To determine the predictive models that include the dimensions of burnout that are predictors for physical/mental health, and subjective/psychological wellbeing perceived in intensive care professionals; to analyse the relationships between burnout syndrome, health status and wellbeing experienced by these professionals; and to establish sociodemographic differences in the variables evaluated.
MethodA correlational and cross-sectional study was conducted. A total of 52 critical care professionals, mainly nurses, were recruited from an intensive care unit of Madrid. All participants were assessed with the questionnaires: Maslach Burnout Inventory-Human Services Survey, Short Form-12 Health Survey, Satisfaction With Life Scale, Positive and Negative Affect Schedule, and Psychological Well-Being Scales.
ResultsNo significant sociodemographic differences were found. High levels in the three burnout dimensions were associated with poor physical/mental health and subjective/psychological wellbeing. High scores in emotional exhaustion and depersonalisation, and low in personal accomplishment negatively predicted subjective and psychological well-being scales. The self-acceptance scale had the highest predictive validity. Emotional exhaustion was the only burnout dimension that negatively predicted physical and mental health.
ConclusionsHealth status and levels of subjective/psychological wellbeing can be negatively influenced by the burnout syndrome experienced by intensive care professionals. As a result, the implementation of programmes to prevent and treat this syndrome is needed. These preventive interventions can positively impact not only the health and wellbeing of these professionals, but can also improve their ability to practice effectively, improve healthcare quality and patient security, and reduce the economic costs of health institutions. It is therefore imperative to implement burnout preventive programmes for intensive care professionals from universities to health institutions.
Determinar los modelos predictivos que incluyan las dimensiones del burnout predictoras de la salud física/mental y del bienestar subjetivo/psicológico percibido en profesionales de intensivos; analizar las relaciones entre el síndrome de burnout, la salud y el bienestar percibido por dichos profesionales; y establecer las diferencias sociodemográficas en las variables evaluadas.
MétodoSe llevó a cabo un estudio correlacional de corte trasversal. Participaron un total de 52 profesionales de intensivos, principalmente enfermeras, de una unidad de cuidados intensivos de Madrid. Todos los participantes fueron evaluados mediante los cuestionarios Maslach Burnout Inventory-Human Services Survey, Short Form-12 Health Survey, Satisfaction With Life Scale, Positive and Negative Affect Schedule y Psychological Well-Being Scales.
ResultadosNo se encontraron diferencias sociodemográficas significativas. Los altos niveles en las tres dimensiones del burnout estuvieron asociados con una pobre salud física/mental y bienestar subjetivo/psicológico. Las altas puntuaciones en agotamiento emocional y despersonalización y bajas en realización personal predijeron negativamente las escalas del bienestar subjetivo y psicológico. La escala de autoaceptación obtuvo la mayor validez predictiva. El agotamiento emocional fue la única dimensión del burnout que predijo negativamente la salud física y mental.
ConclusionesLa salud y el bienestar pueden estar afectados negativamente por el síndrome de burnout de los profesionales de intensivos. Como resultado, es necesaria la implantación de programas para prevenir y tratar este síndrome. Estas intervenciones preventivas no solamente pueden influir positivamente en la salud y bienestar de estos profesionales, sino que también pueden mejorar la práctica clínica, la calidad de la atención y los cuidados prestados y la seguridad del paciente y reducir los costes económicos de las instituciones sanitarias. Por lo tanto, es imperativo implementar programas preventivos dirigidos a los profesionales de intensivos desde las universidades hasta las instituciones sanitarias.
Intensive care units are stressful working environments where there may be a probable development of burnout syndrome. This syndrome is associated with poor health and well-being of intensive care professionals.
Our study determined the dimensions of the burnout predictors of health and well-being perceived by intensive care professionals. High levels of emotional fatigue and de-personalisation and low levels of self-realisation were a negative prediction of subjective and psychological well-being. The three dimensions of burnout predicted self-acceptance with the highest validity. Emotional fatigue was the only dimension of burnout which negatively predicted physical and mental health.
Implications of the studyBurnout syndrome not only affects the health and well-being perceived by intensive care professionals. It also affects their daily clinical practice, the care and the safety provided for the critically ill patient and the financial costs of healthcare institutions. Interventions are therefore fundamental in the prevention and treatment of burnout syndrome in these professionals. The prevention of burnout should be advocated from universities to healthcare institutions.
Most healthcare professionals regularly face up to many stressful factors during their daily clinical practice and are constantly exposed to hostile working environments. Of these professionals, intensive care staff are faced with major stresses at work which have been extensively reported in the literature: high workloads; constant time-related pressures; high risks of developing negative emotional responses caused by the death and suffering of their critically ill patients; moral and spiritual problems related with ethnical issues; reduction of social support at work and uncertainty regarding the medical treatment of patients.1–6 In fact, many studies have shown that the intensive care units (ICUs) are stressful and hostile places to work in, with the most probable likelihood of its professionals developing burnout syndrome.1,7 Mealer8 showed that the estimated prevalence of burnout among nurses and doctors who work in ICU ranges between 25% and 80%. This author even showed that the severity of this syndrome among the intensive care professionals varied from intermediate to severe.8 Also, the high prevalence of this syndrome and the high risk of developing it among intensive care professionals may impact the quality of their clinical practice, the care they provide and even in their own health and well-being. As a result, the main American societies related to critically ill patient care have recently alerted the authorities regarding the serious problem this burnout syndrome constitutes for intensive care professionals and have consequently called for action and the necessary measures to be taken.1
Burnout syndrome is considered to be a negative response to chronic working stress. The professionals who suffer from this syndrome perceived of a continuous imbalance between their needs, values and the work they need to do.9 This syndrome has three principal dimensions.9 Emotional fatigue (feeling emotionally overwhelmed and exhausted by work), de-personalisation (an impersonal and impassive response towards those receiving the service, care, treatment or instruction) and lack of self-realisation (feeling limited in competence and not achieving goals or success at work).
Burnout syndrome also impacts different aspects of well-being perceived by health professionals. However, research on well-being (popularly known as happiness) has mainly been undertaken by two disciplines: medicine and psychology. From medicine, well-being has been identified with peoples’ health status, evaluated from their physical and mental dimensions. In general, physical and mental well-being is an individual's state that allows them to correctly carry out their somatic and psychic activity.10 In other words, being healthy. From psychology it is possible to point to the existence of two different traditions: the hedonic and the eudaimonic approach.11 The hedonic tradition defends pleasure (hedone) as the ultimate goal of human life. This conception has led to subjective well-being (SW), which contains the emotional responses people have, also called affects (affectionate component) and satisfaction with life (cognitive component).12 In other words, feeling good. The eudaimonic tradition considers well-being as a state of psychological plenitude and harmony which involves the development of virtues (eudaimonia). This concept has led to psychological well-being (PW), focusing the attention on the development of indicators of positive psychological functioning.13 In other words, functioning properly. According to the Ryff14 model the six PW indicators are: self-acceptance, positive relations with others, autonomy, environmental mastery, purpose in life and personal growth.
We should point out that, although burnout syndrome is not included in the DSM-515 as a mental disorder, it is considered a serious health problem since it may lead to negative physical, psychological and occupational consequences on an individual level.16 Salvagioni et al.’s16 recent systematic review concludes that burnout syndrome is an important predictor of physical consequences, such as respiratory problems, cardiac diseases, headaches, diabetes type 2, gastrointestinal problems, hypercholesterolemia, prolonged fatigue and musculoskeletal pain. Furthermore, burnout syndrome has a major impact on mental health and predicts symptoms of depression and anxiety, post-traumatic stress disorder, alcohol abuse, insomnia and even suicide ideation. Burnout syndrome may also have negative consequences on an occupational level of the professional, such as absenteeism, presenteeism, dissatisfaction with the job and employment demands. It should be noted that although all of these relations are two-directional, this type of study mainly identifies the temporary relationship between exposure (burnout syndrome) and outcomes (consequences).16
Different studies indicate that low levels of well-being are related to moderate or high levels of burnout syndrome in healthcare professionals. High levels of burnout are associated with a reduction in subjective well-being (low satisfaction with life, low positive affect and high negative affect).17,18 For its part, moderate levels in dimension of the burnout syndrome are related to low levels in the different scales of psychological well-being.19,20 As a result of these negative consequences, healthcare professionals may decide to abandon their profession.21,22
Burnout syndrome, physical/mental health and subjective/psychological well-being are interrelated. Most studies have demonstrated that burnout syndrome is related to poor health status and well-being. Although existing evidence is considerable and abundant in this field of research, to date no predictive models in intensive care professionals have been found to specify the dimensions of burnout that may predict the physical/mental health and subjective/psychological well-being perceived by these professionals.
The main aim of this study was to determine the predictive models that include burnout predictor dimensions of physical/mental health and subjective/psychological well-being perceived by intensive care professionals. Secondary study objectives were, on the one hand, to analyse the relationship between burnout syndrome, health status and well-being perceived by said professionals and on the other, assess the possible differences in the participant sample.
MethodDesignCross-sectional correlation study.
ScopeThe study was conducted in an ICU of a public hospital in the Autonomous Community of Madrid (Spain) during the month of June 2014. The participant ICU had 12 beds and mainly cared for postsurgical patients (principally general and digestive and emergency surgeries), critical cardiac patients (such as myocardial infarctions and cardiac arrests) and respiratory patients (such as pneumonias and chronic obstructive pulmonary diseases).
SubjectsAll intensive care professionals who worked in the participant ICU were included in the study (nurses, nurse's aides and doctors). The total estimated staff was 60 intensive care professionals. Professionals who were absent due to sick leave, holidays or unpaid leave during the data collection period were excluded.
Variables and tools of measurementBurnout syndromeThis syndrome was assessed using the Maslach Burnout Inventory-Human Services Survey (MBI-HSS).9 This questionnaire particularly assesses burnout syndrome in healthcare professionals. The MBI-HSS consists of 22 items and 3 subscales for each dimension of the syndrome: 9 items assess emotional fatigue, 5 assess de-personalisation and 8 items assess self-realisation. Response to the questionnaire items use a Likert type scale of 7 points (from 0=“never” to 6=“daily”). High scores in emotional fatigue and de-personalisation and low scores in self-realisation demonstrate the presence of burnout syndrome. The reliability of the MBI-HSS was evidenced by the obtainment of Cronbach's α coefficients ranging between .72 and .90 for each subscale, both in the original version9 and its adaptation into Spanish.23
Health statusThe Health Survey Short Form-12 (SF-12)24 questionnaire was used to assess physical and mental health. The SF-12 is considered to be a genetic and subjective measurement of subjective health status, and consists of 12 items (6 for the physical and mental components) with different forms of response. Cronbach's α coefficients for each health component varied from .73 to .89 in the original version24 and in the Spanish versión.25
Subjective well-beingThe cognitive component of SW was assessed using the Satisfaction With Life Scale.26 This scale consists of 5 items with a Likert type response of 7 points (from 1=“no, absolutely not” to 7=“totally”). The highest scores reflect higher levels of satisfaction with life. The Spanish version of the Satisfaction With Life Scale27 obtained a reliability coefficient similar to that of the original version26 (Cronbach's α coefficient=.87). The affect component of SW was assessed using the Positive and Negative Affect Schedule8 questionnaire. This questionnaire contains 20 items (10 items for each type of affection, positive and negative). The Positive and Negative Affect Schedule has a Likert type response scale of 5 points (from 1=“not at all or almost never” to 5=“very much”). The affect balance is determined by the difference between both affects. Cronbach's α coefficients for each affect range from .84 to.90 both in its original28 and in the Spanish verison.29
Psychological well-beingThe Psychological Well-Being Scales14 is the most commonly used questionnaire internationally to assess the six indicators of PW: self-acceptance, positive relations with others, autonomy, environmental mastery, purpose in life and personal growth. The Psychological Well-Being Scales consists of 29 items (from 4 to 6 for each indicator) for which scores are given on a Likert type scale of 6 points (from 1=“totally disagree” to 6=“totally agree”). High scores on all scales indicate positive functioning. Cronbach's α coefficients for each indicator vary from .70 to .84 in the original versión.14 These values are similar to those obtained in the adapted Spanish version.30
Data collectionFirstly, approval was obtained from the ethics committee of the hospital where the study was conducted. All participants received written information about the nature and proposal of the study and signed an informed consent form. Prior to this, the main study researcher had met with the registrar and nursing supervisor of the participating ICU. The purpose of this meeting was to obtain their support for the distribution of the questionnaire among the intensive care professionals. A meeting was also called to inform all of them of the study. Posters with information about the study were also exhibited in the rest area and in the nurse's station of the participant ICU. All the self-completion questionnaires were contained in a file that all the participants had to complete and deposit within three weeks in a collecting box in the rest area. All the questionnaires began with a few brief initial recommendations on how to respond appropriately to the questions. The consent form was contained inside the questionnaire, together with a sheet for collecting sociodemographic participant data (sex, age, profession, experience in intensive care and type of contract). The main study researcher individually distributed the files to everyone on the intensive care staff. Participation was voluntary and all the participants anonymously completed the questionnaires during working hours. No one was obliged to complete them and all participants were able to withdraw from the study at any time.
Data analysisThe IBM SPSS Statistics™ v.21.0 for Windows (IBM Corp., Armonk, NY, U.S.A.) statistical package was used for data analysis. All statistical tests applied were bilateral (α=.05), and the statistical significance was therefore established at .05. Descriptive statistics were determined to analyse sociodemographic and psychological variables. Prior to correlation and regression analysis the sociodemographic differences on each psychological scale were assessed to ensure that the correlations and the predictive models obtained were adjusted to all the intensive care participant professionals. The differences in sex and type of contract were analysed using the Mann–Whitney U test. The differences in age, profession and experience in intensive care were assessed using the Kruskal–Wallis H test. Once it had been established that there were no existing differences in any sociodemographic variable and that the total sample was of normal distribution, posterior analyses were performed. Firstly, the correlation analysis between all the psychological variables assessed using the Pearson (r) correlation coefficient was performed. After this and based on the previous analysis, the corresponding multiple lineal regression analyses were performed and the method of successive steps to obtain possible predictive models. Prior to the production of these models, we verified the necessary requisites to be complied with for the regression analysis in the total sample (such as multivariate normality, multicolinearity and homoscedasticity). Due to the regression analysis being repeated 11 times (once for each health scale and once for each subjective well-being scale), the Bonferroni correction was applied to control statistical multiplicity. By applying this correction only the predictive models were accepted which did not exceed a predetermined critical p value (p value/number of predictive models tested=.05/11=.0045). Finally, after the previous regression analysis the burnout syndrome dimensions predicted by physical/mental health and subjective/psychological well-being were determined.
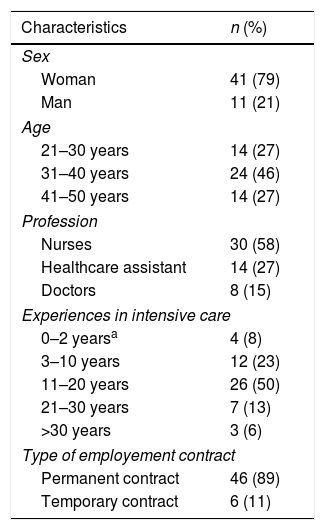
ResultsInitially 55 files were collected. However, three of them contained items which had not been responded to and we thus obtained a total of 52 valid files. The rate of response was 86.7%. Most of the sample comprised nurses, since they formed over half of the participants (n=30; 57.7%). The remainder of the sample were represented by 14 nurse's aides (26.9%) and 8 doctors (15.4%). The majority of participants were women (n=41; 78.8%). The age of the intensive care professional ranged mostly between 31 and 40 years (n=24; 46%), with the minimum age being 23 years and the maximum 50 years (M=36.64; SD=7.05). Their experience in intensive care units mainly ranged between 11 and 20 years (n=26; 50%), with minimum experience being 1 year and maximum 31 years (M=14, 72; SD=7.08). With regard to the type of contract, most intensive care staff had a permanent contract in the participant ICU (n=46; 88.5%). Table 1 shows the sociodemographic data of the study sample.
Demographic characteristics of the intensive care professionals (n=52).
| Characteristics | n (%) |
|---|---|
| Sex | |
| Woman | 41 (79) |
| Man | 11 (21) |
| Age | |
| 21–30 years | 14 (27) |
| 31–40 years | 24 (46) |
| 41–50 years | 14 (27) |
| Profession | |
| Nurses | 30 (58) |
| Healthcare assistant | 14 (27) |
| Doctors | 8 (15) |
| Experiences in intensive care | |
| 0–2 yearsa | 4 (8) |
| 3–10 years | 12 (23) |
| 11–20 years | 26 (50) |
| 21–30 years | 7 (13) |
| >30 years | 3 (6) |
| Type of employement contract | |
| Permanent contract | 46 (89) |
| Temporary contract | 6 (11) |
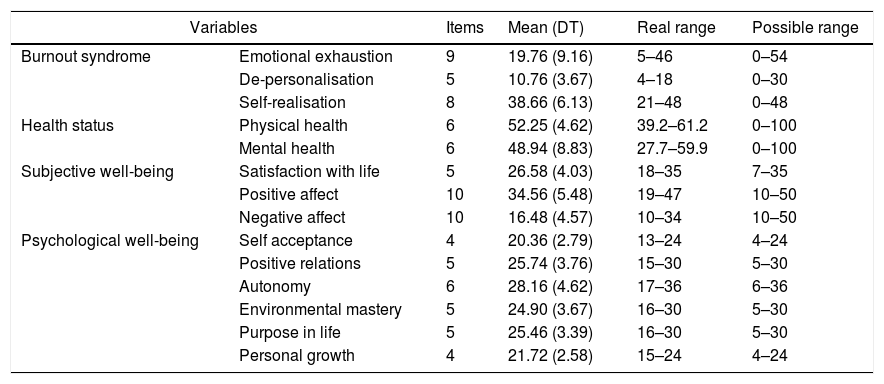
In keeping with the cut-off points of the MBI-HSS included in the questionnaire manual mean scores obtained in the three dimensions of burnout by the total sample were means: the mean score in emotional fatigue was between 16 and 27, that of de-personalisation was between 7 and 12 and that of self-realisation between 32 and 38. Table 2 contains the descriptive statistics obtained in the psychological variables assessed.
Descriptive statistics of the psychological variables analysed in intensive care professionals (n=52).
| Variables | Items | Mean (DT) | Real range | Possible range | |
|---|---|---|---|---|---|
| Burnout syndrome | Emotional exhaustion | 9 | 19.76 (9.16) | 5–46 | 0–54 |
| De-personalisation | 5 | 10.76 (3.67) | 4–18 | 0–30 | |
| Self-realisation | 8 | 38.66 (6.13) | 21–48 | 0–48 | |
| Health status | Physical health | 6 | 52.25 (4.62) | 39.2–61.2 | 0–100 |
| Mental health | 6 | 48.94 (8.83) | 27.7–59.9 | 0–100 | |
| Subjective well-being | Satisfaction with life | 5 | 26.58 (4.03) | 18–35 | 7–35 |
| Positive affect | 10 | 34.56 (5.48) | 19–47 | 10–50 | |
| Negative affect | 10 | 16.48 (4.57) | 10–34 | 10–50 | |
| Psychological well-being | Self acceptance | 4 | 20.36 (2.79) | 13–24 | 4–24 |
| Positive relations | 5 | 25.74 (3.76) | 15–30 | 5–30 | |
| Autonomy | 6 | 28.16 (4.62) | 17–36 | 6–36 | |
| Environmental mastery | 5 | 24.90 (3.67) | 16–30 | 5–30 | |
| Purpose in life | 5 | 25.46 (3.39) | 16–30 | 5–30 | |
| Personal growth | 4 | 21.72 (2.58) | 15–24 | 4–24 | |
Scores in emotional fatigue: ≥27 (high), 26–17 (medium), ≤16 (low). Scores in de-personalisation: ≥13 (high), 12–7 (medium), ≤6 (low). Scores in self-realisation: ≥39 (high), 38–32 (medium), ≤31 (low). High scores in emotional fatigue and de-personalisation imply poorer psychological functioning, whilst high scores in the remainder of psychological variables implies better psychological functioning.
None of the statistical tests for differential analysis indicated that the sociodemographic variables had any impact on the scores obtained in the burnout syndrome, in the physical/mental health or in the subjective/psychological well-being perceived by the intensive care professionals.
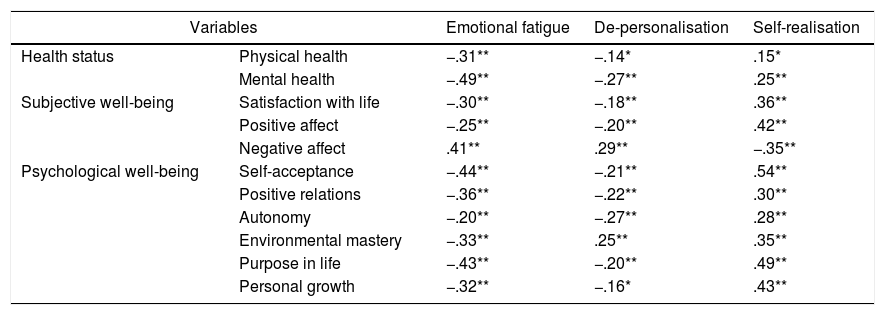
The correlations between physical/mental health and subjective/psychological well-being with the burnout syndrome is contained in Table 3. All the psychological variables assessed were associated (Pearson correlation coefficients between −.14 and .54). However, physical health obtained its lowest correlations with de-personalisation (r=−.14) and self-realisation (r=.15). Correlation analysis showed that both emotional fatigue and de-personalisation were negatively related with physical/mental health and with subjective/psychological well-being. In contrast self-realisation was positively associated with the previous variables. The only exception was the positive relationship of negative affect with emotional fatigue and de-personalisation and the negative relationship of this variable with self-realisation.
Correlations between physical/mental health, Subjective/psychological well-being and the three dimensions of burnout in the intensive care professionals (n=52).
| Variables | Emotional fatigue | De-personalisation | Self-realisation | |
|---|---|---|---|---|
| Health status | Physical health | −.31** | −.14* | .15* |
| Mental health | −.49** | −.27** | .25** | |
| Subjective well-being | Satisfaction with life | −.30** | −.18** | .36** |
| Positive affect | −.25** | −.20** | .42** | |
| Negative affect | .41** | .29** | −.35** | |
| Psychological well-being | Self-acceptance | −.44** | −.21** | .54** |
| Positive relations | −.36** | −.22** | .30** | |
| Autonomy | −.20** | −.27** | .28** | |
| Environmental mastery | −.33** | .25** | .35** | |
| Purpose in life | −.43** | −.20** | .49** | |
| Personal growth | −.32** | −.16* | .43** | |
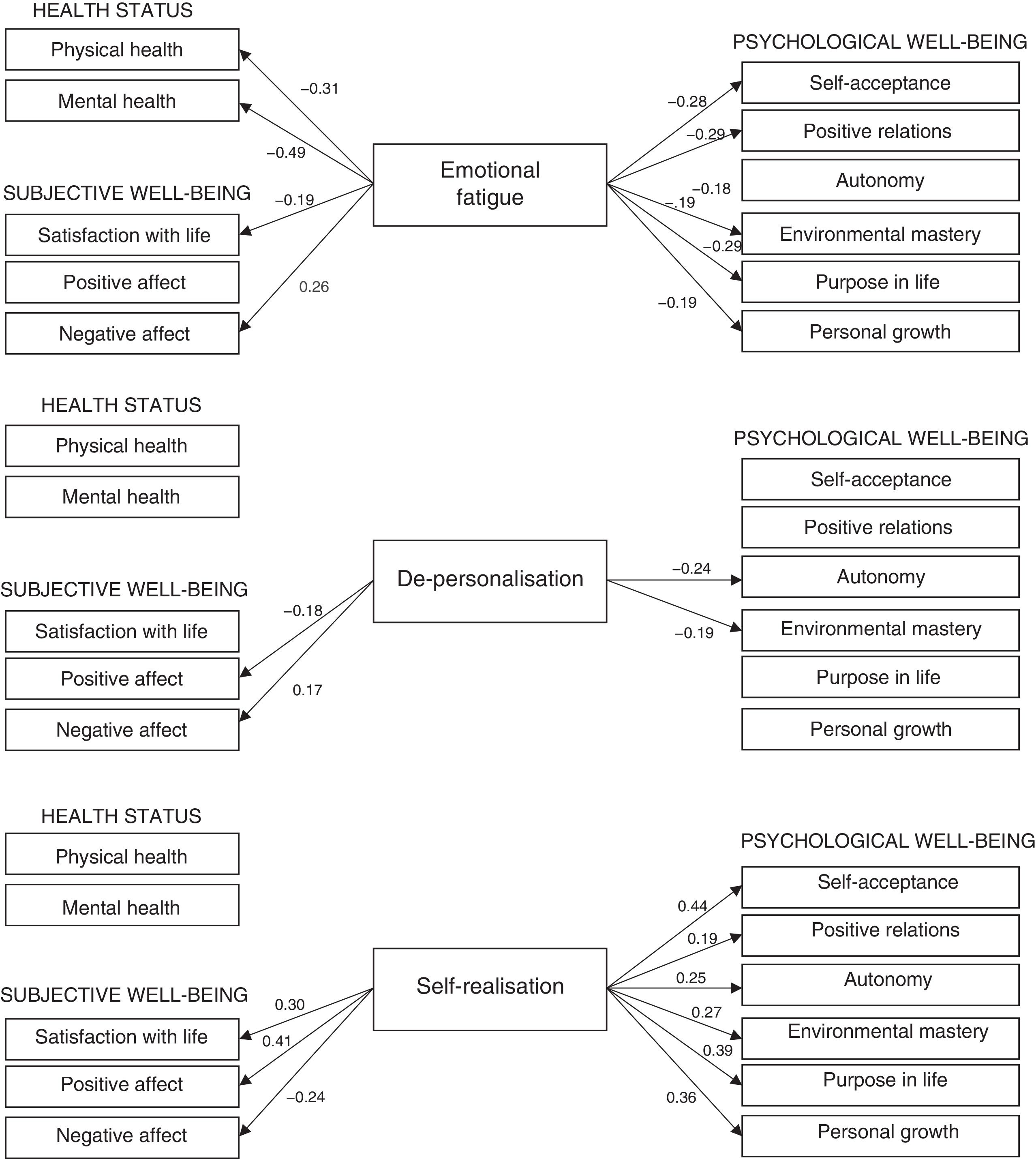
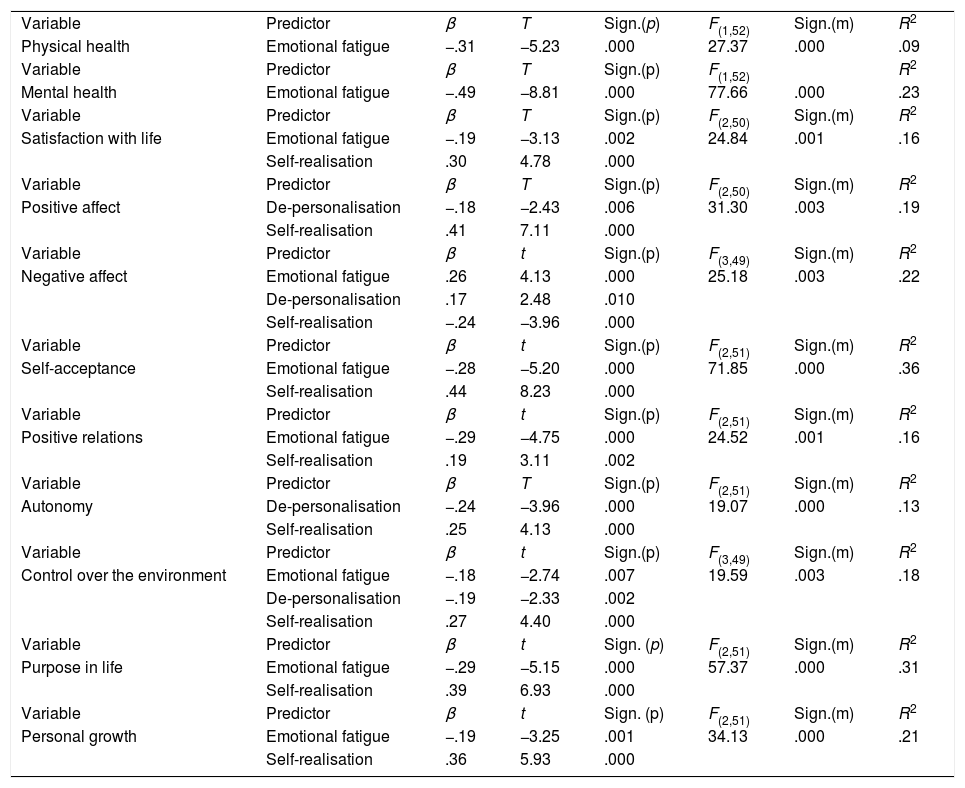
The predictive models obtained are contained in Table 4. As may be observed, no p value exceeded this critically predetermined p value (p=.0045). Thus, the results from regression analysis showed that emotional fatigue was the only dimension of the burnout syndrome which predicted physical health (β=−.31) and mental health (β=−.49). Also, emotional fatigue positively predicted negative affect (β=.26), and negatively satisfaction with life (β=−.19) and all the psychological well-being indicators (the standardised coefficients β ranged between −.19 and −.29), except autonomy. Regarding de-personalisation, this only negatively predicted the positive affect (β=−.18), autonomy (β=−.24) and environmental mastery (β=−.19). This burnout dimension also positively predicted negative affect (β=.17). With regard to self-realisation, this positively predicted all the scales of subjective and psychological well-being (standardised coefficients β between .19 and .44). The only exception was the negative prediction of this dimension of burnout on the negative affect (β=−.24). Finally, the predictive model of physical health obtained the lower explained variance (R2=.09), whilst the predictive model of self-acceptance obtained the higher value (R2=.36). Standardised regression coefficients (β) associated with each dimension of burnout predicted are graphically presented in Fig. 1.
Dimensions of burnout predictors of physical/mental health of the subjective/psychological well-being perceived by the intensive care professionals (n=52).
| Variable | Predictor | β | T | Sign.(p) | F(1,52) | Sign.(m) | R2 |
| Physical health | Emotional fatigue | −.31 | −5.23 | .000 | 27.37 | .000 | .09 |
| Variable | Predictor | β | T | Sign.(p) | F(1,52) | R2 | |
| Mental health | Emotional fatigue | −.49 | −8.81 | .000 | 77.66 | .000 | .23 |
| Variable | Predictor | β | T | Sign.(p) | F(2,50) | Sign.(m) | R2 |
| Satisfaction with life | Emotional fatigue | −.19 | −3.13 | .002 | 24.84 | .001 | .16 |
| Self-realisation | .30 | 4.78 | .000 | ||||
| Variable | Predictor | β | T | Sign.(p) | F(2,50) | Sign.(m) | R2 |
| Positive affect | De-personalisation | −.18 | −2.43 | .006 | 31.30 | .003 | .19 |
| Self-realisation | .41 | 7.11 | .000 | ||||
| Variable | Predictor | β | t | Sign.(p) | F(3,49) | Sign.(m) | R2 |
| Negative affect | Emotional fatigue | .26 | 4.13 | .000 | 25.18 | .003 | .22 |
| De-personalisation | .17 | 2.48 | .010 | ||||
| Self-realisation | −.24 | −3.96 | .000 | ||||
| Variable | Predictor | β | t | Sign.(p) | F(2,51) | Sign.(m) | R2 |
| Self-acceptance | Emotional fatigue | −.28 | −5.20 | .000 | 71.85 | .000 | .36 |
| Self-realisation | .44 | 8.23 | .000 | ||||
| Variable | Predictor | β | t | Sign.(p) | F(2,51) | Sign.(m) | R2 |
| Positive relations | Emotional fatigue | −.29 | −4.75 | .000 | 24.52 | .001 | .16 |
| Self-realisation | .19 | 3.11 | .002 | ||||
| Variable | Predictor | β | T | Sign.(p) | F(2,51) | Sign.(m) | R2 |
| Autonomy | De-personalisation | −.24 | −3.96 | .000 | 19.07 | .000 | .13 |
| Self-realisation | .25 | 4.13 | .000 | ||||
| Variable | Predictor | β | t | Sign.(p) | F(3,49) | Sign.(m) | R2 |
| Control over the environment | Emotional fatigue | −.18 | −2.74 | .007 | 19.59 | .003 | .18 |
| De-personalisation | −.19 | −2.33 | .002 | ||||
| Self-realisation | .27 | 4.40 | .000 | ||||
| Variable | Predictor | β | t | Sign. (p) | F(2,51) | Sign.(m) | R2 |
| Purpose in life | Emotional fatigue | −.29 | −5.15 | .000 | 57.37 | .000 | .31 |
| Self-realisation | .39 | 6.93 | .000 | ||||
| Variable | Predictor | β | t | Sign. (p) | F(2,51) | Sign.(m) | R2 |
| Personal growth | Emotional fatigue | −.19 | −3.25 | .001 | 34.13 | .000 | .21 |
| Self-realisation | .36 | 5.93 | .000 |
β: standardised regression coefficients; F(df,s-df): F(degress of freedom, sample size-degrees of freedom) statistic; R2: R squared statistic; Sign.(m): significance of the predictive model, Sign.(p): significance of the predictor; t: t statistic.
Our results confirm that the physical/mental health status and levels of subjective/psychological well-being may be negatively influenced by the burnout syndrome experienced by intensive care professionals.
The predictive models obtained show that each burnout dimension may have a negative impact on health and well-being.16–20,33 However, only emotional fatigue predicted physical health and mental health. This finding may be explained, due to the high levels in burnout being related to a poorer health status,16,33 whilst the levels obtained in our study in the three dimensions of the syndrome were intermediate. In contrast, the three dimensions of the burnout predicted subjective and psychological well-being which is why in our study this syndrome was mainly related to consequences on a psychological level. Here we should take into consideration previous research studies which have established that the burnout syndrome triggers mental illnesses, and may therefore really be considered as a mental disorder or dysfunction.33 Furthermore, emotional fatigue has been considered the first step in the development of the syndrome, mostly influencing health status negatively.34 But our results suggest that burnout syndrome appears to have greater predictive validity for the psychological well-being indicator of self-acceptance. In other words, it appears that this syndrome is of great importance in predicting the self-acceptance of the intensive care professional. Having positive attitudes towards oneself is an essential trait of positive psychological functioning and of people with a high level of self-acceptance, characterised by high self-esteem.35 As a result, an adverse environment in the ICU may mostly affect self-acceptance experienced by intensive care professionals and may impact other scales of subjective and psychological well-being. Potential interventions to reduce burnout syndrome in these professionals should therefore mainly aim at improving their levels of self-acceptance through the increase in their self-esteem.
Correlational analysis showed a moderate association between the burnout syndrome, health and well-being. These results were also consistent with previous studies which showed that burnout syndrome is linked to poorer physical/mental health and low levels of subjective/psychological well-being.16–20,33
All of these findings pinpoint the need to implement programmes for the prevention of the presentation and development of burnout syndrome and to treat it in intensive care professionals. In keeping with the recent official declaration of collaboration from the main critical care American societies,1 the potential strategies for the prevention of burnout in these professionals can be divided into two categories: (1) interventions focused on optimising the intensive care environment; and (2) interventions focused on helping people cope with their environment.
Regarding the ICU environment, the American Association of Critical-Care Nurses (AACCN) proposes six standards necessary for establishing a healthy work environment36: (1) appropriate communication, (2) authentic collaboration, (3) effective decision-taking, (4) appropriate numbers of staff, (5) significant occupational recognition, and (6) authentic leadership.
Regarding the interventions for facing up to an adverse environment in the ICU, the official declaration proposes1: (1) team interventions (e.g. periodical meetings with the whole team); (2) interventions focused on the professional (e.g. training in stress reduction), and (3) interventions to mitigate risk factors (e.g. consultations on ethics).
Furthermore, our results also suggest that high levels of emotional fatigue are associated with low levels of physical health. Interventions are therefore needed to help doctors and nurses improve their habits to improve their physical health (e.g. exercise, healthy diet and adequate sleep), thus helping them to reduce the adverse effects of the burnout.
With regard to the absence of differences in sociodemographic variables, and given the small size of the sample, this finding must be considered with caution. Other studies that included larger samples have found results to be different. For example, it has been found that the younger intensive care nurses have a higher risk of developing burnout syndrome.6
With respect to study limits, the most important limit refers to possible suppositions regarding causality. We have to consider that the design used did not permit the establishment of causal relationships. Another major limitation was the small sample size. As already mentioned, the absence of differences between the sociodemographic variables may have resulted in a low statistical power. We believe that we would only have found significant differences in these variables in our study if they had been very marked. However, although the ICU selected fulfilled the Spanish standards and recommendations37 and the multiple lineal regression analysis met with the necessary sample size requisites (as a minimum of between 10 to 15 observations per predictor38), the generalisation of the predictive models obtained has to be considered with caution and further studies need to be conducted with larger samples. Regarding the self-completion questionnaires used, their greatest limitation is the possible statistical biases that may be mostly caused by the social desirability bias. In this sense, medical tests could be performed to determine the health status of participants. Unfortunately, although these tests are objective, they are rather costly. However, we must take in to account that all the questionnaires used in our study had a high reliability and validity which was widely documented by numerous international studies. In view of the previous limitations, future research studies should confirm the negative impact of the three dimensions of the burnout syndrome in the health status and the well-being perceived by the intensive care professionals.
Finally, we consider that our results have significant implications for the clinical practice of intensive care personnel. The prevention of burnout syndrome is important for improving the health status and well-being of intensive care professionals but it is also important for optimising their daily clinical practice. Burnout syndrome may also lead to a reduction in efficaciousness and poor output in the workplace, which could have a direct effect on the attention, care and safety of the patient.1 In intensive care professionals this syndrome has been linked with lower patient satisfaction, higher rates of healthcare-associated infections, poorer quality of healthcare offered, higher rates of mortality after 30 days since admission and a higher number of medical errors.39–41 Furthermore, better clinical practice on an individual level could result in a better ICU environment1,36 and consequently, a lower number of burned out intensive care professionals. Healthcare institutions are also faced with problems related to burnout syndrome, such as the increase in absenteeism, too high a rotation of healthcare personnel and even the decision by some healthcare professionals to abandon the profession.21,22 As a result, the intervention programmes for preventing and treating this syndrome may have positive impact on the health and well-being of the intensive care professionals, improving their daily clinical practice and reducing the financial costs of healthcare institutions.
ConclusionsPhysical/mental health and subjective/psychological well-being may be negatively impacted by the burnout syndrome in intensive care professional's experience. Health and well-being perceived by these professionals have considerable implications on their daily clinical practice, and interventions to prevent and treat burnout are therefore necessary. These interventions must first treat the intensive care professionals who experience high levels of emotional fatigue and de-personalisation, and low levels of self-realisation. These preventative interventions and treatment would be beneficial for the daily clinical practice of these professionals, the quality of care and safety for the patient and for the healthcare institutions. These interventions could even be beneficial for medical and nursing students before they experience the adverse effects of burnout syndrome. Bearing in mind the results obtained in the psychological tests applied in this study, if burnout syndrome perceived by the intensive care professionals had been prevented or reduced using the before-mentioned interventions, the levels of health and well-being perceived by those professionals would have been higher. Universities and healthcare institutions must therefore promote the prevention of burnout. The implementation of initiatives such as the project HU-CI42,43 in Spain (http://humanizandoloscuidadosintensivos.com/es/inicio/), which is increasingly spreading to other countries may have a positive impact on the prevention of burnout, reducing its appearance and incidence and improving its management and control by intensive care professionals.
Ethical responsibilitiesApproval was obtained from the corresponding ethical committee (ref. nr. EC508) of the hospital where the study was conducted. All participants received written information regarding the nature and proposal of the study and gave their informed consent.
Authorship/collaborating authorsBoth authors were responsible for the preparation of the manuscript. Eva G. Aparicio-Zaldívar was also responsible for collecting data in the intensive care unit participants.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to express their gratitude for the participation and valuable information given by the 52 intensive care professional participants.
Please cite this article as: Arrogante O, Aparicio-Zaldivar EG. Síndrome de burnout en los profesionales de cuidados intensivos: relaciones con la salud y el bienestar. Enferm Intensiva. 2020;31:60–70.