous and dynamic process influenced by physiological (myocardial function and oxygenation, ventilatory muscles, nutritional status), psychological and environmental variables. These aspects combined lead to three possible outcomes: complete weaning, partial incomplete weaning and total incomplete weaning. The nursing professional plays a key role in the success of this process. The nurse must know the patient and, as Benner et al.4 confirmed, must be the coach and promote collaboration and interaction (nurse-patient) to facilitate weaning.
In this sense, several authors5–10 affirm that when patients face the process of IMV withdrawal, they experience feelings of uncertainty, dependence, fear and frustration, etc. And these feelings influence directly on the success or failure of weaning. For example, the fact that the patient experiences dyspnoea during this process favours the onset of anxiety and makes weaning difficult.11 Also, feeling that they lack the strength to be able to communicate or to hold objects with their hands causes them vulnerability and feelings of weakness.1,12
By contrast, other authors show that the nursing care provided to the patient during weaning5,12–14 and the information and care that is provided to the family members1,7 is a positive influence, which plays a crucial role in reducing the intensity of these adverse experiences.12
Similarly, the nurses’ knowledge about the experiences of the patients during weaning can offer a holistic and personalized care.1 On numerous occasions, the patients view withdrawing from the IMV as very negative.15–17 For this reason, the nursing professional requires training and an expert knowledge that will provide him/her with the skills and competences7,15,17 to be able to help the patients to participate in decision-making. In addition, it adds confidence and a suitable environment that reduces anxiety and fatigue, and maximizes the chances of the weaning success.7,18 On the other hand, the emotional repercussion in the patients influences, in turn, their perception of their caregivers.1,5,11,13–16 Hence, the high prevalence of negative experiences experienced by patients during this process urges nursing professionals to reflect on the daily praxis and to determine the specific strategies to respond to the patient's needs to achieve health and autonomy.
For all of the above, this paper aims to identify the experiences of patients during the process of IMV withdrawal and to indicate how these experiences intervene in this process, as published in literature, in order to be able to introduce improvements in this practice that allow quality care to be provided to these patients.
MethodA review of the literature with a narrative approach is conducted herein. As Dixon-Woods et al. indicates,19 this approach is flexible and allows different types of evidence to be reviewed (qualitative and quantitative). It has an extensive nature where a writing style is used that allows a clear picture of the study subject to be demonstrated. It also focuses on gathering the relevant information that provides the context and the essence of the topic of interest.19
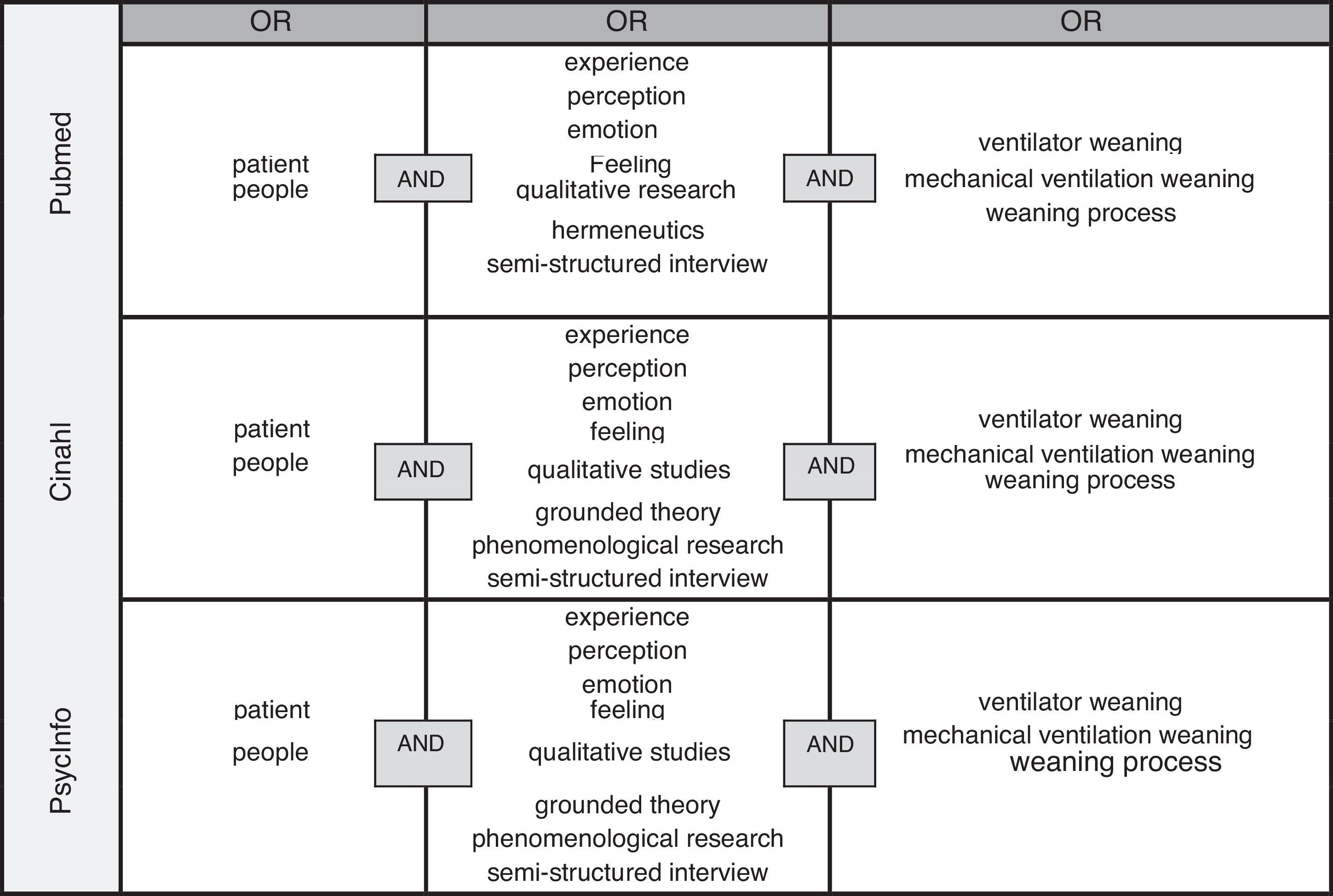
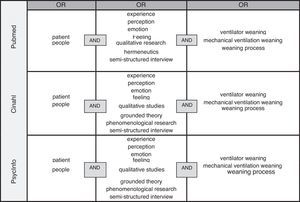
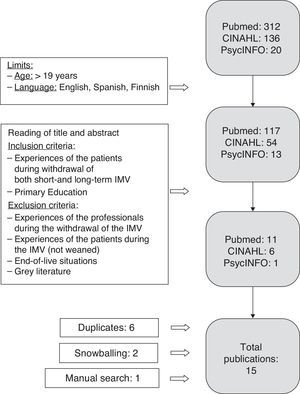
Search strategyA literature search was carried out between October 2014 and January 2015 in the Pubmed, CINAHL and PsycINFO databases. The terms included in the search were: “patient”, “experience” and “ventilator weaning”. The search strategy was established by combining these terms and their corresponding synonyms with the Boolean operators OR and AND, as detailed in Fig. 1.
Also, the limits established in the search were the age (>19years) and the language (Spanish, English and Finnish). In addition, to discard relevant articles, a manual search was conducted in nursing journals such as Dimensions of Critical Care Nursing Journal, Critical Care Nurse, American Journal of Critical Care and Enfermería Intensiva. Finally, through the snowballing method, the reference lists of the main articles (included in the review) were reviewed to corroborate whether there were any additional relevant studies.
We included all the primary studies that referred to the experiences of patients during IMV withdrawal, both short (between 24 and 72h) and long duration (more than 72h).3
We excluded the publications that focused on the experiences of the professionals, on the experiences of patients during IMV that did not refer to weaning, to end-of-life situations and to grey literature (conferences, unpublished reports, theses or dissertations).
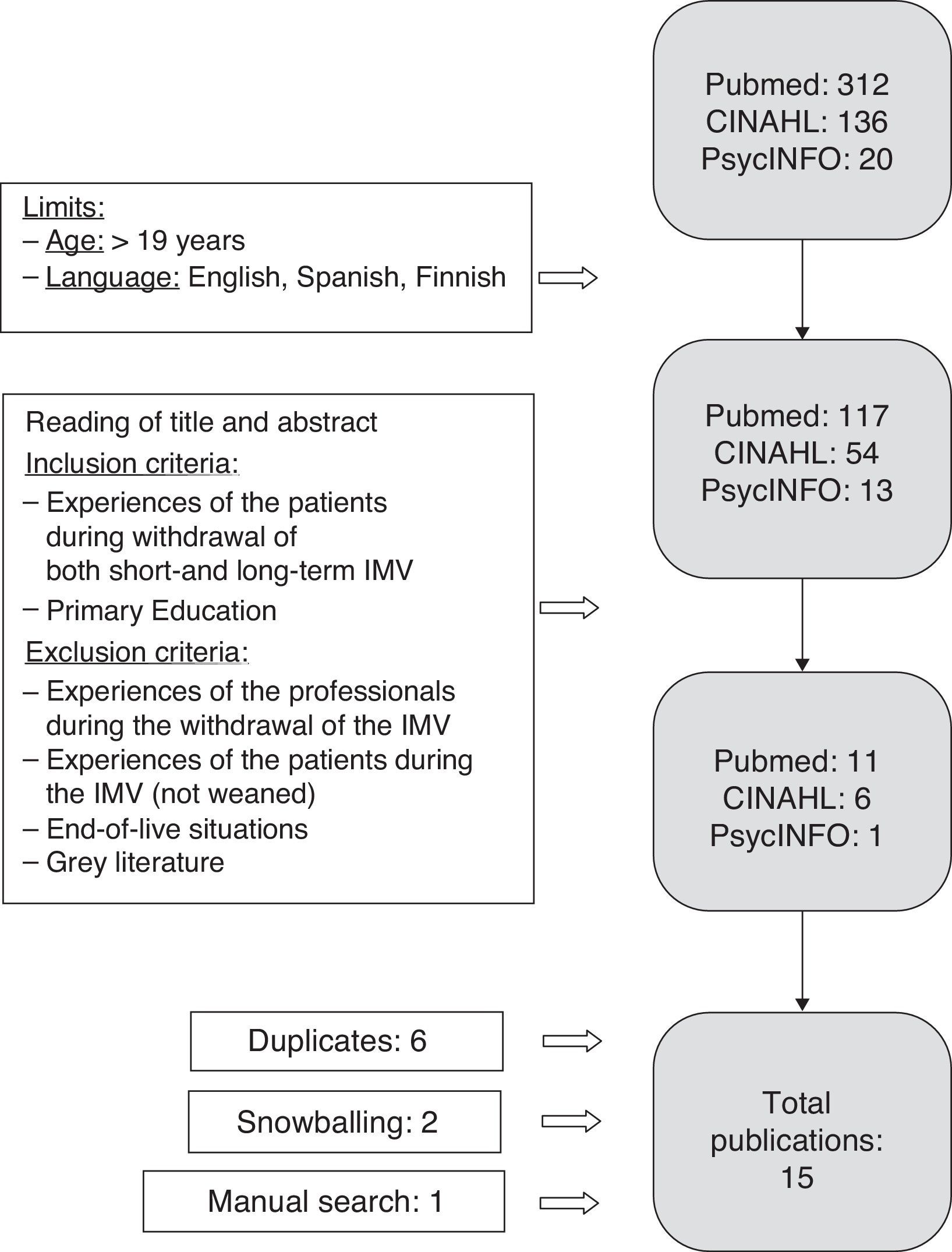
The result of the search is displayed in Fig. 2.
Synthesis of the resultsAfter reading the selected articles in depth, identifying the aspects that responded to the objective, determining the important or recurrent themes in the publications and classifying the articles in the arising thematic lines, a synthesis of the content was made.
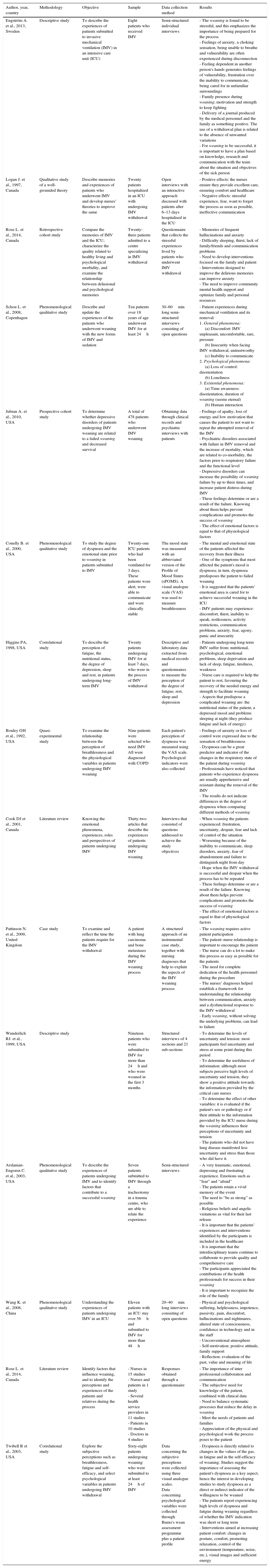
ResultsFifteen publications were analyzed (Table 1) which responded to the objective of the review. The most important findings from the literature were classified into three main themes:
Summary of the selected publications.
| Author, year, country | Methodology | Objective | Sample | Data collection method | Results |
|---|---|---|---|---|---|
| Engström A. et al., 2013, Sweden | Descriptive study | To describe the experiences of patients submitted to invasive mechanical ventilation (IMV) in an intensive care unit (ICU) | Eight patients who received IMV | Semi-structured individual interviews | - The weaning is found to be stressful, and this emphasizes the importance of being prepared for the process - Feelings of anxiety, a choking sensation, being unable to breathe and vulnerability are often experienced during disconnection - Feeling dependent in another person's hands generates feelings of vulnerability, frustration over the inability to communicate, being cared for in unfamiliar surroundings - Family presence during weaning; motivation and strength to keep fighting - Delivery of a journal produced by the medical personnel and the family as something positive. The use of a withdrawal plan is related to the absence of unwanted variations - For weaning to be successful, it is important to have a plan based on knowledge, research and communication with the team about the situation and objectives of the sick person |
| Logan J. et al., 1997, Canada | Qualitative study of a well-grounded theory | Describe memories and experiences of patients who underwent IMV and develop nurses’ theories to improve the same | Twenty patients hospitalised in an ICU with undergoing IMV withdrawal | Open interviews with an interactive approach discussed with patients after 6–13 days hospitalised in the ICU | - Positive effects: the nurses ensure they provide excellent care, ensuring comfort and healthcare - Negative effects: stressful experience, fear, want to forget the process as soon as possible, ineffective communication |
| Rose L. et al., 2014, Canada | Retrospective cohort study | Compare the memories of IMV and the ICU; characterize the quality related to healthy living and psychological morbidity, and examine the relationship between delusional and psychological memories | Twenty-three patients admitted to a centre specializing in IMV withdrawal | Questionnaire that collects the stressful experiences lived by patients who underwent IMV withdrawal | - Memories of frequent hallucinations and anxiety - Difficulty sleeping, thirst, lack of family/friends and communication problems - Need to develop interventions focused on the family and patient - Interventions designed to improve the delirious memories can improve anxiety - The need to improve community mental health support and optimize family and personal resources |
| Schou L. et al., 2008, Copenhagen | Phenomenological qualitative study | Describe and update the experiences of the patients who underwent weaning with the new forms of IMV and sedation | Ten patients over 18 years of age underwent IMV for at least 24h | 30–60min long semi-structured interviews consisting of open questions | - Patient experiences during mechanical ventilation and its removal: 1. General phenomena: (a) Discomfort: IMV unpleasant, uncomfortable, rare, pressure (b) Insecurity when facing IMV withdrawal, untrustworthy (c) Inability to communicate 2. Psychological phenomena: (a) Loss of control: disorientation (b) Loneliness 3. Existential phenomena: (a) Time awareness: disorientation, duration of weaning (seems eternal) (b) Human interaction |
| Jubran A. et al., 2010, USA | Prospective cohort study | To determine whether depressive disorders of patients undergoing IMV weaning are related to a failed weaning and decreased survival | A total of 478 patients who underwent IMV weaning | Obtaining data through clinical records and psychiatric interviews with patients | - Feelings of apathy, loss of energy and low motivation that causes the patient to not want to repeat the attempted removal of the IMV - Psychiatric disorders associated with failure in IMV removal and the increase of mortality, which are related to co-morbidity, the factors prior to respiratory failure and the functional level - Depressive disorders can increase the possibility of weaning failure by up to three times, and increase patient distress during IMV - These feelings determine or are a result of the failure. Knowing about them helps prevent complications and promotes the success of weaning - The effect of emotional factors is equal to that of physiological factors |
| Conelly B. et al., 2000, USA | Phenomenological qualitative study | To study the degree of dyspnoea and the emotional state prior to weaning in patients submitted to IMV | Twenty-one ICU patients who had been ventilated for 3 days. These patients were alert, were able to communicate and were clinically stable | The mood state was measured with an abbreviated version of the Profile of Mood States (sPOMS). A visual analogue scale (VAS) was used to measure breathlessness | - The mental and emotional state of the patients affected the recovery from their illness - One of the symptoms that most affected the patient's mood is dyspnoea; in turn, dyspnoea predisposes the patient to failed weaning - It is suggested that the patients’ emotional area is cared for to achieve successful weaning in the ICU - IMV patients may experience: discomfort, thirst, inability to speak, restlessness, activity restrictions, communication problems, anxiety, fear, agony, panic and insecurity |
| Higgins PA, 1998, USA | Correlational study | To describe the perception of fatigue, the nutritional status, the degree of depression, sleep and rest, in patients undergoing long-term IMV | Twenty patients undergoing IMV for at least 7 days, who were in the process of IMV withdrawal | Descriptive and laboratory data extracted from medical records and questionnaires to measure the perception of the degree of fatigue, rest, sleep and depression | - Patients undergoing long-term IMV suffer from: nutritional, psychological, emotional problems, sleep deprivation and lack of sleep, fatigue, tiredness, weakness - Nurse care is required to help the patient to rest, favouring the recovery of the needed energy and strength to facilitate weaning - Aspects that predispose a complicated weaning are: the nutritional status of the patient, a depressed mood and problems sleeping at night (they produce fatigue and lack of energy) |
| Bouley GH et al., 1992, USA | Quasi-experimental study | To examine the relationship between the perception of breathlessness and the physiological variables in patients undergoing IMV weaning | Nine patients were selected who need IMV All were diagnosed with COPD | Each patient's perception of dyspnoea was measured using the VAS scale. Psychological indicators were also collected | - Feelings of anxiety or loss of control were expressed due to the sensation of breathlessness - Dyspnoea can be a great predictor and indicator of the changes in the respiratory state of the patient during weaning - Professionals have noticed that patients who experience dyspnoea are usually apprehensive and resistant during the removal of the IMV - The results do not indicate differences in the degree of dyspnoea when comparing different methods of weaning |
| Cook DJ et al., 2001, Canada | Literature review | Knowing the emotional phenomena, experiences, roles and perspectives of patients undergoing IMV | Thirty-two articles that describe the experiences of patients undergoing IMV weaning | Interviews that consisted of questions addressed to achieve the study objectives | - When weaning the patients experienced: frustration, uncertainty, despair, fear and lack of control of the situation - Worsening because of the inability to communicate, sleep disorders, anxiety, fear of abandonment and failure to distinguish night from day - Hope when the IMV withdrawal is successful and despair when the process has to be repeated - These feelings determine or are a result of the failure. Knowing about them helps prevent complications and promotes the success of weaning - The effect of emotional factors is equal to that of physiological factors |
| Pattinson N. et al., 2009, United Kingdom | Case study | To examine and reflect the time the patients require for the IMV withdrawal | A patient with lung carcinoma and bone metastases during the IMV weaning process | A structured approach of an instrumental case study, together with nursing diagnoses that help to explain the aspects of the IMV weaning process | - The weaning requires active patient participation - The patient–nurse relationship is important to encourage the patient - The nurse can do a lot to make this process as easy as possible for the patients - The need for complete dedication of the health personnel during the procedure - The nurses’ diagnoses helped establish a framework for understanding the relationship between communication, anxiety and a dysfunctional response to the IMV withdrawal - Early weaning, without solving the underlying problems, can lead to failure |
| Wunderlich RJ. et al., 1999, USA | Descriptive study | Nineteen patients who were submitted to IMV for more than 24h and who were weaned in the first 3 months | Structured interviews of 4 sections and 21 sub-sections | - To determine the levels of uncertainty and tension: most participants feel uncertainty and stress at some point during this period - To determine the usefulness of information: although most subjects perceive high levels of uncertainty and tension, they show a positive attitude towards the information provided by the critical care nurses - To determine the effect of other variables: it is evaluated if the patient's sex or pathology or if their attitude to the information provided by the ICU nurse during the weaning influences their perceptions of uncertainty and tension - The patients who did not have lung disease manifested less uncertainty and stress than those who did have it. | |
| Arslanian-Engoren C. et al., 2003, USA | Phenomenological qualitative study | To describe the experiences of patients undergoing IMV and to identify factors that contribute to a successful weaning | Seven patients submitted to IMV through a tracheotomy in a trauma centre, who are able to relate the experience | Semi-structured interviews | - A very traumatic, emotional, depressing and frustrating experience. Emotions such as “fear” and “afraid” - The patients retain a vivid memory of the event - The need to “be as strong” as possible - Religious beliefs and angelic visitations as vital for their last release - It is important that the patients’ experiences and interventions identified by the participants is included in the healthcare - It is important that the interdisciplinary teams continue to collaborate to provide quality and comprehensive care - The participants appreciated the contributions of the health professionals for success in their weaning - It is important to recognize the role of the family |
| Wang K. et al., 2008, China | Phenomenological qualitative study | Understanding the experiences of patients undergoing IMV in an ICU | Eleven patients with an ICU stay over 56h and submitted to IMV for more than 48h | 20–40min long interviews consisting of open questions | - Physical and psychological suffering, helplessness, impotence, passivity, pain, discomfort, hallucinations and nightmares, altered state of consciousness, confidence in technology and in the staff - Unconventional atmosphere - Self-motivation: positive attitude, family support - Reflection: evaluation of the past, value and meaning of life |
| Rose L. et al., 2014, Canada | Literature review | Identify factors that influence weaning, and to identify the perceptions and experiences of the patients and relatives during the process | - Nurses in 15 studies - Nurses and patients in 1 study - Several health service providers in 11 studies - Patients in 10 studies - Doctors in 4 studies | Responses obtained through a questionnaire | - The importance of inter professional collaboration and communication - The subjective need for knowledge of the patient, combined with clinical data - Need to balance systematic processes that reduce the delay in weaning - Meet the needs of patients and families - Appreciation of the physical and psychological work the process poses to the patient |
| Twibell R et al., 2003, USA | Correlational study | Explore the subjective perceptions such as breathlessness, fatigue and self-efficacy, and select psychological variables in patients undergoing IMV withdrawal | Sixty-eight patients undergoing weaning who were submitted to at least 24h of IMV | Data concerning the subjective perceptions were collected using three visual analogue scales. Data concerning psychological variables were collected through Burns's wean assessment programme plus a patient profile | - Dyspnoea is directly related to changes in the values of the gas, in fatigue and in the self-efficacy of weaning. Studies suggest the importance of assessing the patient's dyspnoea as a key aspect, hence the interest in developing studies to study dyspnoea as a direct or indirect indicator of the willingness to be weaned - The patients report experiencing high levels of dyspnoea and fatigue during weaning regardless of whether the IMV indication was short or long term - Interventions aimed at increasing patient comfort: changes in posture, comfort, promoting relaxation, control of the environment (temperature, noise, etc.), visual images and sufficient energy |
- •
Perceptions, feelings and experiences of the patient during IMV withdrawal.
- •
The influence of care professionals during weaning.
- •
The determining factors for successful IMV withdrawal.
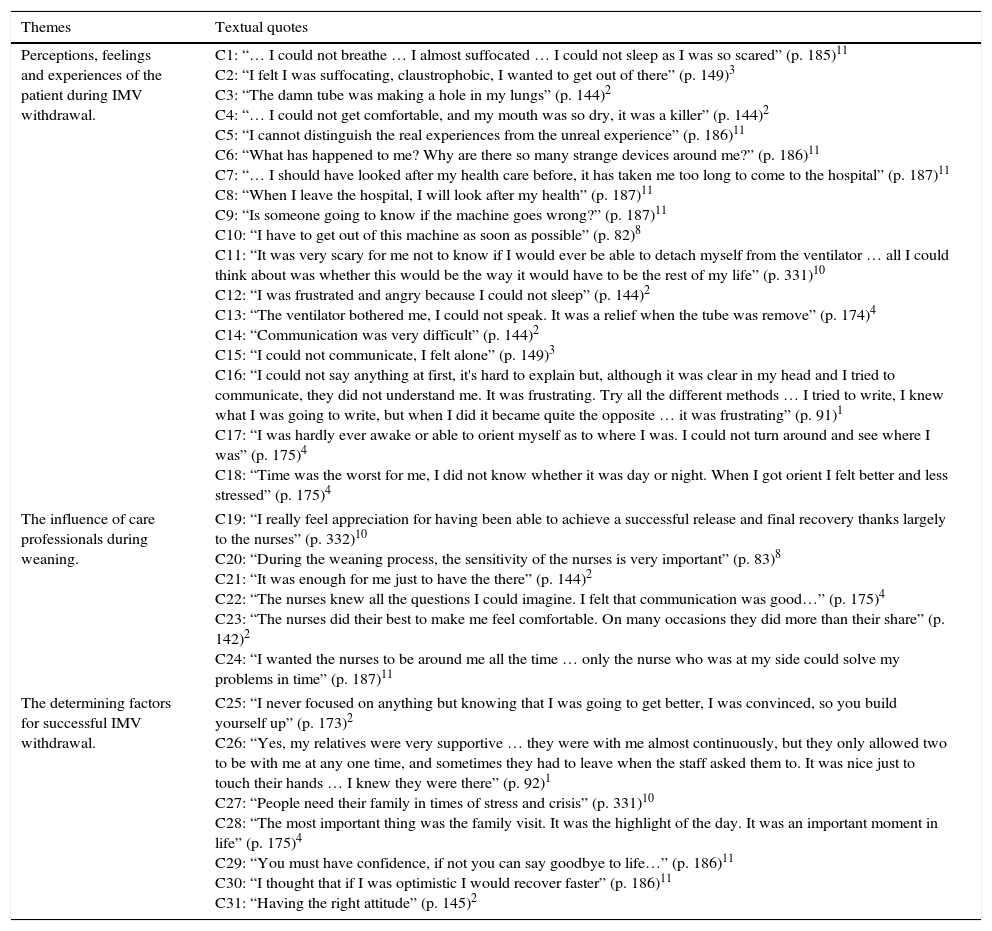
In addition, quotations from qualitative studies included in the review were added Table 2 which can illustrate the results.
Examples of quotations.
| Themes | Textual quotes |
|---|---|
| Perceptions, feelings and experiences of the patient during IMV withdrawal. | C1: “… I could not breathe … I almost suffocated … I could not sleep as I was so scared” (p. 185)11 C2: “I felt I was suffocating, claustrophobic, I wanted to get out of there” (p. 149)3 C3: “The damn tube was making a hole in my lungs” (p. 144)2 C4: “… I could not get comfortable, and my mouth was so dry, it was a killer” (p. 144)2 C5: “I cannot distinguish the real experiences from the unreal experience” (p. 186)11 C6: “What has happened to me? Why are there so many strange devices around me?” (p. 186)11 C7: “… I should have looked after my health care before, it has taken me too long to come to the hospital” (p. 187)11 C8: “When I leave the hospital, I will look after my health” (p. 187)11 C9: “Is someone going to know if the machine goes wrong?” (p. 187)11 C10: “I have to get out of this machine as soon as possible” (p. 82)8 C11: “It was very scary for me not to know if I would ever be able to detach myself from the ventilator … all I could think about was whether this would be the way it would have to be the rest of my life” (p. 331)10 C12: “I was frustrated and angry because I could not sleep” (p. 144)2 C13: “The ventilator bothered me, I could not speak. It was a relief when the tube was remove” (p. 174)4 C14: “Communication was very difficult” (p. 144)2 C15: “I could not communicate, I felt alone” (p. 149)3 C16: “I could not say anything at first, it's hard to explain but, although it was clear in my head and I tried to communicate, they did not understand me. It was frustrating. Try all the different methods … I tried to write, I knew what I was going to write, but when I did it became quite the opposite … it was frustrating” (p. 91)1 C17: “I was hardly ever awake or able to orient myself as to where I was. I could not turn around and see where I was” (p. 175)4 C18: “Time was the worst for me, I did not know whether it was day or night. When I got orient I felt better and less stressed” (p. 175)4 |
| The influence of care professionals during weaning. | C19: “I really feel appreciation for having been able to achieve a successful release and final recovery thanks largely to the nurses” (p. 332)10 C20: “During the weaning process, the sensitivity of the nurses is very important” (p. 83)8 C21: “It was enough for me just to have the there” (p. 144)2 C22: “The nurses knew all the questions I could imagine. I felt that communication was good…” (p. 175)4 C23: “The nurses did their best to make me feel comfortable. On many occasions they did more than their share” (p. 142)2 C24: “I wanted the nurses to be around me all the time … only the nurse who was at my side could solve my problems in time” (p. 187)11 |
| The determining factors for successful IMV withdrawal. | C25: “I never focused on anything but knowing that I was going to get better, I was convinced, so you build yourself up” (p. 173)2 C26: “Yes, my relatives were very supportive … they were with me almost continuously, but they only allowed two to be with me at any one time, and sometimes they had to leave when the staff asked them to. It was nice just to touch their hands … I knew they were there” (p. 92)1 C27: “People need their family in times of stress and crisis” (p. 331)10 C28: “The most important thing was the family visit. It was the highlight of the day. It was an important moment in life” (p. 175)4 C29: “You must have confidence, if not you can say goodbye to life…” (p. 186)11 C30: “I thought that if I was optimistic I would recover faster” (p. 186)11 C31: “Having the right attitude” (p. 145)2 |
IMV withdrawal is a stressful physiological and psychological experience for patients.1,11 The results show, first, that the patient's mental and emotional state affects their functional status, and that second, other physiological variables are related to the success or failure of the IMV withdrawal.9,20
Fatigue and dyspnoea are not usually priority indicators to be considered before beginning the IMV withdrawal process.20 However, in most cases patients describe these symptoms as two of the most distressing symptoms during IMV withdrawal. In fact, dyspnoea is recognized as one of the sensations that has the greatest effect on the patient's mood, and which plays a part in developing feelings of anxiety or loss of control, which are shown as predisposing factors for a failed weaning11,20 (C1 and C2, Table 2).
Also according to the study by Wang et al.16 the patients who had undergone IMV suffered both physically (pain, discomfort) (C3 and C4, Table 2) and psychologically (feelings of helplessness, passivity, hallucinations, nightmares, altered level of consciousness) (C5 and C6, Table 2). Living such a negative experience led them to a time of evaluating the past, seeking the value and meaning of life and the importance of being as strong as possible to solve it15 (C7 and C8, Table 2).
Jubran et al.,8 in a study regarding the appearance of depressive disorders in patients undergoing IMV withdrawal, describes how patients experienced feelings of helplessness, anger, and despair because of knowing that the ability to breathe depended on a machine (C9 and C10, Table 2). It implied dependence on the ventilator, and this heightened the adverse emotions, thus delaying the weaning process. In turn, it caused the patient not to want to repeat the attempt of disconnection, and annoyance at the need of ventilatory support (C11 and C12, Table 2). In this regard, it is noteworthy that the patients went from an initial state of fear and respect for the medical team, to a state of excessive dependence and attachment, showing anxiety and fear when the ventilator was removed to begin weaning.16
In contrast, Cook et al.12 revealed that the patients’ reactions to successful weaning were reactions of hope, in comparison to the hopelessness created by failure and the fear of repetition (C13, Table 2).
Also, feelings of helplessness were shown due to the inability to communicate8,16 (C14, C15 and C16, Table 2). In the studies reviewed, the patients reported that being unable to be understood led them to experience panic and frustration. On the contrary, some patients identified feelings of relief due to being able to attract the attention of professionals by establishing communication strategies through the use of signs and gestures. In addition, some of them recognize that in the presence of their family members they managed to make themselves understood and communicate better.16
Additionally, the variation in the level of consciousness due to sedation, sleeping difficulties, thirst, lack of relatives and the difficulty to communicate caused hallucinations, asphyxia, claustrophobia and the desire to escape6,9,10,16 (C17 and C18, Table 2). These feelings affected them so much that they continued to experience high levels of anxiety, three years after being discharged from the ICU.6,16
The influence of care professionals during weaningThis discussion shows that the IMV withdrawal process is dynamic and sometimes complicated. Many patients, due to the negative emotions they experience (frustration, uncertainty, despair, fear or lack of control) are predisposed to difficulties during weaning and/or failure.9,12,17 If the healthcare personnel comprehend, understand, accompany and help the patient during this process, then they are able to meet the patients’ needs and to make the feelings of loneliness and uncertainty diminish or disappear, thereby achieving better results12 (C19, Table 2). Many patients crave the interaction with the health team and considered the contribution of the professionals by means of care and preparation, as of utmost importance. Specifically, they praise the concept of the nurse and describe their desire to spend more time with him/her7–15 (C20 and C21, Table 2).
Cook et al.12 emphasized how important it is for health professionals to recognize the situation that the patient is going through, as well as to conduct interviews and analyze the clinical documents to know each patient in depth. Within this framework, the excellent attention and attitude of care by the nurse is recognized as essential (C22, Table 2). Patients remember the nurse as a figure of support and safety, who strives to do everything necessary to ensure the patient's comfort during the process1,5 (C23, Table 2). Specifically, the nurse is attributed with the interventions aimed at increasing patient comfort, such as changes in posture, being comfortable, encouraging relaxation, control of the environment (temperature, noise, visual images, etc.), in order to promote recovery of the strength needed to cope with weaning.20
In short, the general feeling is that the proximity of a nurse gives confidence and improves well-being (C24, Table 2). However, there are still studies that evidence the lack of emphasis nurses place on some of the distressing symptoms such as fatigue and dyspnoea.10
Determinants of successful withdrawal of invasive mechanical ventilationThe literature confirms that for the IMV withdrawal to be successful, it is important to have an action plan based on interdisciplinary knowledge, research and team communication.1,6 And to avoid undesirable variations during the process, it is recommended to have protocols of action so as to aid both physiological and emotional problems.1,13
On the other hand, the studies show that although there are no indexes that determine the success or failure of weaning, it has been observed that the management of patients submitted to IMV over a long period of time differs to that of patients submitted to IMV during a short period of time.10 Weaning a patient who was submitted to IMV for a short time can be a rapid and isolated event. However, in a patient with long-term IMV, the process can last for days and weeks, and can include progress, setbacks and interruptions. Some of the factors that predispose the long-term IMV patients to suffering a complicated and abrupt weaning are: the patient's nutritional status (indicated by albumin and haemoglobin levels), being depressed (this causes psychological stress) and poor night-time rest (this produces fatigue and lack of energy).10
Regarding a weaning patient's negative feelings, literature shows how patients were able to find comfort during this vital experience despite having a negative perception and experiencing stressful emotions1 (C25, Table 2). On the one hand, it was identified that the support of the family plays a fundamental role in providing comfort, as they take charge of maintaining the level of confidence and fuelling the hopes of an early discharge15,16 (C26 and C27, Table 2). The presence of the family strengthened the patient's ability to cope with this traumatic experience, and they related to feelings of comfort and tranquillity during a time when they were experiencing great uncertainty, stress and fear15 (C28, Table 2). On the other hand, for some patients religion and spiritual encounters with loved ones or deceased persons provided them with an experience from which they gained optimism and comfort.6 In addition, both self-determination, described as the need to be as strong as possible at that moment, and self-motivation in the context of a positive attitude and self-confidence, were identified by patients as being essential to detach themselves from the ventilator15,16 (C29, C30 and C31, Table 2).
Another predominant aspect rated as the worst experience, together with pain, is the inability to communicate.1,5–15 Patients considered the use of help-strategies as adequate, and recognized the nurses’ ability to use non-verbal language to communicate effectively.7 In this sense, Engström et al.1 describes the safety and trust experienced by patients when it comes to relationships with the health team as essential for the success of IMV withdrawal. Patients were grateful when they felt they were informed and were able to know the time that they had to try to breathe without help, with the assurance that both the ventilatory support and the nurse would be there. In other words, they needed to know what was going on and then, to face it.
DiscussionThe main results of this review show that the withdrawal of IMV is an experience which marks patients for life, and is remembered with negative feelings. However, factors such as the support provided by the health team, the family or self-determination allow the person to live the experience with less physical and emotional suffering, thus promoting the feeling of control and participation in the process of withdrawing the IMV. For this reason, it is necessary to continue reflecting on what is necessary to improve this vital experience and to deepen the emotional dimension and its implication in the person.
The weaning process is stressful and causes feelings of fear, anxiety and/or distress. Physiological factors such as pain, difficulty breathing, dry mouth, feelings of hot flushes and/or suffocation make IMV a negative experience marked by feelings of discomfort and malaise, as well as feelings of helplessness, fear and apprehension. This interrelation between the subjective perceptions and the physiological variables of the patient can be complex. Hence, the evaluation of the patient's objective symptoms together with the exploration of the emotional area, are essential to starting a successful weaning.9,16,20
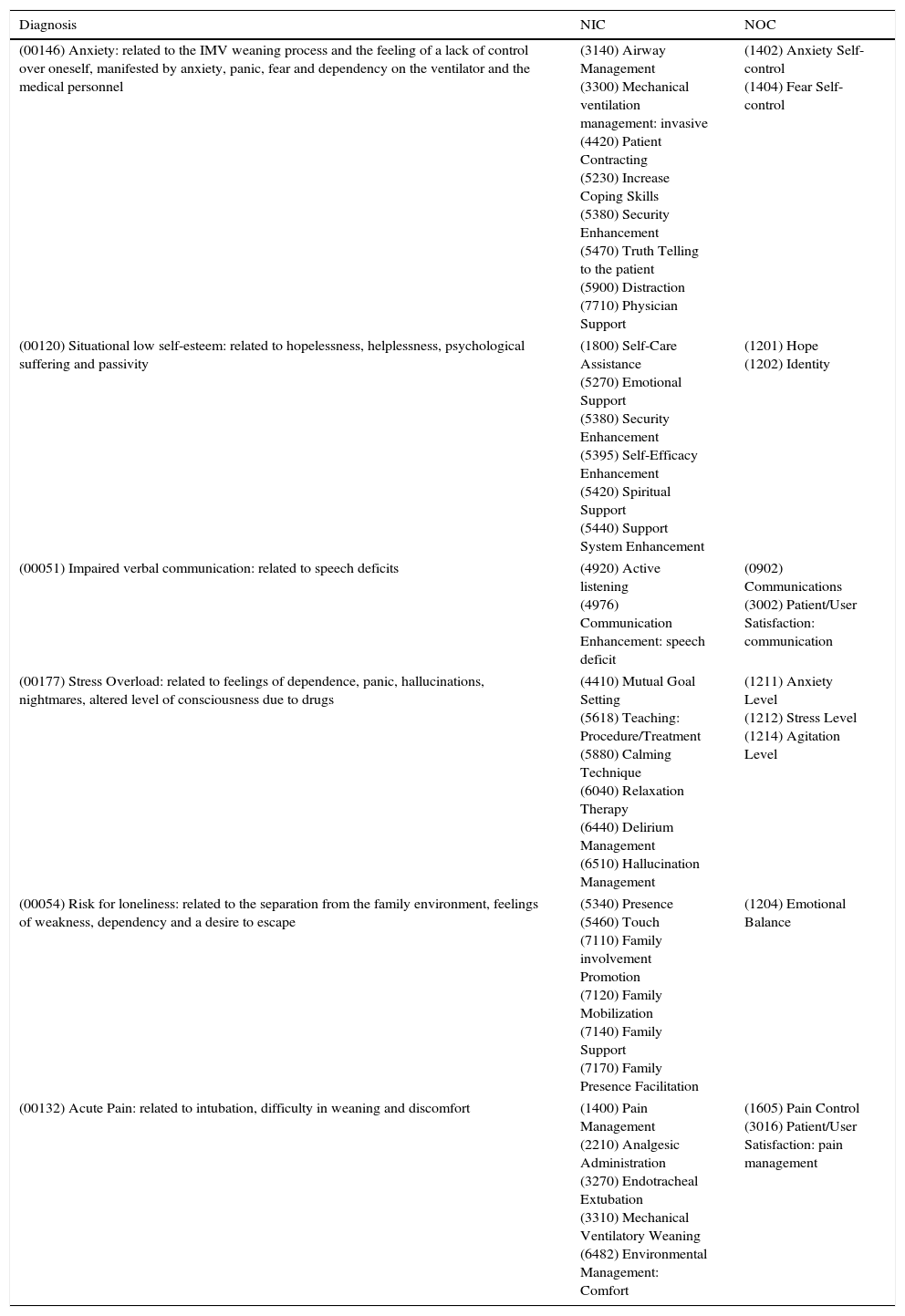
It should be noted that to encompass the set of results found, standardized nursing terminology is an adequate instrument that allows the implementation of a theoretical framework which identifies problems (NANDA),21 interventions (NIC)22 and results in care (NOC).23 Its use in different care settings is varied. In the case of ICUs, studies have been carried out during the last few years that try to understand the implications of integrating this nurse taxonomy into healthcare practices.24,25
Based on this, and with more details in Table 3, the following nursing diagnoses and interventions are highlighted: anxiety related to feelings of anxiety, panic, fear and dependency on the ventilator and the medical personnel. In this regard, providing the patient with an explanation of the weaning process and the feelings he/she may experience, using true and objective information, builds up greater trust in the nurse-patient relationship. Likewise, listening to the patient's needs is considered essential to foment the feeling of having company and reducing the fear generated by the situation.
NANDA taxonomy: NIC and NOC.
| Diagnosis | NIC | NOC |
|---|---|---|
| (00146) Anxiety: related to the IMV weaning process and the feeling of a lack of control over oneself, manifested by anxiety, panic, fear and dependency on the ventilator and the medical personnel | (3140) Airway Management (3300) Mechanical ventilation management: invasive (4420) Patient Contracting (5230) Increase Coping Skills (5380) Security Enhancement (5470) Truth Telling to the patient (5900) Distraction (7710) Physician Support | (1402) Anxiety Self-control (1404) Fear Self-control |
| (00120) Situational low self-esteem: related to hopelessness, helplessness, psychological suffering and passivity | (1800) Self-Care Assistance (5270) Emotional Support (5380) Security Enhancement (5395) Self-Efficacy Enhancement (5420) Spiritual Support (5440) Support System Enhancement | (1201) Hope (1202) Identity |
| (00051) Impaired verbal communication: related to speech deficits | (4920) Active listening (4976) Communication Enhancement: speech deficit | (0902) Communications (3002) Patient/User Satisfaction: communication |
| (00177) Stress Overload: related to feelings of dependence, panic, hallucinations, nightmares, altered level of consciousness due to drugs | (4410) Mutual Goal Setting (5618) Teaching: Procedure/Treatment (5880) Calming Technique (6040) Relaxation Therapy (6440) Delirium Management (6510) Hallucination Management | (1211) Anxiety Level (1212) Stress Level (1214) Agitation Level |
| (00054) Risk for loneliness: related to the separation from the family environment, feelings of weakness, dependency and a desire to escape | (5340) Presence (5460) Touch (7110) Family involvement Promotion (7120) Family Mobilization (7140) Family Support (7170) Family Presence Facilitation | (1204) Emotional Balance |
| (00132) Acute Pain: related to intubation, difficulty in weaning and discomfort | (1400) Pain Management (2210) Analgesic Administration (3270) Endotracheal Extubation (3310) Mechanical Ventilatory Weaning (6482) Environmental Management: Comfort | (1605) Pain Control (3016) Patient/User Satisfaction: pain management |
Another interesting aspect is the physical and emotional separation from loved ones experienced by patients during the disconnection process. While it is true that most patients emphasize the need to be accompanied by their family during their time in the ward, the desire to be with them is intensified during this process. As described by patients, the absence of the family intensifies the feelings of loneliness, weakness, dependence and the desire to escape when it is the time to be disconnected from the IMV. Therefore, encouraging the family members to be actively involved could improve the patient's physical and emotional experience. At the same time, it is considered that the active presence of family members may help the healthcare team to recognize the patient's feelings of anger, despair, anxiety and sadness and thus achieve a joint solution.
When the family is absent, the nurse is recognized by the patients as being not only a professional with high clinical competence but also a key figure and a source of support and well-being.5,7 They believe that nurses can contribute to orientation in time due to their ability to “be present”. Additionally, the patients consider that the nurses are excellent communicators, who make an effort to understand them and anticipate many of their needs.
Therefore, patients appreciate the time and efforts nurses devote to meet their needs. At the same time, patients appreciate the extra effort made by those who truly try to understand their feelings,5,7 because although it should not be forgotten that holistic care of the patient and his/her family constitute the practice of nursing, there is evidence that professionals underestimate some of the specific interventions related to more subjective needs.4,15 The times when patients feel that the nurse does not understand them or is ignoring them7 are the times that cause manifestations of frustration and insecurity.
Jenabzadeh and Chlan et al.,26 a nurse who related her experience in childhood when she underwent IMV affirms that, in contrast with her professional life, health professionals usually assure patients that they will not feel or remember the weaning process. However, this is not so in most cases. Some patients are relaxed on a muscular level, but are aware of the situation and they find the inability to move and to express themselves terrifying.25 Therefore, as stated by Wang et al.,16 it is important to take into account the subjective experiences identified by the patients so as to provide holistic care during the great challenge presented by this process.
At the same time, Jenabzadeh and Chlan26 and Cook et al.12 agree on the idea that nursing professionals play an important role during the period in which the patient remains intubated because they are the key players who meet the patient's physical needs (moistening the mouth, continuing proper oral hygiene, suctioning secretions) and psychological needs (support, confidence, dedication).
The fact that health professionals sometimes prioritize the patient's clinical status and the knowledge of his/her medical history to perform therapeutic actions26 could be related to the excessive mechanization of healthcare, which leads to an institutionalized behaviour by nurses and neglecting human aspects.10 However, we must not forget the importance of “knowing the patient” entirely, i.e. at the bedside, and in situ. This approach could prevent patients from mentioning feelings of dehumanization or depersonalization, as the fact that patients have more voice and greater control over their treatment, needs or priorities in the ICU is increasingly taking a stronger hold.
Several authors5,25 agree on the need to preserve the patients’ “being” and the need to personalize the process, individualizing decision-making and encouraging autonomy. Humanization is essential and necessary for the patient to adapt to a situation described as foreign, strange and dehumanizing.
In this context, there are many factors that directly affect the patient's ability, decision-making and control, among which the need for continual explanations for guidance is stressed. Patients need help in interpreting the environment they are in, to be able to take an active part in the process, reduce anxiety and increase their confidence.5 In addition, they can benefit from visual signs, such as a large clock, a calendar and even a sign which describes their location, to keep the patient oriented.7
This idea provides a basis for future research studies on the responsibility and the need to improve patient experience and the outcomes, as patients continue to completely trust and feel safe with the professional staff.1
Given the foregoing, it appears that the principle requirements of both the patient and his/her family, which could result in improving their experience, falls squarely on the need for more human contact. This includes taking into account their value and participation, as well as devoting time, and physical and emotional contact.7,16 However, it seems that current research lines continue to prioritize the physiological aspects.27 Although there is extensive literature on this subject, there is still a lack of consensus on some issues, such as the weaning definition, modes or techniques and/or the parameters to decide when a patient is ready to begin the process. For this reason, implementing the use of protocols would be very beneficial. Evidence reflects the benefits of following these standardized guidelines, such as a decrease in the number of IMV days, less time admitted in the ward, and less patient chronification. Consequently, this reduces the complications associated with the use of IMV such as pneumonia, bronchoaspiration, and the number of cases of accidental extubations.28 For example, the causes of accidental extubation include: patient agitation, altered level of consciousness (produced by inadequate sedation) and insecure tube clamping. So implementing protocols that governing sedation in these patients could help reduce the number of cases of accidental extubation, as well as other incidents.28,29
However, there are different opinions as to the application of protocolised interventions. Blackwood and Wilson-Barnett30 concluded, through a quasi-experimental study, that nurses with more training were more satisfied with the implementation of a protocol for weaning, compared to those with less training or practical experience. Most of them agreed that a protocol for weaning is useful, but according to Lavelle and Diwking31 some still believed that a weaning performance protocol restricts their autonomy and its use may not be as useful in practice as it claims to be.
In addition, as shown previously, the complex and changing weaning process involves not only physical aspects but it also has a direct impact on the patients’ emotions. That is why the patient requires continuous care and a personal relationship to individualize and develop a weaning plan focused on interventions that support the most subjective needs. This reflects the importance of the nurse's performance during this process.30 Hence, in recent decades the nurse's role during weaning has gained momentum.
Highlighted among the constraints encountered throughout this literature review, are the reduced number of articles dealing with the experiences of patients during weaning, unlike the substantial amount of publications that provide evidence about the experiences during IMV. On the other hand, the number of databases analyzed as well as the limit of language, have probably influenced on the loss of relevant information regarding this topic.
Regarding the implications that the proposed results may have in the field of nursing practice and research, a series of contributions have been proposed that revolve around the standardization of nursing practice during weaning, the active participation of the family and the communication process between the nurse and patient.
The need to standardize nursing practice in the process of patient care during weaning from mechanical ventilation is unavoidable, when we take into account the stated experiences, the personal needs of each patient and the need to be flexible with regard to adapting to each one of them. Hence all weaning protocols should provide for the patient's psychological and emotional dimensions throughout the process. In this regard, it is proposed that two key areas are included: information and relaxation.
On the one hand, the information should be transmitted progressively, explaining the interventions to be performed, while orienting the patient in space, time and person, being empathetic and ensuring that the patient feels accompanied at all times, explaining the sensations that the patient may experience beforehand and reinforcing the merits achieved. On the other hand, for the patient to live the process with the utmost tranquillity in this situation, it is proposed to provide an environment of security and serenity, as well as promoting gestures like kindness, affection, sensitivity, or empathy intentionality.
To meet this objective, it is essential that the nursing professionals recognize their ability to lead the development of these projects (protocols, clinical practice guidelines [GCPs]) in order to respond to the needs of the patient and his/her family during the IMV disconnection process.
Regarding the influence of the family and the benefits that patients describe with their presence. The identified results reinforce the idea that family involvement in the process has a therapeutic effect which is able to help alleviate the anxiety experienced by patients during weaning.17 In this way, the nursing professional should try to integrate the family involvement into care-giving through a holistic perspective. This process can be carried out in two phases. First, the planning of family involvement in the weaning process, prioritizing open communication with the family, evaluation of the family unit, and the identification of the family's wishes. Second, family involvement would take place.
Family involvement will consist in collaborating with the nurse in the communication process, providing emotional support through physical presence, assisting in washing the oral cavity, helping with postural changes, encouraging space and time orientation, participating in positive reinforcement, as well as giving other healthcare as planned by both the family and the nurse beforehand.
Due to the deterioration of verbal communication related to the patient's difficulty to speak when undergoing IMV, information and communication should be directed towards the active participation in decision-making, allowing for collaboration and autonomy. Hence it is deemed necessary to establish an effective communication system with the patient, in order to achieve the most effective communication possible. This can be done using traditional methods such as: blackboards; the YES/NO cards; and hand gestures; as well as new digital alternatives, such as communication boards in electronic form that can be used on a tablet or PDA. There are also programmes such as the Board Maker, the Plaphoons or Sicla 2.0, which allow communication boards to be edited, based on the objectives and needs of the user and whose purpose is to encourage communication for persons lacking functional language.
ConclusionsThe literature review shows that nurses have a key role in improving patient communication and anticipating their needs. Physical, psychological and technological care is important so as to provide holistic care. Hence training, instruction and professional practice are considered as priorities, and studies are necessary to improve the care and communication and reduce anxiety and stress of patients during IMV withdrawal.
In addition, the findings suggest the need to design protocols whose interventions are addressed to the patient and his/her family, as they are related to lessening the patient's worry and anxiety during the weaning process.
Conflict of interestsThe authors declare no conflict of interest.
To the ICU staff, to the entire teaching staff of the Clinical University of Navarra and to our families and friends for their support and understanding provided during the course of specialization.
Please cite this article as: Merchán-Tahvanainen ME, Romero-Belmonte C, Cundín-Laguna M, Basterra-Brun P, San Miguel-Aguirre A, Regaira-Martínez E. Experiencias del paciente durante la retirada de la ventilación mecánica invasiva: una revisión de la literatura. Enferm Intensiva. 2017;28:64–79.