To measure the intensity of interprofessional collaboration (IPC) in nurses of an intensive care unit (ICU) at a tertiary hospital, to check differences between the dimensions of the Intensity of Interprofessional Collaboration Questionnaire, and to identify the influence of personal variables.
MethodA cross-sectional descriptive study was conducted with 63 intensive care nurses selected by simple random sampling. Explanatory variables: age, sex, years of experience in nursing, years of experience in critical care, workday type and work shift type; variable of outcome: IPC. The IPC was measured by: Intensity of Interprofessional Collaboration Questionnaire. Descriptive and bivariate statistical analysis (IPC and its dimensions with explanatory variables).
Results73.8% were women, with a mean age of 46.54 (±6.076) years. The average years experience in nursing and critical care was 23.03 (±6.24) and 14.25 (±8.532), respectively. 77% had a full time and 95.1% had a rotating shift. 62.3% obtained average IPC values. Statistically significant differences were found (p<0.05) between IPC (overall score) and overall assessment with years of experience in critical care.
ConclusionsThis study shows average levels of IPC; the nurses with less experience in critical care obtained higher IPC and overall assessment scores.
Medir la intensidad de colaboración interprofesional (ICP) en enfermeras de una unidad de cuidados intensivos (UCI) de un hospital de tercer nivel; comprobar diferencias entre las dimensiones de la escala Intensidad de la Colaboración Interprofesional (ICP), e identificar la influencia de variables personales en la ICP.
MétodoEstudio descriptivo transversal realizado con 63 enfermeras de cuidados intensivos seleccionadas mediante muestreo aleatorio simple. Variables explicativas: edad, sexo, años de experiencia en enfermería, años de experiencia en cuidados críticos, jornada laboral y turno de trabajo; variable resultado: ICP. La ICP se midió mediante el cuestionario «Intensidad de la Colaboración Interprofesional». Se realizó análisis estadístico descriptivo y bivariante (ICP y sus dimensiones con variables explicativas).
ResultadosEl 73,8% fueron mujeres, con una edad media de 46,54 (±6,076) años. La media de años de experiencia en enfermería y en cuidados críticos fue de 23,03 (±6,24) y de 14,25 (±8,532), respectivamente. El 77% tenían una jornada completa y el 95,1%, turno rotatorio. El 62,3% tuvieron valores de ICP media. Se encontró asociación estadísticamente significativa (p<0,05) entre ICP (puntuación global) y apreciación global con años de experiencia en cuidados críticos.
ConclusionesEl estudio muestra niveles medios de ICP; las enfermeras con menos experiencia en cuidados críticos son las que puntúan más alto la ICP global y su dimensión de apreciación global.
Over the past few years, patients’ needs have gradually intensified, which implies that no professional can satisfy them on their own. Hence, interprofessional collaboration has become an essential tool for the current health systems.
This study highlights the mean intensity levels of interprofessional collaboration among nurses of an intensive care unit, identifying possible weaknesses and, consequently, potential improvements in interprofessional collaboration.
Implications of the studyThis study has enabled us to detect components related to interprofessional collaboration that need a greater degree of attention on the part of health professionals, in order to achieve improved collaborative work. Improving these levels of collaboration could improve patient health outcomes, teamwork among professionals and, ultimately, the health system as a whole. It is crucial to continue research on this matter, as the available literature shows positive results related to interprofessional collaboration in healthcare settings.
At present, patients’ health needs have become so complex1 that no professional is capable of satisfying all of them,2 transforming collaborative work into an urgent goal for health systems.
But beyond its necessary nature, interprofessional collaboration has proved to be a fundamental tool for achieving efficient and effective1 health care, as it allows for improving health outcomes and strengthening the health system,3 while promoting planned health coordination4 and helping professionals carry out their job and address problems in a more positive manner.3 Many policymakers have identified it as one of the most effective ways of dealing with the complexity of health care.3
However, working cooperatively is not an easy task.1 There are important barriers that hamper interprofessional collaboration, such as communication problems among health professionals,5–12 the ignorance of the professional roles and responsibilities of other staff members,5–7,12–14 the power and hierarchy,5,6,13–16 the lack of confidence (in the other)5,6 and even the lack of respect.5,6,8 In order to overcome these barriers, it is especially important to hold real interprofessional meetings,2,5,10,17,18 given that the actual or de facto absence of some professional groups at these meetings (in which a patient's care is decided) is still frequent.6,7,15 Nevertheless, the existence of such meetings does not suffice, and it is essential that those gathered in the meeting value the contributions of each member of the team to the patients’ health,9 in order for the meeting to not constitute a mere overlap of professionals gathered in the same setting with little interaction between them.3
The need for a change in the institutionalized forms of collaboration on behalf of all team members must, therefore, become a key element for an effective and efficient health care. However, some authors state that interprofessional collaboration may be perceived differently by the different team members.19 While physicians score the quality of the collaboration higher than nurses,5 the latter feel that they are not being heard by other professionals, particularly by doctors, which seems frustrating for them as they are unable to actively participate in interprofessional meetings.15 Nurses even perceive interprofessional collaboration as an additional stress factor derived from their work.10
These differences in the perception of interprofessional collaboration are also observed when comparing different settings of clinical practice. Primary care nurses (community settings) are satisfied with their interaction and collaboration with their peers, as they feel involved in the planning and decision making concerning patients’ health care.7,20 However, nurses working at inpatient health teams describe their work as a simple execution of orders and procedures7; and this even takes place in the intensive care unit (ICU), despite the fact that interprofessional collaboration in these units is essential to cope with the complex care required by these patients.17
In this sense, Nathanson et al.19 stated that, although ICU physicians and nurses recognize that the responsibility for the decision making process is not shared, nurses see this as proof of the lack of collaboration, while doctors are satisfied with the situation.
Johnson and Kring12 indicated another relevant fact: nurses believe that doctors are unaware of what their work consists of, and they complain about such behavior. And this still occurred despite the fact that 75% of the participating ICU nurses stated that they participated in interprofessional meetings held with doctors.
However, the review carried out by Tang et al.5 indicates that most research carried out within this context has been conducted in the United States, as a result of which both cultural and social differences, as well as differences in the health systems of other settings, are still unknown. Hence, we proposed the conduct of this study with the purpose of gaining knowledge on the intensity of professional collaboration (IPC) among nurses of an ICU setting of the south of Spain, using the Intensity of collaboration among health professionals scale, validated and adapted transculturally into Castilian Spanish by San Martín-Rodríguez et al.21
Thus, the general objective of this study was:
- •
To measure the intensity of professional collaboration (IPC) among nurses of an intensive care unit (ICU) of a tertiary level hospital.
The specific objectives of our study were:
- •
To check for differences in the different dimensions that make up the Intensity of Interprofessional Collaboration scale.
- •
To identify the influence of personal variables (sociodemographic and related to the workplace) on IPC and its different dimensions.
Cross-sectional observational descriptive study.
ScopeThe study was carried out in the ICU of a tertiary level hospital from the south of Spain, between the months of November 2015 and June 2016. The study setting consisted of a multipurpose ICU equipped with 32 beds distributed among 5 modules (heart unit, transplants unit, neurotrauma unit and 2 multipurpose modules, 1 and 2).
SubjectsThe study population was comprised by 95 nurses who were currently working at the ICU and who had at least 6 months of experience working at the service. Nurses with management functions were excluded from the study.
The sample size was calculated for an infinite population, with a typical deviation of 6.84,22 a maximum imprecision of 1.7 and a 95% confidence level, resulting in a total of 63 sample subjects. To select these nurses, we carried out a simple random sampling on the list of nurses working at the unit (who met the inclusion criteria).
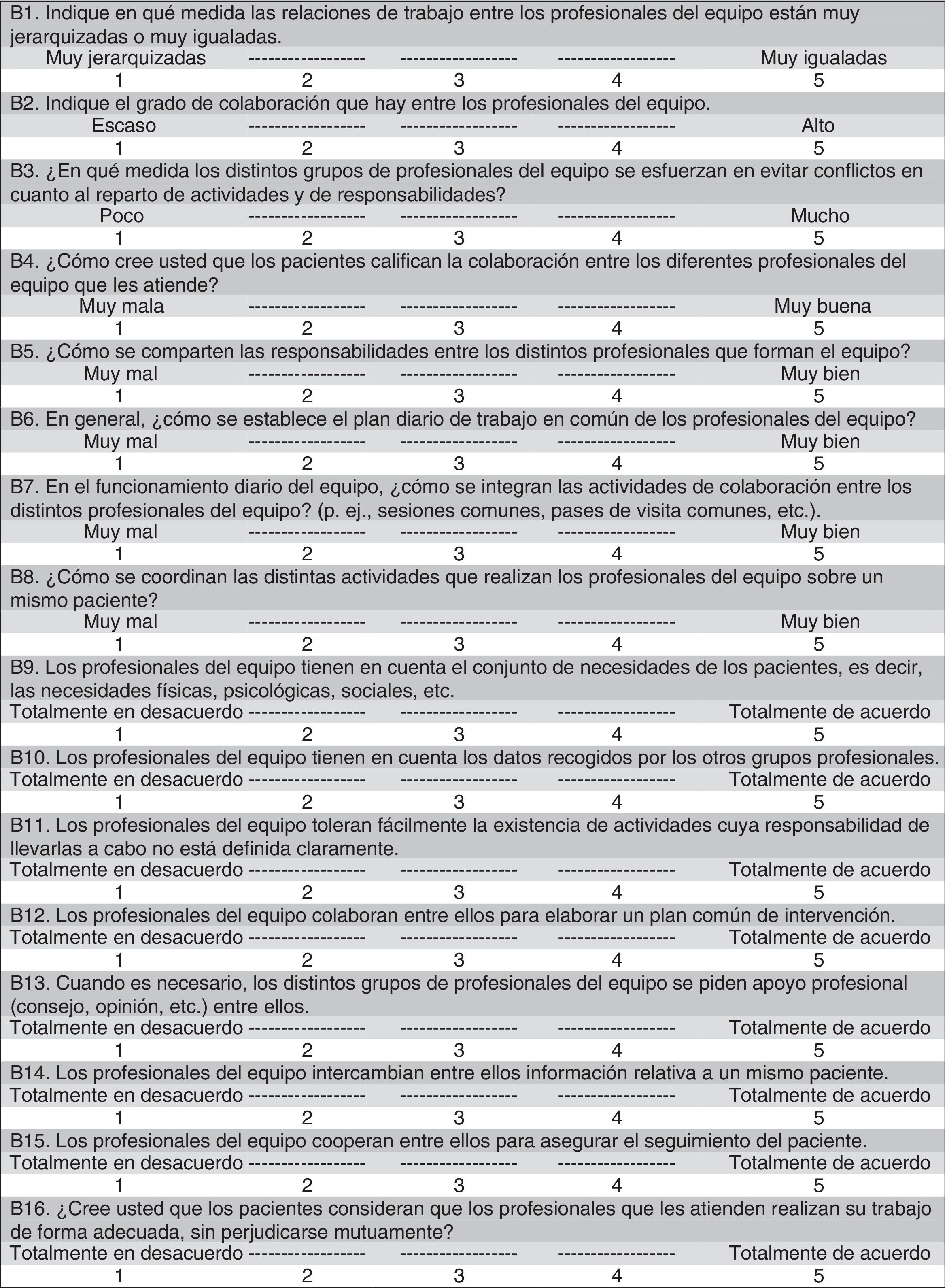
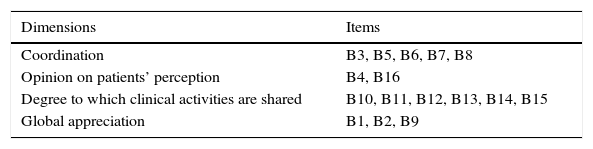
Variables and measuring toolsThe intensity of the collaboration was measured with the self-administered Intensité de la Collaboration Interprofessionnelle (Intensity of Interprofessional Collaboration [IPC]) scale, developed by Sicotte et al.,23 and translated and validated in Spanish by San Martín-Rodríguez et al.21 The tool, validated into Castilian Spanish, consists of 16 items (with 2 items having been removed from the original questionnaire), evaluated by a 5-point Likert scale, with the minimal score being 16 and the maximum one being 80 (Fig. 1). Unlike the original tool, this tool suggests the existence of 4 factors, adding another 2 to the original 2 (“coordination” and “degree to which clinical activities are shared”); the “opinion on patients’ perception” and “global appreciation”. These 4 factors explain 61.47% of the total variance. The analysis of the internal consistency of the Spanish version yielded a Cronbach's alpha coefficient of 0.907. Table 1 shows the items of each dimension of the version validated into Castilian Spanish.
Intensity of Collaboration among Health Professionals Scale.21
The stratification of the collaboration followed the levels created by Bengoechea Calpe et al.22 According to these authors, IPC is considered to be high if the scores range from 80 to 60 points, average if they range from 59.99 to 38 points and low if they range from 37.99 to 16 points. According to this same criterion, the scale's dimensions are structured in the following way:
- •
Coordination: high from 25 to 19 points, average from 18.99 to 12 points and low from 11.99 to 5 points.
- •
Opinion on patients’ perceptions: high from 10 to 8 points, average from 7.99 to 5 points and low from 4.99 to 2 points.
- •
Degree to which the clinical activities are shared: high from 30 to 22 points, average from 21.99 points and low from 13.99 to 6 points.
- •
Global appreciation: high from 15 to 11 points, average from 10.99 to 7 points and low from 6.99 to 3 points.
Other study variables included were age, sex, years of nursing experience, years of work experience in the critical care unit, type of working day (full-time, part-time, hourly and other) and shift (rotating, fixed – mornings, afternoons, nights, other).
Due to the small number of cases of some categories related to the type of working day and shift variables, we recorded these as dichotomous variables: full-time and other, in the first case; rotating and other, in the second case.
Moreover, to improve comparability with the study performed by Bengoechea Calpe et al.,22 we classified the continuous quantitative variables into 4 groups according to the variables’ quartiles: age (range 1 [35–42], range 2 [43–47], range 3 [48–51] and range 4 [52–62]), years of nursing experience (range 1 [9–20], range 2 [21–23], range 3 [24–27] and range 4 [28–42]) and years of experience working at the critical care unit (range 1 [1–8], range 2 [9–12], range 3 [13–21.5] and range 4 [21.6–40]).
Data collectionThe questionnaire was delivered by hand and collected in a sealed envelope by the principal investigator, upon request of the subjects’ participation through an informed consent, both in writing and verbally. The deadline for data collection was 10 days, from 4 May 2016 to 13 May 2016, in the studied Intensive Care Unit.
Data analysisA descriptive univariate analysis was carried out of the nurses’ sociodemographic variables and of the IPC questionnaire (its 4 dimensions and the items that comprise them), including frequencies, means and standard deviations.
We then checked if the outcome variables had a normal distribution among the different stratified groups with the Shapiro–Wilk test, using both parametric and non-parametric tests according to the results of the normality test.
Thereafter, we analyzed the relationship between the results of the IPC and its dimensions (as quantitative variables) with respect to the dichotomized variables, using Student's t-test and Mann–Whitney's U-test according to whether or not they had a normal distribution.
Furthermore, to analyze the relationship between the IPC and its dimensions (as quantitative variables), with respect to the groups defined per quartiles, we used an analysis of simple variance with a post hoc least significant difference (LSD), and as a non-parametric test we used Kurskal–Wallis's test, with subsequent Mann–Whitney U tests carried out in pairs, and adjusting the p-values by Finner's adjustment (WinPepi software version 11.62).
The confidence interval defined in all cases was 95%. The statistical software package used was SPSS Statistics v.23.
Ethical considerationsThis research complies with the current legislation on personal data protection and the regulatory framework of reference for the execution of Research projects in Spain or the European Union. Good Clinical Practice standards and the ethical principles set out by the Declaration of Helsinki, and its subsequent revisions, for research on human beings, were met at all times.
The study protocol was approved by the province's Research Ethics Committee.
ResultsSociodemographic variablesOf the 95 nurses working at the ICU under study, a total of 63 participated in our study. Two cases were excluded due to lack of information. Of the 61 nursing professionals enrolled in the study, 73.8% (45) were women with a mean age of 46.54 (±6.076) years. The mean time of overall nursing experience was 23.03 (±6.2) years, and the mean time of experience working at the ICU was 14.25 (±8.532) years.
Out of all professionals interviewed, 77% (47) worked full-time and 95.1% (58) had a rotating shift.
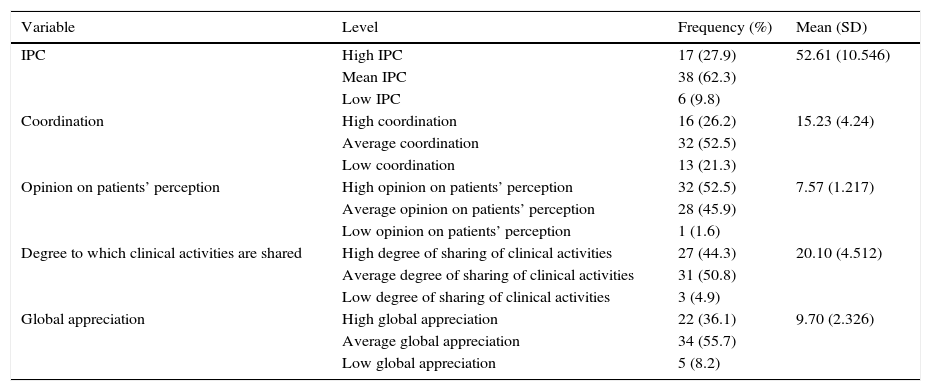
Intensity of Collaboration among Health Professionals ScaleTable 2 shows the mean scores obtained in the Intensity of Collaboration among Health Professionals Scale, including both the overall IPC score, and the scores of the 4 dimensions that comprise it.
Results of the intensity of professional collaboration and dimensions.
| Variable | Level | Frequency (%) | Mean (SD) |
|---|---|---|---|
| IPC | High IPC | 17 (27.9) | 52.61 (10.546) |
| Mean IPC | 38 (62.3) | ||
| Low IPC | 6 (9.8) | ||
| Coordination | High coordination | 16 (26.2) | 15.23 (4.24) |
| Average coordination | 32 (52.5) | ||
| Low coordination | 13 (21.3) | ||
| Opinion on patients’ perception | High opinion on patients’ perception | 32 (52.5) | 7.57 (1.217) |
| Average opinion on patients’ perception | 28 (45.9) | ||
| Low opinion on patients’ perception | 1 (1.6) | ||
| Degree to which clinical activities are shared | High degree of sharing of clinical activities | 27 (44.3) | 20.10 (4.512) |
| Average degree of sharing of clinical activities | 31 (50.8) | ||
| Low degree of sharing of clinical activities | 3 (4.9) | ||
| Global appreciation | High global appreciation | 22 (36.1) | 9.70 (2.326) |
| Average global appreciation | 34 (55.7) | ||
| Low global appreciation | 5 (8.2) |
The mean global IPC score was 52.61 (±10.546), which corresponds to an average IPC. Only 27.9% of participants showed high IPC values.
With regard to the dimensions that make up the questionnaire, the lowest levels of collaboration were recorded for “global appreciation” and “coordination”. In both dimensions, less than 40% of participants rated the level of collaboration as high; 22 (36.1%) high global appreciation, and 16 (26.2%), high coordination (Table 2).
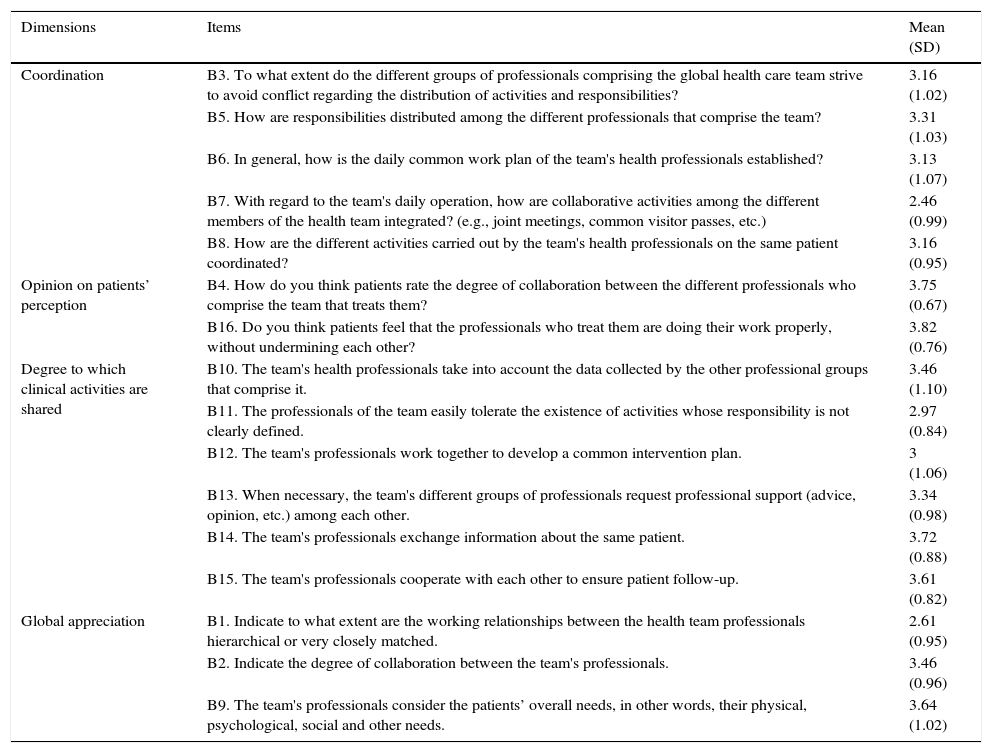
Moreover, the items with the lowest mean scores (below 3) were recorded in these 2 dimensions. These items were: B1 (global appreciation): “Indicate to what extent are the working relationships between the health team professionals hierarchical or very closely matched”, and B7 (coordination): “(During the team's daily operation, how are collaborative activities among the different members of the health team integrated? e.g., joint meetings, common visitor passes, etc.)” (Table 3).
Mean scores of the questionnaire items.
| Dimensions | Items | Mean (SD) |
|---|---|---|
| Coordination | B3. To what extent do the different groups of professionals comprising the global health care team strive to avoid conflict regarding the distribution of activities and responsibilities? | 3.16 (1.02) |
| B5. How are responsibilities distributed among the different professionals that comprise the team? | 3.31 (1.03) | |
| B6. In general, how is the daily common work plan of the team's health professionals established? | 3.13 (1.07) | |
| B7. With regard to the team's daily operation, how are collaborative activities among the different members of the health team integrated? (e.g., joint meetings, common visitor passes, etc.) | 2.46 (0.99) | |
| B8. How are the different activities carried out by the team's health professionals on the same patient coordinated? | 3.16 (0.95) | |
| Opinion on patients’ perception | B4. How do you think patients rate the degree of collaboration between the different professionals who comprise the team that treats them? | 3.75 (0.67) |
| B16. Do you think patients feel that the professionals who treat them are doing their work properly, without undermining each other? | 3.82 (0.76) | |
| Degree to which clinical activities are shared | B10. The team's health professionals take into account the data collected by the other professional groups that comprise it. | 3.46 (1.10) |
| B11. The professionals of the team easily tolerate the existence of activities whose responsibility is not clearly defined. | 2.97 (0.84) | |
| B12. The team's professionals work together to develop a common intervention plan. | 3 (1.06) | |
| B13. When necessary, the team's different groups of professionals request professional support (advice, opinion, etc.) among each other. | 3.34 (0.98) | |
| B14. The team's professionals exchange information about the same patient. | 3.72 (0.88) | |
| B15. The team's professionals cooperate with each other to ensure patient follow-up. | 3.61 (0.82) | |
| Global appreciation | B1. Indicate to what extent are the working relationships between the health team professionals hierarchical or very closely matched. | 2.61 (0.95) |
| B2. Indicate the degree of collaboration between the team's professionals. | 3.46 (0.96) | |
| B9. The team's professionals consider the patients’ overall needs, in other words, their physical, psychological, social and other needs. | 3.64 (1.02) |
Of all the independent variables collected throughout the study, only variable “years of experience working at a critical care unit” showed significant differences with respect to the IPC and the coordination and global appreciation dimensions.
Intensity of interprofessional collaboration/years of experience working at a critical care unitWhen comparing the global IPC score with the 4 ranges of variable “years of experience working at a critical care unit” we observed significant differences (p=0.050). A subsequent analysis revealed significant differences between range 1 and range 2 (p=0.011), and between range 1 and range 4 (p=0.047), of the variable.
Global appreciation/years of experience working at a critical care unitThe comparison between the 4 ranges of variable “years of experience working at a critical care unit” and the global appreciation variable, showed significant differences (p=0.050), when comparing range 1 with range 2 (p=0.008) and range 1 with range 4 (p=0.045).
Coordination/years of experience working at a critical care unitWe also observed statistically significant differences when comparing the coordination variable with the ranges of variable “years of experience working at a critical care unit” (p=0.032). However, significance was lost after adjusting the p-values for multiple comparisons.
DiscussionThe results of this study demonstrated an average degree of collaboration indicative of deficiencies in interprofessional collaboration.
Our results are much lower than those reported by Bengoechea Calpe et al.,22 whose mean IPC score was high (61.68±6.84], according to the previous classification established in that same study. This difference may be due to the fact that the mean age of our study participants was approximately 11 years older than that of the subjects included in the study conducted by Bengoechea Calpe et al.,22 which could hamper collaborative working relationships due to the existence of generational differences, as stated by Moore and Prentice.14
When considering all the dimensions that make up the scale, we observed that our participants obtained higher scores in variables “degree to which clinical activities are shared” and “opinion on patients’ perception”. Therefore, it seems that the coordination and global appreciation dimensions are the main factors accounting for the mean IPC values.
As in the case of the global scores, the scores obtained in our study for each dimension of the questionnaire were lower than those reported by Bengoechea Calpe et al.22
In our study, it is important to note the participants’ concern for 2 of the main issues included among the worst-rated items: the integration of collaborative activities (such as common sessions) and hierarchical common sessions, which shows the interest of ICU professionals to integrate common collaborative activities between different health professionals in their daily work, and to maintain more equal professional relationships among the health team.
With regard to the participants’ concern for the integration of collaborative activities in their daily work, our results coincide with those of previous studies reporting that, in spite of the conduct of professional meetings, these do not tend to include all the health professionals comprising the work teams,24 and they rather tend to constitute uniprofessional meetings segmented by types of profession,25 which hinders potential positive collaborations among members of the health team.24
In this regard, the study carried out by Alexanian et al.15 highlights than in the ICUs studied, teamwork was carried out in a uniprofessional way, with doctors being responsible for all decision making processes, whereas the rest of professionals only participated by providing information specific to their profession when required.
Reeves et al.25 reported similar findings, stating that doctors and nurses (from ICUs) worked separately and only interacted with each other briefly and randomly to resolve any clinical matter. In this same study, Reeves et al.25 also stated that the second major issue of concern was hierarchical relationships, as in our case. According to these authors, not only are the interactions insufficient, but also, interprofessional discussions are marked by the traditional hierarchy of doctors over the rest of health professionals.25
This same finding was reported by Johnson and Kring,12 who asserted that the nurses interviewed in their study, despite claiming that the doctors respected their decisions, and rating their doctor–nurse relationships as satisfactory, reported feeling subordinate to the doctors.
However, in contrast to the above, some dissonant voices with respect to the issue of the lack of joint collaborative activities and the existence of hierarchical working relationships are also found in the available literature, such as the case of Egerod et al.,26 who reported that nurses from an ICU reported that the decision-making process was carried out in an interprofessional manner, and that all decisions were made during collaborative meetings.
If we now focus on the relationships observed between the general IPC scores, the global appreciation and the years of working experience at a critical care unit, participants with fewer years of experience working at an ICU felt that, in general, the levels of interprofessional collaboration were adequate, as opposed to the claims of more experienced workers. These results coincide with those reported by Bengoechea Calpe et al.,22 who found statistically significant differences between the second and first range of years of working experience: 11–20 and 21–29, respectively (nurses with intermediate experience vs nurses with extensive experience), when comparing IPC according to the years of experience working at the ICU. This may owe to the fact that more experienced professionals, and, therefore, professionals of older age, are less interested in cooperating with younger team members, or with less experience, as observed by Moore and Prentice14 in their study carried out in an oncological clinic.
With regard to the relationship observed between IPC and global appreciation according to the years of working experience in the critical care unit (ranges 1 and 2), no clear explanation as to why our 2 lower ranges differed to such extent was found in the available literature. However, we believe that there could be a possible explanation: the decision to carry out the composition of the different ranges according to the quartiles of variable “years of experience working at a critical care unit” conditioned the existence of extremely different groups: while range 1 comprised 8 years, range 2 only comprised 4 years, which could have generated a difference in this second range with respect to the rest of groups, especially compared to range 1. In future studies we may try to confirm this possible influence, or try to find another explanation, in order to understand what could have caused this range to be so different from the other groups.
The following are the most relevant limitations of our study:
Given that it is a cross-sectional study, we could not ensure the directionality of the relationships. Also, given that we used a self-administered questionnaire, provided and collected in a closed envelope after a specific period of time, we do not have absolute certainty of the identity of the person who answered it, nor of the potential influence of a third person in the responses.
Furthermore, given that no tool assessing interprofessional collaboration has been validated in Castilian Spanish, and that it could not be provided to doctors and nurses in the hospital setting, we had to choose a specific scale validated only for nurses. However, this decision enabled us to study the group of professionals with the most dissatisfaction with respect to interprofessional collaboration.
Also, despite the fact that the questionnaire of choice has shown a good degree of validity and reliability to measure the degree of collaboration among health professionals of interprofessional teams, it is a tool that, according to its authors,21 needs to be further examined in order to assess potential problems associated with the geographical region or the specific professional group.
To the above, we must also add that the choice of this tool has caused us to have to compare the results of our study with those of other studies using different tools, and in some case, even different methodologies.
Finally, it should also be noted that our study differs greatly from that carried out by Bengoechea Calpe et al.,22 as the latter was carried out in a much smaller ICU with younger health professionals. This has caused comparisons between groups not to be exactly the same.
ConclusionsThis study has made it possible to gain knowledge on the intensity of IPC among nurses working at ICUs, with the levels of collaboration being average. In our study, the lowest levels corresponded to the “coordination” and “global appreciation” dimensions. With regard to the influence of personal variables on IPC and its dimensions, we only found a relationship between variables “years of experience working at a critical care unit” and “global appreciation”.
This research topic is still very recent and much has yet to be discovered on this matter. Therefore, we recommend the conduct of future research studies related to IPC in critical care units in order to compare different studies.
Ethical responsibilitiesProtection of human and animal subjectsThe authors of this study declare that the procedures followed conformed to the ethical standards of the Committee responsible for human experimentation, the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they followed the protocols established by their work center regarding the publication of patient data.
Right to privacy and informed consentThe authors obtained the informed consent of all patients and/or subjects referred to in this study. This document is currently in the possession of the corresponding author.
FundingThe authors declare that they did not receive any sort of external funding.
Conflict of interestThe authors declare no conflict of interest.
We are grateful for the collaboration and willingness of all the professionals working at the critical care unit of the University Hospital Reina Sofía of Cordoba to participate in this study, and for their interest in improving interprofessional relationships as a basis for health care. Also, we would like to thank Rafael Serrano del Rosal and Marina García Martínez for their collaboration in the final revision of the manuscript.
Please cite this article as: Serrano-Gemes G, Rich-Ruiz M. Intensidad de colaboración interprofesional entre enfermeras de cuidados intensivos de un hospital de tercer nivel. Enferm Intensiva. 2017;28:48–56.