Delirium is cognitive impairment related to negative inpatient outcomes in the Intensive Care Unit (ICU), family interventions have been shown to be effective in reducing the incidence of this condition.
ObjectiveTo identify strategies that include the family in the prevention of delirium in the adult intensive care unit that can be integrated into ABCDEF. Inclusion criteria: Studies describing actions and interventions involving caregivers and family members in the ICU for the prevention of delirium, conducted in the last five years, available in full text, in English and Spanish, Portuguese and in adults.
MethodsA scope review was conducted using the keywords “Critical Care, Delirium, Family, Primary Prevention” in 11 databases (PubMed, Virtual Health Library, Cochrane Library, TRIP Data base, EBSCO, Ovid Nursing, Springer, Scopus, Dialnet, Scielo, Lilacs) and other sources (Open Gray, Google Scholar), between August - October 2019; 8 studies were considered relevant and were analysed.
ResultsThe results were described in 3 categories: flexibility vs. restriction of visits in the ICU, Reorientation as a prevention strategy and post-ICU syndrome in the family.
ConclusionExtended visits, development of family-mediated activities, and redirection are non-pharmacological strategies that reduce the incidence of delirium in the ICU and offer multiple benefits to the patient and family/caregiver.
El delirium es una alteración cognitiva relacionada con resultados negativos en el paciente interno en la unidad de cuidados intensivos (UCI), las intervenciones familiares han demostrado ser efectivas para reducir la incidencia de esta condición.
ObjetivoIdentificar las estrategias que incluyen a la familia en la prevención del delirium en la UCI del adulto que pueden ser integradas al ABCDEF. Criterios de inclusión: Estudios que describieran acciones e intervenciones que incluyan a cuidadores y familiares en la UCI para la prevención del delirium en adultos, realizados en los últimos 5 años, disponibles en texto completo, en español, portugués e inglés.
MétodosSe realizó una revisión de alcance utilizando las palabras clave «Critical Care, Delirium, Family, Primary Prevention» en 11 bases de datos (PubMed, Biblioteca Virtual de Salud, Cochrane Library, TRIP Data base, EBSCO, Ovid Nursing, Springer, Scopus, Dialnet, Scielo, Lilacs) y otras fuentes (Open Gray, Google Scholar), entre los meses de agosto-octubre de 2019; 8 estudios se consideraron relevantes y fueron analizados.
ResultadosLos resultados fueron descritos en 3 categorías: flexibilidad vs. restricción de visitas en la UCI, reorientación como estrategia de prevención y síndrome post-UCI en la familia.
ConclusiónLas visitas extendidas, el desarrollo de actividades mediadas por la familia y la reorientación son estrategias no farmacológicas que reducen la incidencia del delirium en la UCI y ofrecen múltiples beneficios para el paciente y su familiar/cuidador.
Delirium is considered as an altered or disturbed state of consciousness evidenced by a disorganised change in the patient's cognition (content) and perception (level); it has a sudden onset that varies between hours or days, behaves in a fluctuating manner and prevents the patient from receiving, processing, storing and remembering information correctly.1,2 It is considered a significant and independent aspect associated with poor prognostics for the critically ill patient3 such as : longer duration of hospital stay,4,5 high mortality rates,6–8 readmittance into the intensive care unit (ICU),9 cognitive impairment10 and long term functional impairment.11,12
The characteristics of delirium are difficult to observe in settings such as the ICU and its severity varies between patients. Delirium has been classified into 3 types: hyperactive, characterised by agitation, anxiety and the desire to remove therapeutic devices; hypoactive where the patient is drowsy, withdrawn and does not respond well to stimuli, and mixed which consists in fluctuation between the 2 previous states.13–15 Furthermore, the rate of the delirium in the ICU is heterogeneous, this variation is related to the type of population studied, the tools of detection used and /or the interpretation of events; the literature reports incidences above 30% in mixed populations,8,16,17 and up to 80% in patients with mechanical ventilation.6,18
One strategy developed for the management of critically ill patients has demonstrated benefits for the management and prevention of delirium. A package of interventions was developed based on evidence which includes activities such as: A- evaluating, preventing and controlling pain, B- completing both SAT (spontaneous awakening trials) and SBT (spontaneous breathing trials) in mechanically ventilated patients when appropriate, C- appropriate choice of sedation and analgesia, D- vigilance of delirium using the evaluation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) and application of different non-pharmacological strategies for treatment, E- activation of early mobility over a continuum of protocolised mobility.19 These actions arise with the proposal to improve the directives of clinical practice which were being managed by the Pain, Agitation, Delirium (PAD)20 protocol. Implementation of this package has shown it can reduce up to 50% the probability that patients suffer from some kind of episode of delirium.21
The family is a newly incorporated component of ICU inpatient care as part of the ABCDEF package for delirium prevention. The latest addition to this package was intervention F - patient and family involvement and engagement; it resulted from research development sponsored by the Gordon and Betty Moore.22 Studies have found that for every 10% increase in compliance with the "ABCDEF" package, patients had 2% more delirium-free days and a 15% greater chance of hospital survival.20 Recently, implementation of the strategy has been associated with reductions in the incidence of coma or delirium, time on mechanical ventilation, use of physical restraint, hospital mortality, ICU readmission and discharge to a non-home setting.23
According to the Society of Critical Care Medicine (SCCM) the F element requires patient-centred care where the needs of both the patient and the family member are respected and responded to through empowerment and participation, which provides an environment of safety related not only to physical but also to mental well-being as evidenced by assertive and timely communication between the professional and the family group; this element in addition to the benefits already mentioned for the patient, brings well-being for the family and improves the joint decision-making process, as well as the expectations regarding the care of the family member.24
Considering the impact that family actions can have on the prevention of delirium and the value placed on family involvement in the "ABCDEF" intervention package, it is important to review which strategies are most effective in developing positive patient outcomes. This scoping review aims to identify strategies that involve the family in the prevention of delirium in adult intensive care units that can be integrated into the ABCDEF.
Materials and methodsA scoping review was carried out using the 5 steps defined by Arskey and O’Malley25 as a framework: 1) Identification of the research question, 2) Identification of relevant studies, 3) Selection of studies, 4) Data analysis and 5) Collation, summarisation and reporting of results.
Search processThe databases consulted were PubMed, Virtual Health Library, Cochrane Library, TRIP Database, Ebsco, Ovid Nursing, Springer, Scopus, Dialnet, Scielo, Lilacs and other sources such as Open Gray and Google Scholar; during the months of August to October 2019.
For the search, keywords such as Delirium, Critical Care, Family, Primary prevention, Prevention and control were used in conjunction with the “AND” and “OR” operators, according to the particularities of each search engine; for example, for PubMed the search equation was "(((``prevention and control'' [Subheading] OR ``Primary Prevention''[Mesh]) AND ``Family''[Mesh]) AND ``Critical Care''[Mesh]) AND ``Delirium''[Mesh]'' while in the Virtual Health Library it was ``(tw: (Delirium)) AND (tw:(Critical care)) AND (tw:(Family)) AND (tw:(primary prevention)).''
The search was limited to studies in humans, published between 2014 and 2019, with texts in English, Portuguese and Spanish that had access to the full text. In the databases that allowed it, the search was limited by discipline to "Medicine" and "Public Health".
Inclusion criteriaWe included qualitative and quantitative studies conducted in the last 5 years, in the population over 18 years of age, describing actions and interventions that incorporate caregivers and family members in the ICU for the prevention of delirium, available in full text.
Exclusion criteriaStudies involving patients with a history of cognitive impairment, research with interventions that are also carried out by agents outside the family (health personnel) and whose outcome is not exclusively attributable to the actions of the family.
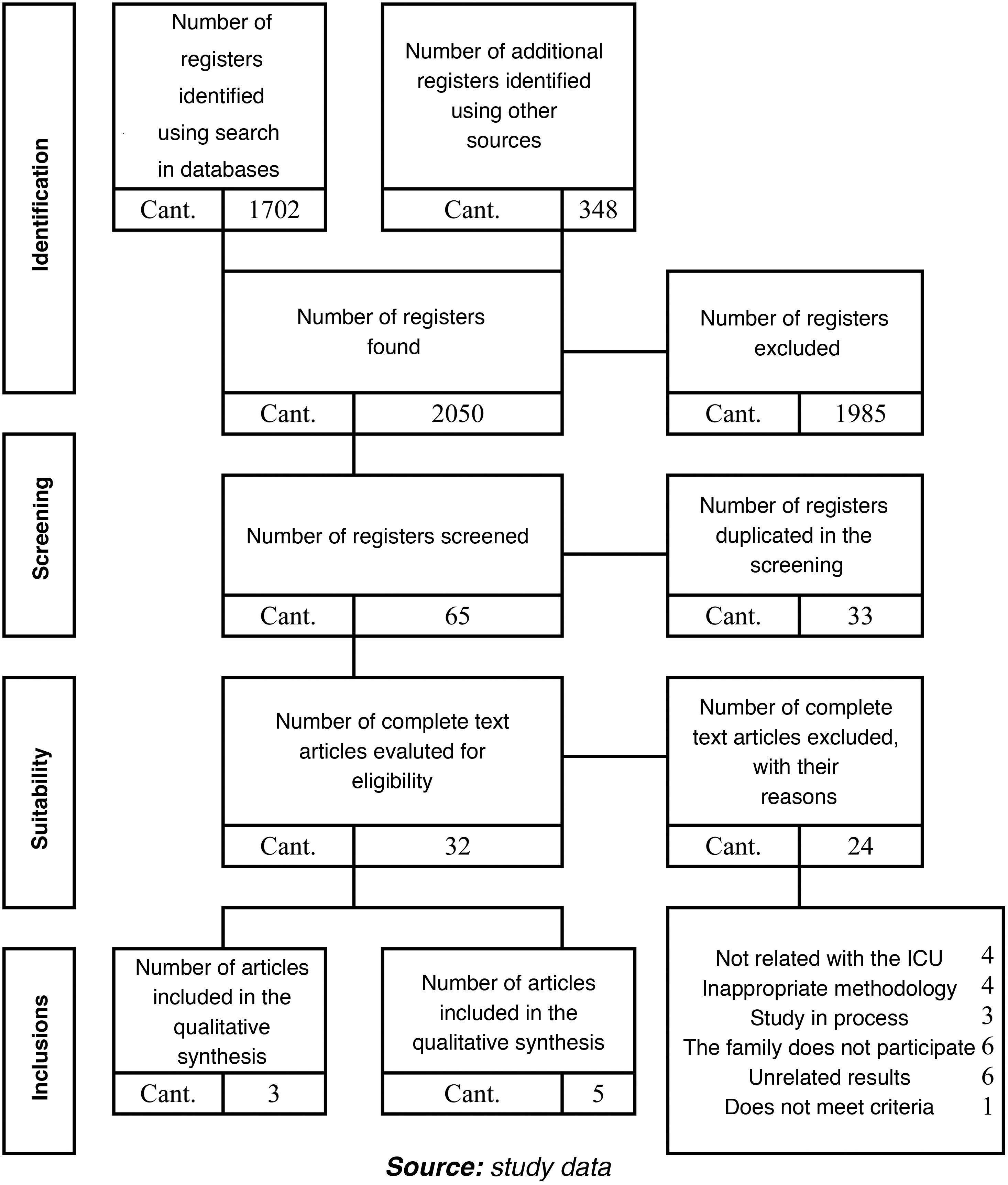
Selection and extraction processThe selection was carried out by two researchers who independently assessed each of the articles using the instruments of the proposed Spanish Critical Appraisal Skills Programme (CASPe).26 A total of 2,050 studies were selected by title; after reading the abstracts and main results, 65 articles were selected for full-text review. At the end of this process and by consensus of the researchers, 8 articles were selected to be included in the scoping review (Fig. 1). The determining factors assessed by each researcher for the selection of studies were objective, intervention, outcomes, and conclusions.
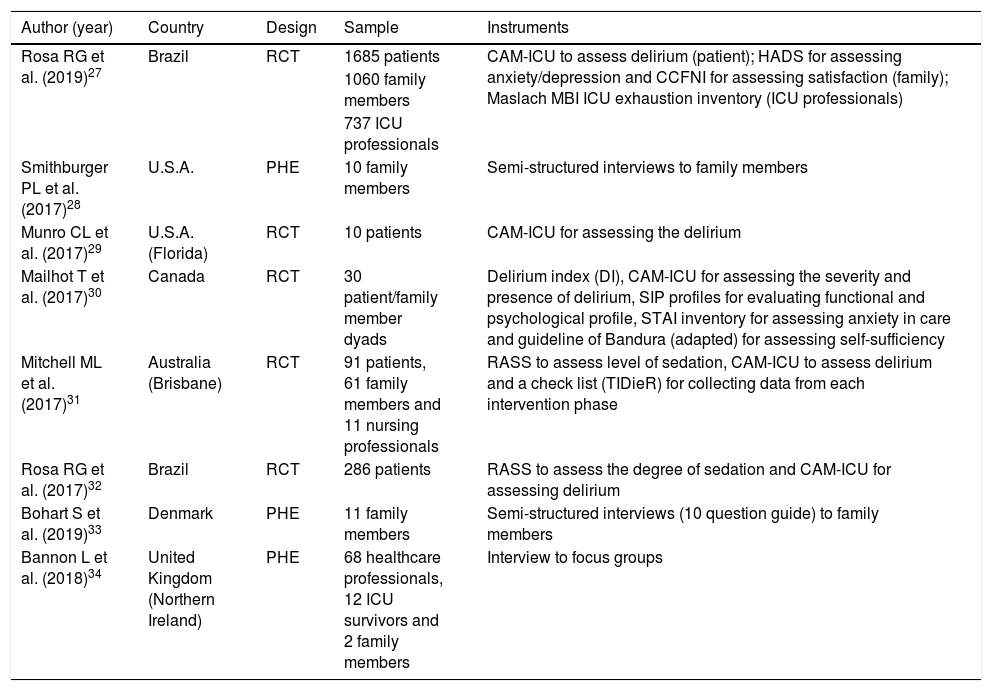
ResultsThis scoping review included 8 articles, 5 of which are quantitative studies and 3 are qualitative studies. The general characteristics of each are described in Table 1.
General description of the articles included in scoping review.
| Author (year) | Country | Design | Sample | Instruments |
|---|---|---|---|---|
| Rosa RG et al. (2019)27 | Brazil | RCT | 1685 patients | CAM-ICU to assess delirium (patient); HADS for assessing anxiety/depression and CCFNI for assessing satisfaction (family); Maslach MBI ICU exhaustion inventory (ICU professionals) |
| 1060 family members | ||||
| 737 ICU professionals | ||||
| Smithburger PL et al. (2017)28 | U.S.A. | PHE | 10 family members | Semi-structured interviews to family members |
| Munro CL et al. (2017)29 | U.S.A. (Florida) | RCT | 10 patients | CAM-ICU for assessing the delirium |
| Mailhot T et al. (2017)30 | Canada | RCT | 30 patient/family member dyads | Delirium index (DI), CAM-ICU for assessing the severity and presence of delirium, SIP profiles for evaluating functional and psychological profile, STAI inventory for assessing anxiety in care and guideline of Bandura (adapted) for assessing self-sufficiency |
| Mitchell ML et al. (2017)31 | Australia (Brisbane) | RCT | 91 patients, 61 family members and 11 nursing professionals | RASS to assess level of sedation, CAM-ICU to assess delirium and a check list (TIDieR) for collecting data from each intervention phase |
| Rosa RG et al. (2017)32 | Brazil | RCT | 286 patients | RASS to assess the degree of sedation and CAM-ICU for assessing delirium |
| Bohart S et al. (2019)33 | Denmark | PHE | 11 family members | Semi-structured interviews (10 question guide) to family members |
| Bannon L et al. (2018)34 | United Kingdom (Northern Ireland) | PHE | 68 healthcare professionals, 12 ICU survivors and 2 family members | Interview to focus groups |
CAM-ICU: Confusion Assessment Method for the ICU; CCFNI: Critical Care Family Needs Inventory; COH: cohorts; HADS: Hospital Anxiety and Depression Scale; PHE: phenomenological; RASS: Richmond Agitation-Sedation Scale; RCT: randomized clinical trial; SIP: Sickness Impact Profile; STAIS: State-Trait Anxiety Inventory; TIDieR: Template for Intervention Description and Replication.
Source: study data.
The search results were divided into 3 categories, which correspond to the common topics in the included studies; it should be clarified that 2 of them arise in response to the review question and detail possible interventions to be developed by a multidisciplinary team in the ICU setting, including under the framework of the ABCDEF strategy for the prevention of delirium; the last category corresponds to events reported by the literature as phenomena typical of relatives of patients hospitalised in the ICU, some as already described by the literature as "post-ICU syndrome".
Flexibility vs. Restriction of visits to the intensive care units in the prevention of deliriumOne of the strategies for the management of delirium that has gained momentum in recent years is the inclusion of the family in the care during the ICU stay, for which an increase in the number of family visiting hours has been proposed.35 Although no particular role has been defined for the family within the ICU, it has been shown that even without an intervention described in a protocol, the presence of the family member and their interaction with the patient can reduce the incidence of delirium and/or reduce the duration of delirium.36 This has led to the implementation of special regulations related to the openness of ICUs, with what is now known as "open door ICUs.35 One of the most frequent obstacles to the promotion of flexible visits is the perception of health professionals regarding the increase in infectious processes and workload, issues that have been debated in several studies.37,38
In the prospective before-and-after research conducted by Rosa et al. (2017) extended and restricted visit models (EVM and RVM, respectively) in a medical-surgical ICU in Porto Alegre (Brazil) were compared and their respective incidence of delirium, secondary outcomes included duration of delirium/coma, any ICU-acquired infection, ICU-acquired bloodstream infection, pneumonia and urinary tract infection, all-cause ICU mortality, and length of ICU stay. The MVE had a mean duration of 4.08 h visit versus the MVR with 2.21 h visit (p < 0.001). The sample consisted of 286 patients, who were allocated into 2 groups; 145 in the intervention group (IG) and 141 in the control group (GC). Patients in both groups received interventions according to the ABCDEF package, their relatives received orientation on ICU rules and good practices during the visit. Delirium was measured with the CAM-ICU once every shift by trained nurses. Results showed that the incidence of delirium was lower in the EVM; delirium occurred in 14 (9.6%) patients compared to the RVM with 29 (20.6%) patients, 95% CI: .50 (.26/.95); p = .03.32
Another study by Rosa et al. (2019) revisited the extended and restricted visit models, this time with a randomised clinical trial (RCT), in which 1,685 patients were recruited in 34 ICUs in Brazil (GI: 837, GC: 848); this study sought to measure, in addition to the incidence of delirium, the incidence of ICU-acquired infections, symptoms of anxiety and depression in the family, and burnout in ICU staff. The extended visit model had a mean of 4.8 h visit versus the restricted visit model with 1.4 h (adjusted difference: 3.4 h, 95% CI: 2.8-3.9; p < .001). Incidence of delirium was measured using the CAM-ICU, family anxiety and depression symptoms using the Hospital Anxiety and Depression Scale (HADS) and professional burnout using the Maslach Burnout Inventory-2. The extended visit included education for the family about the ICU environment, common procedures, multidisciplinary work, infection control, palliative care and delirium with supporting material (brochure and website), while the restricted visit maintained existing protocols. The investigators found that the decrease in the incidence of delirium was not significant; in GI: 18.9% (n = 157) of patients had delirium compared to GC where the incidence was 20.1% (n = 170) of patients, 95% CI: .92 (.73-1.15); p = .44. In contrast, this study reported that, the longer the interaction time with their relatives, patients had a 50% reduction in the duration of delirium, in the MVR the mean duration was 3.0 days versus 1.5 days for the MVE, 95% CI: .61 (.39-.97); p = .03.27
In the secondary outcomes for the 2 studies by Rosa et al. (2017, 2019) the reduction in ICU days of stay is not statistically significant and the variation in the mean is minimal. For the prospective study (2017) the mean number of days for ICU stay in the EVM was 3.0 (2.0-4.0) days and for the RVM 4.0 (2.0-0.6), 95% CI:0.89 0.79-.99); p = .04; while in the RCT (2019) the mean number of days was equal for both models 5 (3.0-8.0) days, 95% CI: -.02 (-.15/-.09); p = .59. Reported ICU mortality in the prospective study for EVM was 2.1% and in RVM 6.3%, 95% CI: .34 (.09-1.26); p = .10, while the RCT presents 14.8% for EVM and 14.4% for RVM, 95% CI: 1.01 (.77-1.32); p = .9. In relation to the acquisition of infections in the ICU setting, the 2 studies agree that EVM has a lower incidence 8 (5.5%) and 31 (3.7%) patients vs. RVM 13 (9.2%) and 38 (4.5%) patients.27,32
Qualitative research by Bannon et al. (2018) describes the perspectives of ICU staff, survivors and their families on the implementation of a package of interventions for the prevention of delirium in the ICU. The researchers conducted focus group interviews based on semi-structured questions in 12 ICUs in England, Scotland, Wales and Northern Ireland. Family members and ICU survivors talked about the extended visit model as a tool to facilitate the care provided between the team of professionals and them, which also allowed them to better develop some activities related to mobilisation and orientation; they found the extended visit model an efficient way to organise visits and thus avoid overwhelming the patient. The professionals, for their part, stated that the family is an under-utilised resource in the care of ICU patients; they consider that the family can make great contributions by making visits more flexible, although these should have a limit so that they do not interrupt the dynamics of the ICU and so that family members can return home and rest.34
Reorientation as a strategy for the prevention of deliriumReorientation through environmental modifications and the use of conventional objects has been a strategy used by health professionals in order to keep the patient's cognitive function stable, thus preventing delirium and its negative outcomes.39,40 Different visual and acoustic activities are used to stimulate the patient; through simple tasks such as mentioning the patient's name, repeating what day it is, where he/she is, recalling past events, providing guidance on the therapeutic devices around him/her and the reason for hospitalisation, the aim is to enable the patient to better interpret his/her environment in order to reduce the incidence of delirium during his/her stay in the ICU; the use of technological tools has made it possible to automate some of these tasks.41
A RCT developed by Munro et al. (2017) analysed a sample of 30 patients divided into 3 equal groups as follows: 20 of them received acoustic reorientation by means of hourly recordings for 8 h over 3 days; 10 patients with recordings developed by a stranger to the patient (RD) and 10 patients with recordings developed by family members (RF); the remaining 10 patients received usual care (GC). The researchers found that delirium-free days were highest in the RF group with 1.9 (.99) days, followed by the RD group with 1.6 (1.07) which did not differ from the GC: 1.6 (1.13); p = .043.29
Another type of intervention found in the literature is nurse-developed mentoring. Mailhot et al. (2017) conducted a pilot test for a randomised clinical trial with 30 patient/family dyads (GI: 16; GC: 14) GI: 16; GC: 14 where they sought to know the effectiveness of an educational intervention (tutoring/mentoring) to family caregivers called "MENTOR_D". This intervention was divided into 3 phases (pre-bedside, bedside and post-bedside) with a total duration of 60 min; the mentoring focused on the caregiver being able to distinguish the signs of delirium, communicate what they observe to the nurse, reorient the patient, talk about family memories, use clear and simple sentences, and keep the devices needed by their relative (glasses, hearing aids, etc.) in working order. Patient complications during delirium and length of hospital stay were taken from the medical record, the remaining data were collected manually; delirium was assessed from the CAM-ICU. This study found that the GI had better results regarding duration of delirium, with a mean of 1.94 (1.34) days compared to the GC with 4.14 (4.04) days. In terms of hospital stay, the GI obtained a significant reduction of almost 50%, with a mean of 6.30 (7) days compared to the GC with 12.10 (11.10) days; p < 0.34. Finally, in the assessment of delirium severity it was found that the GI presented lower values on days 1, 2 and 3; the GI obtained a mean of 10.56 (3.5), 5.38 (5.45) and 3.43 (4.96), respectively compared to the GC which obtained 12.7 (4.05), 8 (6.34) and 5.5 (7), respectively; p < .27.30
A cohort study developed by Mitchell et al. (2017) included 91 patients pre-randomisation (Pre-a): 30; GI: 29; GC: 32 to try to assess the feasibility of the design, recruitment and acceptability to family members and nurses of a family-delivered intervention to reduce delirium in ICU patients. The 3-element protocol included: sensory, orientation-memory and therapeutic engagement-cognitive stimulation. Activities to be performed by family members included orienting the patient to date, place, and space, remembering the name of treating professionals, discussing current family events, recalling events that occurred in the past and using sensory aids such as glasses and hearing aids when necessary; family members were educated and accompanied in the development of these activities and were asked to implement them at least once per visit. The researchers found that the days of presence of delirium were slightly lower in Pre-a 0.5 (2) days versus GC and GI with 1.0 (2) day in both groups; p = 0.06; while the prevalence of delirium exhibits similar dynamics in Pre-a 15 (50%) patients, in GI:17 (59%) and in GC: 18 (56%); p = .98.31
Similar interventions have been described in the qualitative approach. Smithburger et al. (2017) conducted a qualitative research study with 62 relatives of inpatients in an American ICU, where they sought to know the opinions of patients' relatives on active participation in delirium prevention interventions, for which they conducted semi-structured and in-depth interviews. Among their main findings they describe 3 themes: family presence, family/patient interaction and education about delirium. The first one "Consistent family presence and involvement in care" highlights the need for family members to "be there" for the patient, also expressing that they can help when needed with simple activities such as bathing for the patient's well-being or being a facilitator in including familiar objects and reorientation. The second and third themes of this study have communication at their core, these were called "Improving ease of interaction between family and patient" and "Delirium education for families"; here family members expressed that well-structured initial education, reinforced with reminders, could be helpful in improving reorientation processes; most focused this work on the nurse, as this was the "bedside" professional who told them what they were allowed to do and when (even for joint care).28
Post-ICU family syndrome (PICS-F)The process of illness and admission to the ICU is in itself an emotionally demanding event that affects not only the patient but also the caregivers and relatives. Events such as anxiety, depression,42,43 perceived overload, restriction of activities, complication of grief,44 dissatisfaction and even post-traumatic stress45 are described in the scientific literature as post-ICU family syndrome (PICS-F). These events have an impact on the family member's ability to provide attentive and optimal support to the surviving ICU patient and even on his or her personal life afterwards.
Risk factors for PICS-F include being female, having a low level of education, being younger than the patient or having a history of mental illness.44 During hospitalisation, a very important risk factor is the limited communication of the family/caregiver with the healthcare staff and even with the patient, as this increases fears, anxiety and uncertainty in both the patient and the family.45,46 Some authors state that the ABCDEF strategy should include additional elements for the prevention of PICS and PICS-F; F- should add to the family component the continuous updating of information (follow-up) and functional reconciliation, G- good communication management and H- information and education material.44,47
Research by Bohart et al. (2019) analysed the views of 11 family members of ICU inpatients to explore the experience of their loved one's delirium; the authors describe 3 categories "Delirium is not the main concern", "Communication with health professionals is crucial" and "Delirium affects family members".
In the first category, the participants explained their conception of delirium before witnessing it, most were unaware of this symptom or related it to withdrawal syndrome, but not to the ICU. Another point made was that delirium is an effect of pharmacological treatment, ventilator use and was even associated with fear, "delirium is seen as a natural consequence." Even so, for them the important thing was not the episodes of delirium but the survival of their loved one. In the second category, relatives expressed that the way in which health professionals communicate the presence and behaviour of delirium makes them think that it is not an entity to worry about, even saying that in the discussion with the health team the general state was clear but leaving "issues related to delirium unspoken." Some participants expressed needing more information about delirium, illnesses and treatments, while those who received information described feeling relieved, as it was easier to understand the changes their loved one was going through. Finally, it is described how family members are unable to recognise an episode of delirium for the first time; some noticed the patient behaving differently, ranging from bizarre to irritable, and one family member even noticed the patient as "absent", which led many of them to limit communication with their loved one to avoid making excessive demands or creating anxiety.33
In the previously mentioned RCT by Rosa et al. (2019) on flexible visiting hours, it was found in sensitivity analyses that the probability of presenting anxiety and depression were lower in the GI; clinical anxiety values were 13.4% in the GI vs. 28.2% in GC, with a prevalence ratio (PR): .48 (95% CI: .35-.66; p = .001); the percentage of depression was GI: 8.1% vs. GC: 17.7%; PR: .46 (95% CI: .28-.76; p = .001). As for satisfaction it was higher in GI, showing a mean of GI: 146.1 compared to GC: 132.6 (95% CI: 10.4-16.7; p < .001).27
The research by Mailhot et al. (2017), included within their secondary objectives to assess levels of family caregiver anxiety and sense of self-efficacy in patient care when implementing a nursing intervention involving family caregivers in the management of delirium after cardiac surgery. Results for days 4, 15 and 30 showed that family caregiver anxiety and self-efficacy were favourable in GI compared to GC (GC anxiety: D4: 43.86 [11.46], D15: 41 [9.22], D30: 37.42 [9.96] and GI: D4: 36.62 [7.36], D15: 36.69 [7.72], D30: 36.87 [11.43]; p = 0.21) (Self-efficacy GC: D4: 110.43 [16.87], D15: 112.58 [15.52], D30: 115.36 [15.81] e GI: D4: 124.25 [9.16], D15: 123.06 [7.05], D30: 124.93 [6.1]; p = .15), although not statistically significant within the ANCOVA model used in the analysis.30
DiscussionThis scoping review focused on identifying and describing strategies that involve the family in the prevention of delirium; the most frequently reported interventions focused on flexible visiting hours and reorientation of the ICU patient. The data from the different research studies included in this review allow us to infer that these interventions are useful in the ICU environment and favour the interaction of the family member with the patient in order to reduce the physical and mental sequelae after the discharge of the critically ill patient.
Ely (2017) explains that the management paradigm in the ICU has changed, with one of the main objectives in the units now being to decrease any possible negative iatrogenic effects on the patient and their family.22 Inoue et al. (2019) developed a literature review where they state that critically ill patients experience high levels of physical and psychological stress in the ICU.44 These experiences give rise to cognitive impairment and the appearance of post-traumatic stress symptoms that persist months or years after hospital discharge (PICS) and are associated with a deterioration in quality of life. They also report that during the first week after the patient's discharge the family presents similar symptoms in response to this same phenomenon, with the highest prevalence of anxiety (42-66%) and depression (14.5-66.7%) as manifestations of PICS-F.44 This is why in recent years there has been increased research to prevent sequelae after discharge from the ICU, not only in the patient but also in their family and caregivers; flexible visiting models, as well as family participation in daily activities such as reorientation, could bring benefits in the prevention of PICS and PICS-F.
When comparing the research results of Rosa et al., 2017 and Rosa et al., 2019, it can be concluded that their results are contradictory, however, it is necessary to consider the relevance of each. One possible interpretation is that Rosa et al, 2019 has greater statistical value as it was conducted in 34 different ICUs and their sample was approximately 6 times larger than that studied by Rosa et al. in 2017. Although the difference in the incidence of delirium between the restricted and flexible visiting models was not statistically significant, none of the variables considered in the study showed statistically more favourable variations for the restricted visiting model, from which it can be assumed that flexible visiting carries the same risks as usual visiting, so it could be used for interventions with marked benefit for the patient in the presence of the family member, such as reorientation. In addition, the researchers acknowledged that flexible visiting may have different effects in different socio-cultural contexts, so the results may vary in a different context than in Brazil.27,32
Studies such as Zhang et al. (2017) where a nursing protocol that mixes several interventions is evaluated, among them the increase in the number of visits (2 per day with duration of 30 min) from the first day in a cardiothoracic ICU, expose that the incidence of delirium in the GI: 19 (13.48%) patients was lower than the GC: 41 (29.93%) patients, with a statistically significant p value, p = .00148; due to the fact that this intervention was evaluated in conjunction with others, it is difficult to establish a cause-effect between the variables; however, if the results reported for the totality of the interventions in relation to the incidence of delirium are considered, a reduction is found for the MVE with respect to the MVR in all the cases analysed and contrasted. With regard to the other results of this intervention, the behaviour is similar with the exception of mortality in the ICU, which presents statistically non-significant values in all cases; with regard to days of stay, the variation is miniscule; with regard to the acquisition of infections, everything indicates that it is lower in the MVE.48
The analysis carried out in this review has allowed us to infer that flexible visiting is in itself a feasible intervention for the prevention of delirium in patients admitted to the ICU. However, it entails a series of challenges for the entire healthcare team, the patient and the family. This intervention, as described in this review, requires activities linked to it, such as family education, supervision of care, family-health team coordination and a set of interventions that the family must make for the patient during visits; for some authors, this represents a drawback for professionals, who consider that the presence of the family becomes an additional burden that can impair the organisation of care,49,50 increase the number of interruptions51 and contribute to a greater psychological burden for professionals.49 In contrast, Bannon et al. (2018) found that family, according to staff, are underutilised and could be used to assist in communication, counselling, selection of family elements and personal care if adequate support was available, and the presence of family was perceived as an opportunity to create a sense of familiarity and security for patients in the ICU.34
Delirium prevention strategies such as counselling via recorded messages by family members and caregivers have been shown to reduce the time to delirium episodes29 and the incidence of delirium in ICU inpatients.41 Statistical values reported by Munro et al. (2017), as well as Elcokany and Ahmed (2019) support this hypothesis29,41; the latter found that patients who received voice-recorded messages from family members had no delirium episodes within 5 days, while 28% of patients who received voice messages from a stranger had a delirium episode by day 5 and those with standard care had delirium from the first day of ICU admission.41
Research on delirium in non-ICU settings, such as Byun et al. (2018), has shown that the paediatric population in post-anaesthesia care units have similar outcomes when using recordings with a familiar voice. This study showed that there is a significant decrease in the incidence of delirium (delirium in emergency) in those children who received recorded messages with the mother's voice GI: 24.2 vs. GC: 60.6%, 95% CI: 4.88 (1.7/13.9); p = .006.52 The evidence seems to support the use of recordings as a tool in the prevention of adult and paediatric patients; the ease of using recordings makes this strategy a good means of keeping the patient oriented even when constant family companionship is difficult to maintain.
Family-mediated face-to-face counselling is another of the interventions studied in the prevention of delirium in ICUs; the research by Mitchell et al. (2017) states in their results that GI and GC have a similar incidence of delirium, suggesting that the strategy does not have a great impact.33 In contrast, authors such as Martínez et al. (2012) who evaluated a multicomponent strategy of education-reorientation of the family member in conjunction with extended visiting hours (5 h daily), found that the incidence of delirium was lower in the GI: 8 (5.6%) people, than in the GC: 19 (13.3%) persons; p = .027; with the evidence it is difficult to establish the impact this strategy has on the prevention of delirium,53 there are few studies that use the family as a re-orientator of the ICU inpatient. On the other hand, interventions related to mentoring developed by nurses and the orientation protocol seem to indicate that they reduce the duration of delirium, its severity and the number of days of hospital stay, although we must bear in mind that this is an intervention that has been little explored in settings such as the ICU.30
If it is accepted that flexible visiting is an effective intervention in the prevention of delirium, it would remain to evaluate the difference between these recorded messages and the same messages delivered in person by relatives during extended visits and regular visits through MENTOR-D; or the possibility that these recordings are complementary to the intentional family visit, understood as the visit in which the relative dedicates part of his/her stay in the unit to communicate with the patient, redirect him/her and participate in other activities agreed with the healthcare staff.
ConclusionsInterventions reported in the literature for the prevention of delirium that include the family are flexible visiting hours and reorientation of the patient in the ICU, both face-to-face and audio-mediated. Considering the data reported in the studies, both interventions may be useful in reducing the incidence of delirium, although further studies are needed on the flexibility component to be more certain of its efficacy.
While research reports a number of data that appear to establish a relationship between flexibility of ICU visits and decreased incidence of delirium, other benefits of flexibility and reorientation such as delirium-free days, reduction in duration of delirium, incidence of infections, hospital stay and family anxiety/depression have also been reported.
It is then up to the hospital and other entities involved in the regulation and management of family visits to develop and modify protocols for patient management in the ICU; likewise, it is the job of the interdisciplinary health team to integrate the family in patient care and thus mitigate the adverse effects associated with the family post-intensive care syndrome, always backed by scientific evidence, to constitute a management guide that allows the implementation of the ABCDEF package for the prevention of delirium in patients admitted to the ICU.
LimitationsAlthough the articles included in this research have at least 60% of the possible score in the critical reading analysis of the CASPe tool, there is no homogeneity in the quality of the evaluated articles which may affect the level of evidence of the results. However, the included manuscripts meet the minimum inclusion criteria in relation to methodology and results.
Since there were no mixed studies, the inclusion of qualitative articles could give rise to diverse interpretations, where quantitative results are refuted or contrasted, which is not the objective of this research. What is sought with the confrontation of these methodological designs is to demonstrate that the perspective of the needs of the family with a patient in the ICU is in the same direction as the evidence reported through statistical and mathematical analysis.
Two of the authors of the manuscript are novice researchers, who, although they were part of a research group, continue to develop research skills in the area, so the discussion could be affected in relation to its scope due to a lesser background in relation to the topic of interest; an element that is weighed against the contributions of a nurse doctor who is also part of the co-authorship of this research.
FinancingThis research has not received specific support from public sector agencies, the commercial sector or non-profit organisations.
Conflict of interestThe authors have no conflict of interests to declare.
We thank the Semillero de Investigación en Urgencias y Cuidado Crítico (SECUCRIT) of the Faculty of Nursing of the National University of Colombia for their training and guidance in the research process of this manuscript.
Please cite this article as: Pabón-Martínez BA, Rodríguez-Pulido LI, Henao-Castaño AM. La familia en la prevención del delirium en la unidad de cuidados intensivos: scoping review. Enferm Intensiva. 2022;33:33–43.