To determine the opinion of healthcare staff (HS) on the presence of minors in an adult intensive care unit.
MethodTransversal descriptive research study in an adult intensive care unit with 62 people, between September/December 2017. The Knutsson questionnaire was used with 10 closed questions with space for comments, and 2 open questions.
Selection of the respondents was by means of convenience sampling. Descriptive statistics with absolute frequencies and percentages. Chi-squared-test or Fisher. Significance p<.05.
Results61 questionnaires were collected: 70.5% nursing staff (NS).
Fifty percent of medical staff (MS) would restrict the entry of 0–6-year old minors versus 76.2% NS (p=.04). Of the MS, 16.7% would restrict the visits of minors between the ages of 7 and 12 versus 46.5% NS (p=.02).
Seventy-five percent of HS thought that minors’ access could entail a risk of infection for the children. Of the survey respondents, 60% believed that the environment could intimidate the minor, and 66.7% thought that the patient's condition could affect the child. They would permit 0–6-year-old minors to access the ICU if the patient was dying (70.6% MS/41% NS, p=.04), awake and alert (77.8% MS/57.5% NE) and close relatives (parents) (66.7% MS/60% NS).
ConclusionsHS support minors visiting an adult intensive care unit if they are >6 years old. HS show a more positive attitude towards visits in special circumstances such as close relatives, awake patient, and death regardless of their age. The reasons for restriction of visits are: environment, patient's condition and risk of infection.
NS show a less positive attitude in relation to visits.
Determinar las opiniones del equipo asistencial (EA) ante la visita de menores en una unidad de cuidados intensivos de adultos.
MétodoEstudio descriptivo transversal en una unidad de cuidados intensivos de adultos con un EA de 62 personas, entre septiembre-diciembre 2017. Se utilizó el cuestionario de Knutsson con 10 preguntas cerradas con espacio para comentarios y 2 abiertas.
Selección de los encuestados mediante muestreo de conveniencia. Estadística descriptiva con frecuencias absolutas y porcentajes. Prueba de Chi2 o Fisher. Significación p<0,05.
ResultadosSe recogieron 61 cuestionarios: 70,5% correspondían a personal de enfermería (PE).
El 50% de profesionales médicos (PM) restringiría la entrada de menores de 0-6 años frente al 76,2% de PE (p=0,04). Entre 7-12 años, el 16,7% de PM la limitaría frente al 46,5% del PE (p=0,02).
El 75% del EA opinó que la entrada podía significar riesgo de infección para el menor. El 60% creyó que el entorno podía intimidarlo y el 66,7% que podía impresionarlo el estado del paciente. Permitirían la entrada de menores de 0-6 años, si el paciente se estuviera muriendo (70,6% PM y 41% PE) p=0,04), despierto (77,8% PM y 57,5% PE) o parentesco cercano (padre/madre) (66,7% PM y 60% PE).
ConclusionesEl EA es partidario de la visita con una edad >6 años. En circunstancias especiales: parentesco cercano, paciente despierto o muerte son más permisivos independientemente de la edad. Los motivos de restricción son: entorno, estado y riesgo de infección.
El PE es más restrictivo ante la visita.
Despite belonging to the family group, visits from minors are not usually considered within the adult ICU organisational structure.
The care team staff has different opinions regarding visits from minors, with nurses being the collective least in favour of allowing it. Many of the points of view expressed are not based on scientific evidence.
Implications of the studyTo implement visiting policies for minors to adult ICUs it is essential to be aware of the barriers from care teams. Given the controversy of this issue, further research and broader studies are required.
Hospitalisation of a family member to an intensive care unit (ICU) is a critical situation and may lead to changes in the family nucleus.1,2
Within the family, considered as a social unit, formed by a group of individuals linked by marriage, family relationships or afinity,3 there are also minors, who perceive of a change in behaviour of their parents when hospital admittance takes place, and their information regarding the new situation is limited. This may lead to feelings of confusion, solitude, jealousy and sadness.4
The revised literature5–8 proposes visits from minors as a method for helping children to confront this situation since it allows them to ask questions and express their emotions, reduces feelings of guilt, separation nor abandonment and increases the understanding and feeling of belonging to the family group, improving the ability to face up to and master difficult situations.
During the 80s in the United States visits from siblings9 into paediatric ICUs were introduced, with visual training and emotional support from nurses prior to entry. This led to the development of programmes dependent upon the age, level of development and personality of the minor, to give support before, during and after the visit.10 Nationally, there are different initiatives such as those promoted by the movement to humanise intensive care (HICU project) or that undertaken in the neonatal ICU of the Hospital Vall d’Hebron in Barcelona (Projecte Germans) which consists of preparing siblings through games, reproducing the environment they will find in the Unit.11 However, these strategies have not been much implemented in adult ICUs.12
Despite the introduction of new initiative, as previously stated, currently in ICUs hours are usually restricted which may impede contact with the family. This does in fact occur and according to the study by Escudero et al.,13 it occurs in 90.2% of Spanish ICUs where the most frequent visiting hours (67.7%) are twice daily, although in daily practice unwritten or extraofficial, more flexible and permissible visiting policies are often used, but these depend on the care team (CT) and more specifically on the nursing staff (NS).7
The main causes why the CT does not allow entry by majors are emotional traumas, risk of infection14 and not knowing how to confront the emotions expressed by the children.15 Although research does not support these reasons6,8,16 in most units they do not even contemplate the possibility of minors going to visit a loved one and they are, in fact, completely overlooked.
At present with a broader outlook and care focused on the family there is a tendency to open the doors of the ICU. However, it is important to emphasise that there is no universal definition of the meaning of “open door ICU”, since for example, visits for minors are not usually mentioned and there continue to be certain restrictions in this respect.17 This is why there is a need to discover which obstacles or barriers of the CT could be due to reticence, insecurities or the fact they give advice or recommendations that confuse the family members. Studies on this controversy are scarce and international in nature.
ObjectiveTo determine the opinions of the care team to visits from minors to adult ICUs.
MethodA cross-sectional descriptive study conducted in a multi-purpose ICU with 12 beds in a tertiary level hospital between September and December 2017. The population to study comprised 62 people, of whom 18 were doctors, and 44 nursing staff, specifically 31 nurses and 13 nursing auxiliaries. There was no ancillary staff in this unit.
The personnel were selected using non probalisitc convenience sampling. All people with a job in the ICU were included, regardless of the type of contract or years of experience in the job. Staff who did not wish to participate were excluded.
The Knutsson et al.15 questionnaire was used as a tool, with a test-retest reliability coefficient of .92. This questionnaire included the main reasons found in the literature to restrict or allow visits from minors in the ICU.
The transcultural adaption of this questionnaire was structured into three stages. The first consisted of its translation from English into Spanish by two people who were fluent in both languages. The two translations were reviewed by the research team for detection of errors and interpretation of some of the items, producing the first version in Spanish as a result. During the second stage, the re-translation of the first version from Spanish into English was made by two bilingual translators, who had not been used in the first phase. The 2 versions were compared by the research team to search for possible discrepancies, resulting in a final consensual version with the 4 translators involved in the process. In a third and final stage, the questionnaire in Spanish was passed onto the NS of the semi critical unit (n=20), to identify words or questions that were difficult to comprehend, and the time used for completion was obtained as a median of 17 (P25=15 P75=20) min. Once this phase was completed the results obtained from the final version of the questionnaire translated into Spanish were analysed (Banexo 1 appendix). These results did not form part of the final results.
The final questionnaire consisted of 10 closed questions (yes/no/I don’t know) with a space for explanatory comments of the response given and 2 open-ended type questions.
Sociodemographic datas were also included, such as age and sex (man/woman), years of professional experience, professional category (nurse/nursing auxiliary/doctor) and existence of children (yes/no).
This was an anonymous, self-completion questionnaire and was handed out with an envelope at the workplace on an agreed collection day and time.
Descriptive statistics with medians were used (25-percentile 75 percentile), means (standard deviation) and proportions. In the bivariate analysis the Chi square test was used or the exact Fisher test to determine the relationship between profession and the different qualitative variables and, the Student's t-test for the quantitative data. For data response analysis to open questions 4 categories were used referring to the patient, family, environment and others.
The level of statistical significance was established as p<.05. Statistical analysis was made with the SPSS programme version 17 for Windows.
The study received the approval of the Clinical Research Ethics Committee and authorisation from the hospital. Since participation was voluntary no informed consent was regarded as necessary as response to the questions was considered as acceptance of participation in this study.
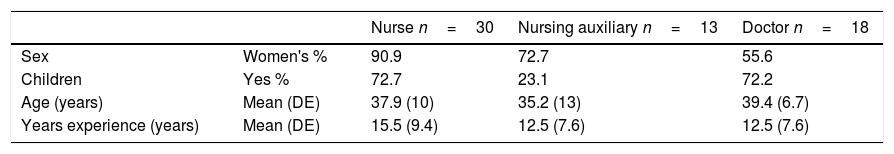
ResultsA total of 61 questionnaires were collected (98.4% of the population), 29.5% corresponded to medical professionals (MP) and 70.5% to the NS (69.8% nurses and 30.2% nursing auxiliaries). Table 1 contains the socio-demographic data.
No statistically significant differences were established between age (p=.5), years of professional experience (p=.6) or sex (p=.6) of the MP or NS and whether they were more permissive regarding visits from minors.
28.6% of the CT who had children would allow access to the ICU compared with 23.1% of the staff without children (p=.6).
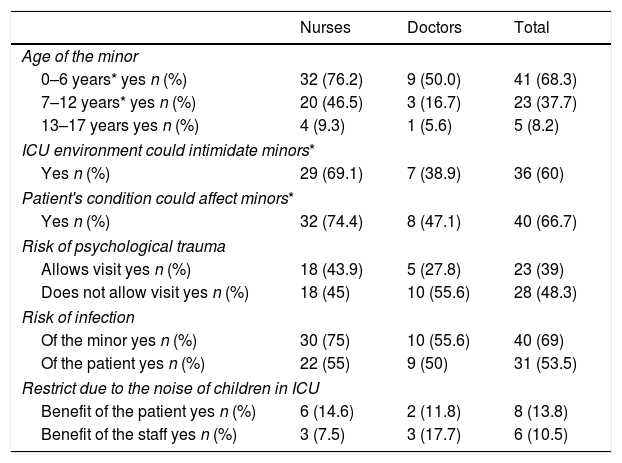
In general, both the MP and the NS clearly and concisely allowed for minors to enter into the ICU if there were aged between 13 and 17 years. The NS would be more restrictive towards the visit, compared with the NS, if the minor was <12 years (p=.04) (Table 2).
Main reasons for restricting the visit of minors to the ICU.
| Nurses | Doctors | Total | |
|---|---|---|---|
| Age of the minor | |||
| 0–6 years* yes n (%) | 32 (76.2) | 9 (50.0) | 41 (68.3) |
| 7–12 years* yes n (%) | 20 (46.5) | 3 (16.7) | 23 (37.7) |
| 13–17 years yes n (%) | 4 (9.3) | 1 (5.6) | 5 (8.2) |
| ICU environment could intimidate minors* | |||
| Yes n (%) | 29 (69.1) | 7 (38.9) | 36 (60) |
| Patient's condition could affect minors* | |||
| Yes n (%) | 32 (74.4) | 8 (47.1) | 40 (66.7) |
| Risk of psychological trauma | |||
| Allows visit yes n (%) | 18 (43.9) | 5 (27.8) | 23 (39) |
| Does not allow visit yes n (%) | 18 (45) | 10 (55.6) | 28 (48.3) |
| Risk of infection | |||
| Of the minor yes n (%) | 30 (75) | 10 (55.6) | 40 (69) |
| Of the patient yes n (%) | 22 (55) | 9 (50) | 31 (53.5) |
| Restrict due to the noise of children in ICU | |||
| Benefit of the patient yes n (%) | 6 (14.6) | 2 (11.8) | 8 (13.8) |
| Benefit of the staff yes n (%) | 3 (7.5) | 3 (17.7) | 6 (10.5) |
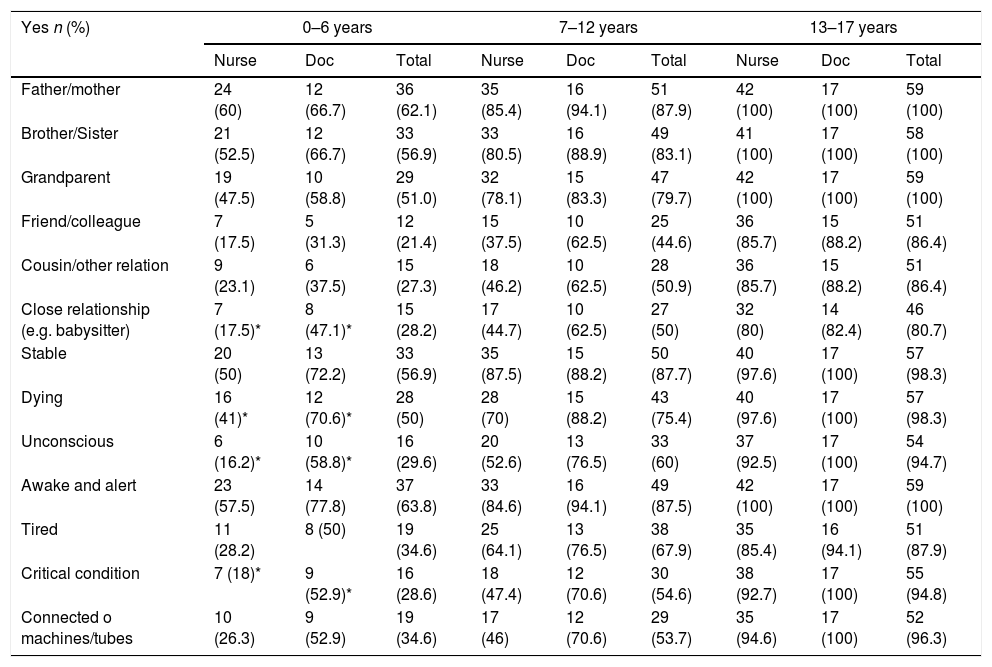
On exploring the viewpoint of the CT according to level of family relationship and condition of the patient (Table 3), the MP with 47.1% compared to the 17.5% of the NS were more permissive to the entry of minors when the link between the patient and the minor from 0 to 6 years was a close relationship (p<.01). Similarly, the MP, with 70.6% compared with 41% of the NS would have permitted the visit at this same age range if the patient had been unconscious (p<.01), at risk of imminent death (p=.04) or in a critical condition (p<.01).
Permit the visit of minors in the ICU depending on the family relationship or patient status.
| Yes n (%) | 0–6 years | 7–12 years | 13–17 years | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Nurse | Doc | Total | Nurse | Doc | Total | Nurse | Doc | Total | |
| Father/mother | 24 (60) | 12 (66.7) | 36 (62.1) | 35 (85.4) | 16 (94.1) | 51 (87.9) | 42 (100) | 17 (100) | 59 (100) |
| Brother/Sister | 21 (52.5) | 12 (66.7) | 33 (56.9) | 33 (80.5) | 16 (88.9) | 49 (83.1) | 41 (100) | 17 (100) | 58 (100) |
| Grandparent | 19 (47.5) | 10 (58.8) | 29 (51.0) | 32 (78.1) | 15 (83.3) | 47 (79.7) | 42 (100) | 17 (100) | 59 (100) |
| Friend/colleague | 7 (17.5) | 5 (31.3) | 12 (21.4) | 15 (37.5) | 10 (62.5) | 25 (44.6) | 36 (85.7) | 15 (88.2) | 51 (86.4) |
| Cousin/other relation | 9 (23.1) | 6 (37.5) | 15 (27.3) | 18 (46.2) | 10 (62.5) | 28 (50.9) | 36 (85.7) | 15 (88.2) | 51 (86.4) |
| Close relationship (e.g. babysitter) | 7 (17.5)* | 8 (47.1)* | 15 (28.2) | 17 (44.7) | 10 (62.5) | 27 (50) | 32 (80) | 14 (82.4) | 46 (80.7) |
| Stable | 20 (50) | 13 (72.2) | 33 (56.9) | 35 (87.5) | 15 (88.2) | 50 (87.7) | 40 (97.6) | 17 (100) | 57 (98.3) |
| Dying | 16 (41)* | 12 (70.6)* | 28 (50) | 28 (70) | 15 (88.2) | 43 (75.4) | 40 (97.6) | 17 (100) | 57 (98.3) |
| Unconscious | 6 (16.2)* | 10 (58.8)* | 16 (29.6) | 20 (52.6) | 13 (76.5) | 33 (60) | 37 (92.5) | 17 (100) | 54 (94.7) |
| Awake and alert | 23 (57.5) | 14 (77.8) | 37 (63.8) | 33 (84.6) | 16 (94.1) | 49 (87.5) | 42 (100) | 17 (100) | 59 (100) |
| Tired | 11 (28.2) | 8 (50) | 19 (34.6) | 25 (64.1) | 13 (76.5) | 38 (67.9) | 35 (85.4) | 16 (94.1) | 51 (87.9) |
| Critical condition | 7 (18)* | 9 (52.9)* | 16 (28.6) | 18 (47.4) | 12 (70.6) | 30 (54.6) | 38 (92.7) | 17 (100) | 55 (94.8) |
| Connected o machines/tubes | 10 (26.3) | 9 (52.9) | 19 (34.6) | 17 (46) | 12 (70.6) | 29 (53.7) | 35 (94.6) | 17 (100) | 52 (96.3) |
Nurse: nurse; Doc: doctor.
Most NS stated that the environment, at 69.1% compared with 38.9% of the MP (p=.03) and the condition of the patient, at 74.4% and47.1% (p=.04), respectively, could intimidate minors regardless of their age range (Table 2).
Over half of the CT were of the opinion that a risk of infection could exist both for the minor (75% NS and 55.6% MP) and for the patient (55% NS and 50% MP), although no statistically significant differences were found between the two populations studied (Table 2).
45% of the NS and 55.6% of the MP considered that not allowing visits could result in psychological trauma for the minor.
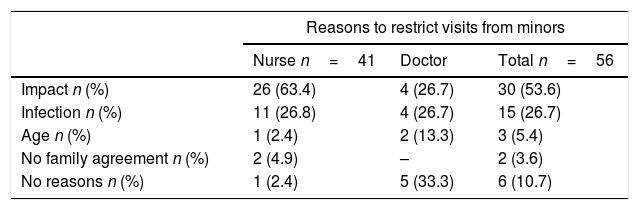
With reference to the two existing open-ended questions on the questionnaire, regarding the reasons for restricting and permitting visits from minors, 91.8% of respondents answered the first and 86.9%, the second. The impact and risk of infection were the main reasons for restriction and the reason for permission were family agreement or risk of the patient's death (Table 4).
Responses to the open-ended questions about the reasons to restrict or permit visits from minors to the ICU.
| Reasons to restrict visits from minors | |||
|---|---|---|---|
| Nurse n=41 | Doctor | Total n=56 | |
| Impact n (%) | 26 (63.4) | 4 (26.7) | 30 (53.6) |
| Infection n (%) | 11 (26.8) | 4 (26.7) | 15 (26.7) |
| Age n (%) | 1 (2.4) | 2 (13.3) | 3 (5.4) |
| No family agreement n (%) | 2 (4.9) | – | 2 (3.6) |
| No reasons n (%) | 1 (2.4) | 5 (33.3) | 6 (10.7) |
| Reasons to allow visit from minors | |||
|---|---|---|---|
| Nurse n=38 | Doctor n=15 | Total n=53 | |
| Family agreement n (%) | 26 (68.4) | 10 (73.3) | 36 (69.8) |
| Patient is conscious n (%) | 3 (7.9) | – | 3 (5.7) |
| Death n (%) | 9 (23.9) | 4 (26.7) | 13 (24.5) |
Lastly, we should underline that no statistical use was made of the responses in the space for explanatory comments to the closed questions because they were repetitive of the same concept asked and due to the low level of compliance.
DiscussionOpen door visits in an ICU are considered a positive intervention to reduce the stress of the critically ill family member17,18 but despite belonging to the family group, children continue to be restricted regarding visits to adult ICUs, infringing thus on family needs.19
Care team with/without childrenNo statistically significant differences were found between allowing minors to visit and the CT having children, for both MP and NS. This fact was surprising since in a study undertaken with nurses from a medical–surgical ICU it was found that professionals with children had a more positive approach towards open door visits since this made them more emotionally involved with the families.20 However, this study did not explore the opinion of the staff to the visits of the minors. It is possible this circumstance is not so relevant and greater importance is attached to the fact that culturally speaking adults try to protect minors from stressful situations.21
Age of the minorAccording to the results obtained and in a similar manner to that described in the Knutson et al.15 study, age is an important reason given by the CT for not allowing entry into the ICU, particularly to minors under 7 years of age. However, if the child wishes to visit their relation and with previous preparation which, depending on age, may be undertaken before the visit, this may be beneficial. Separation from a loved one when the child is under 7, as reflected by the review undertaken by Clarke et al.,22 may be experienced as a punishment or loss of love and may lead to anxiety and rejection by the minor when the patient returns to life at home.
Curiously, the restrictions by the CT for those over 12 years of age are practically nonexistent, but according to the cognitive stages of development of the child by Piaget23 these are the children who most need this preparation to be able to confront the situation because they are able to perceive of the gravity of the moment, unlike those under 12 who have a more abstract thinking pattern.24
The NS, in contrast to the Knutsson et al.,15 study, is much less permissive than the MP regarding visits from minors. This could be a defence mechanism by the NS, to protect them from the demands or reactions of the children.17 In fact, Capellini et al.25 demonstrated that the hours with the greatest concetration of visitors were between 14.00 and 20.00h, when the medical staff was reduced and only those on duty were present, and it is during these hours that minors are outside school. As a result it is the NS whose presence is greatest and who are most in contact and share the greatest physical space with the families.
State/environment of the ICUThe ICU is a highly technical unit which could cause an impression on minors and adults. In fact, this was stated mainly by the CT.
Similarly, and as stated by the Knutsson et al.15 study, a high percentage of respondents believed that the patient's condition could be a reason not to allow visitors, possibly in an attempt to protect the minor. However, this reticence dropped in the specific case of an end-of-life patient, especially if the minor was aged between 13 and 17. Visiting the patient may be as important for the minors as for the adults to understand what is happening,4,24 to help them feel integrated within the family nucleus22 and to be able to say a final farewell if necessary.8,26
The experiences related by the children in the Kean et al.24 study, who visited a relation for the first time in an ICU, demonstrate the importance of preparing them prior to the visit and not letting their imagination run away with them because if the minor is prepared for the visit they do not have to experience fear.27
Boyer et al.14 demonstrated that creating a guide for minors could be a useful tool both for the family members and for the CT. There were therefore collaborations between the ICU staff and child specialists for planning these visits, differentiating between the therapeutic interventions to be followed depending on the age group of the minor and their cognitive development.8,14 These interventions may be as simple as using a comprehensible vocabulary, avoiding medical terminology, creating a peaceful atmosphere, helping them to visit outside the established hours, letting them take in toys or drawing materials and encouraging their participation in care, such as reading a story or covering the patient up.6,12
RelationshipDepending on the relationship between the minor and the patient in the ICU, it was found that the MP and the NS would be more permissive with the visit when there was a very close family tie, such as father/mother or sibling, and especially if the minor was between 0/6 years. However, restrictions became harder when the relationship of the minor towards the patient was for a close relation such as grandfather/grandmother, friend or other relation and especially in ages under 12 when only half and on many occasions less than half of the respondents would allow the minor to visit the grandparent or another family member. These days, as reflected in several studies,28,29 the grandparents may have a very close relationship with their grandchildren for employment reasons or after divorce procedures of the parents and it is therefore necessary for the CT to be aware of new family structures.
Risk of infectionSimilarly to other studies,15,30 over half of the respondents stated that another reason for not permitting visits from minors in an ICU is the risk of infection, both for the minor and for the patient.
This argument is not reflected in the literature, where visits for minors to adult ICUs was not associated with an increase in rates of infection as indicated by reviews undertaken by Flalk et al.31 and Hanley et al.12 Several guidelines such as the Prevention of Infection of Neutropenic Patients of the American Society of Haematology do not contain specifications relating to age.32,33
This justification by the CT may be more closely linked to giving a good reason to persuade the family and avoid discussions regarding the minor's request to visit, than an argument based on evidence.
When exploring the response to the open-ended questions and, similarly to the study carried out by Clarke et al.,22 a high percentage of CT would allow minors to visit provided there was a family agreement, and the first decision has to be taken by an adult who is in charge of and accompanies the child at all times during the visit.
The results of this study have their limitations, since certain caution should be taken when treating the opinion of the CT of a single ICU, which cannot be extrapolated to the population in general. Notwithstanding, it may provide us with an idea of the possible barriers expressed by the staff to this issue which is largely unexplored in the literature, and particularly the Spanish literature, and provide a useful tool to determine them.
ConclusionsBoth the MP and the NS accept minors visiting adult ICUs provided they are over 6 years of age. However, clear contradictions abound, since in special circumstances such as very close relationships, patients who are awake, or in end-of-life processes, the CT becomes open to the visit regardless of the age range.
The CT will mostly initiate the visit with a pre-agreement by the family, although they believe that the environment and the condition of the patient intimidate the minor. Another reason to limit the visit is the belief in the risk of infection for both minor and patient.
The NS is less permissive than the MP towards visits from minors.
The different points of view among the CT members show how complete this issue is and necessitates updating of knowledge of all people involved in the process, together with information and training of the staff to provide tools and be able to cope with visits from children in adult ICUs. It is therefore essential to develop protocols of action and determine their impact in future research projects.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Valls-Matarín J, Peradejordi-Torres RM, Calvet-González E, Jorge-Castillo A, Calvo-Alonso S, Sandalinas-Mulero I. Visita de los menores de edad en una unidad de cuidados intensivos. ¿Qué opina el personal sanitario? Enferm Intensiva. 2020;31:52–59.