The COVID-19 pandemic has caused an unprecedented health crisis. Pressure on the National Health System has created unique demand particularly in certain services and care units like the critical care units.
ObjectiveTo learn about the experience of nurses in caring for people with coronavirus in critical care units.
MethodA qualitative phenomenological study that constitutes the second phase of a mixed methodology project. We conducted interviews with 17 nurses caring for patients affected by COVID-19 in critical care units. The interviews were audio-recorded, transcribed, and analysed using thematic discourse analysis.
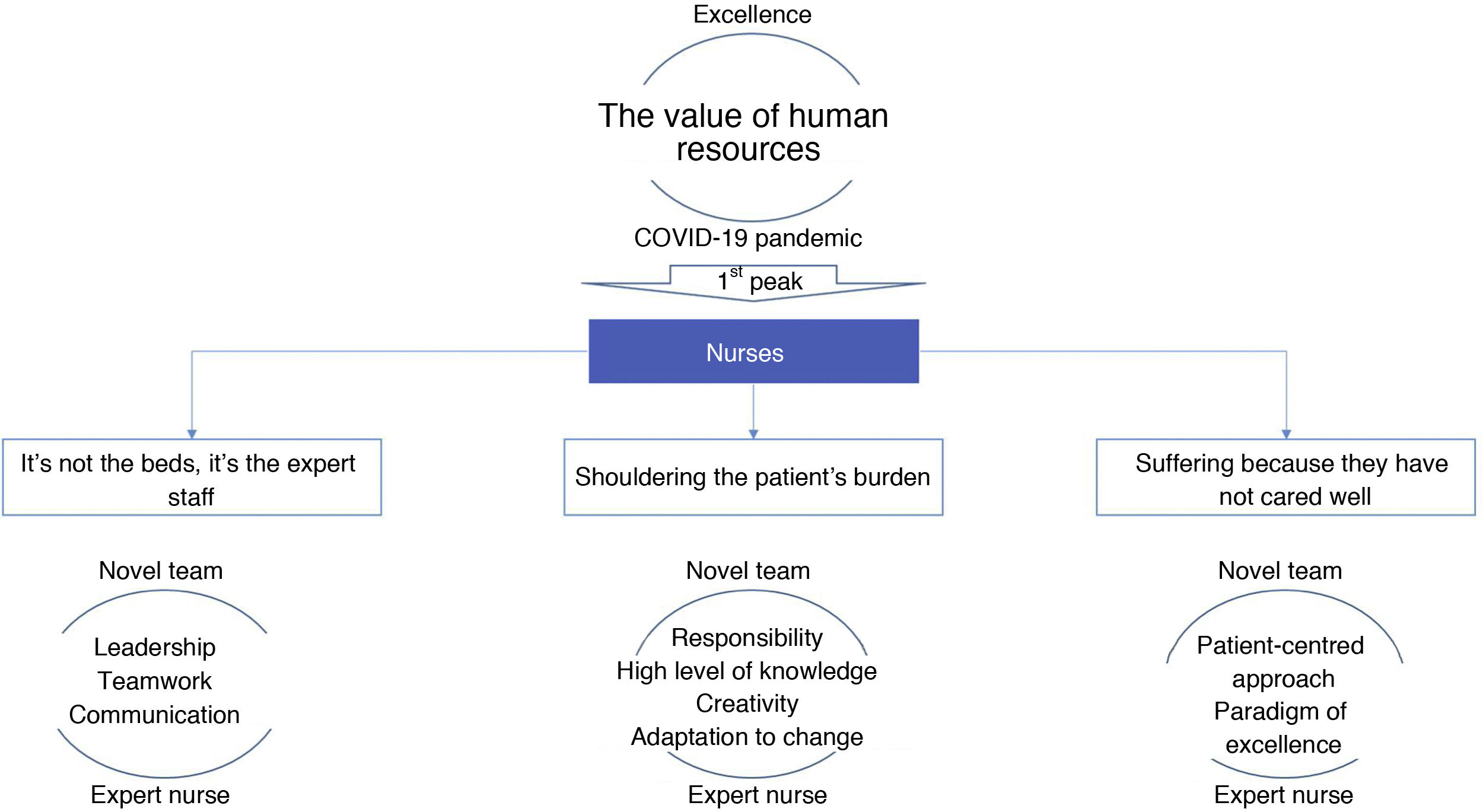
ResultsThis article shows the findings around the theme “the value of human resources” which is nuanced through sub-themes “it's not the beds, it’s the expert staff”, “shouldering the patient's burden”, and suffering because “they have not cared well”.
DiscussionExpert nurses have emerged as leading professionals in the care of the critical patient during the COVID-19 pandemic. This leadership is executed from a profile framed in an inclusive philosophy where wisdom, agility and intuition are the key elements underpinning problem identification and solving in a creative way, while adapting to the needs of the patient and healthcare team as they emerge.
ConclusionsExpert nurses have played an advanced role in the management of care and human resources by exercising effective leadership in the clinical setting. Care has been hampered due to the crisis, which causes nurses moral distress because they have been unable to meet standards of quality and excellence in care.
La pandemia por COVID-19 ha supuesto una crisis sanitaria sin precedentes. La presión asistencial sobre el Sistema Nacional de Salud ha generado escenarios insólitos de demanda especialmente llamativos en algunos servicios o unidades asistenciales como las Unidades de Cuidados Críticos.
ObjetivoConocer la experiencia de los profesionales enfermeros referida a la atención de personas infectadas por coronavirus en las Unidades de Cuidados Críticos.
MétodoEstudio cualitativo de carácter fenomenológico que constituye la segunda fase de un proyecto de metodología mixta. Se realizaron entrevistas a 17 enfermeras que prestaron cuidados en Unidades de Cuidados Críticos a pacientes afectados de COVID-19. Las entrevistas fueron audiograbadas, transcritas y analizadas mediante análisis temático del discurso.
ResultadosEn este artículo se muestran los hallazgos en torno al tema «el valor del recurso humano» que matiza su significado a través de los subtemas «no son las camas, es el personal experto», «llevando la carga del paciente» y sufriendo por «no haber cuidado bien».
DiscusiónLos profesionales enfermeros expertos se erigen como profesionales líderes en el cuidado del paciente crítico durante la pandemia por COVID-19. Este liderazgo se ejerce desde un perfil enmarcado en una filosofía integradora donde sabiduría, agilidad e intuición son los elementos clave que dan soporte a la identificación y resolución de problemas de forma creativa adaptándose a las necesidades emergentes de los pacientes y equipo de cuidados.
ConclusionesLos profesionales enfermeros expertos han desempeñado un rol avanzado en la gestión de cuidados y de recursos humanos mediante el ejercicio de un liderazgo eficiente en el entorno clínico. Los cuidados se han visto mermados por la situación de crisis, circunstancia que les genera sufrimiento moral por no haber podido cumplir con los estándares de calidad y excelencia en el cuidado.
In the first wave of the COVID-19 pandemic, nurses in Intensive Care Units (ICU) suffered both physically and emotionally because they found it impossible to deliver care as they wished, and saw those under their care die alone. They also experienced the fear of infecting those close to them.
ICU nurses have proven effective leaders of health teams, demonstrating their high level of skill in decision-making in complex clinical situations. They also endured the moral distress of being forced to deliver only "minimal, survival care”.
Study implications?Health care institutions should recognise and support the leadership of expert ICU nurses within health management teams and address the physical and emotional distress resulting from the care they delivered over the pandemic in the medium to long term.
The WHO declared a global SARS-CoV-21 pandemic on 11 March 2020.1 In the following weeks and during what was termed the first wave of the pandemic, the infection spread rapidly through Europe; 163,515 people had died in the European Union and the United Kingdom by the end of May. In Spain, according to data from the Ministry of Health, there were 238,564 confirmed cases, and 27,121 deaths.2 The autonomous community of Madrid (CAM) was one of the worst affected regions. The demand for health care put great strain on the public health system, whose material and human resources were insufficient. Public hospitals had to allocate a large part of their facilities to caring for the more than 40,000 infected people who had to be admitted. The spaces for the care of critically ill patients had to be extended and provided with the necessary equipment and staff. Nurses of the intensive care units and of the new spaces specifically created in the autonomous community of Madrid’s public hospitals were responsible for the care of the 3574 people hospitalised in these units over those months.3
BackgroundICU nurses have been on the front line of care during the COVID-19 pandemic, exposed to a substantial risk of infection and a dramatic increase in their workload. They felt uncertainty, nervousness, feared contracting the disease and infecting their family, and suffered the distress and frustration at seeing those they cared for dying alone and being unable to care for them as they would have wanted. They also suffered symptoms including fatigue, sleeping problems, headaches and breathing difficulties.4,5
Nurses had to cope with a challenging professional practice with limited information on COVID at the beginning of the pandemic, which then changed and became excessive as the scientific evidence increased.6 Organisational support was perceived as inefficient and there was a lack of material resources, in particular protective equipment.7 Despite these challenges, they felt a duty and responsibility to care for patients and their families. At the same time, they became aware of the social value of their profession and the importance of humanistic care, and launched initiatives to provide care like that provided before the pandemic, seeking to overcome the barriers imposed by the pandemic.8
In this context, ICU nurses have been considered a valuable and scarce resource due to their ability to deliver highly specialised care. Over this time, they have exercised greater autonomy in clinical decision making,4 assuming informal leadership with their versatility in undertaking diverse roles and tasks and increased interdisciplinary work.7 The experience of expert nurses in relation to their leadership role during the COVID-19 pandemic has not been explored.
The general objective of this study is to explore the experiences of nurses who have cared for people in ICUs during the first wave of the pandemic. The specific objective of this article is to describe the experience of expert nurses in ICUs in relation to their leadership role in managing the COVID-19 pandemic in these units, in the Spanish context.
MethodologyThis research study is the second phase of a sequential mixed quan-qual study9,10 developed in two phases: (1) descriptive cross-sectional study using a questionnaire with closed questions;4 (2) qualitative phenomenological study by means of in-depth individual interviews.
The study was conducted in the autonomous community of Madrid (Spain), in public hospitals classified as highly complex (HGC) and medium complex (HCI). The study population covered all nurses who provided care to patients with COVID-19 and voluntarily agreed to participate in the research study.
Purposive sampling11 was used to select the study sample, taking the inclusion criteria suggested by the results of the first phase of the project as the reference.4 Specific profiles were sought to ensure heterogeneity to reflect diverse realities and complementary discourses. Specific nurse profiles were sought with varying lengths of professional experience in ICU (>10 years, between 10 and 5 years, and <5 years) as well as those with no previous experience in ICU who were recruited to meet the increased demand. However, it was thought important to consider basic versus advanced training as well as care burdens outside the clinical setting (care of dependents; minors or elderly). Finally, it was considered relevant that they should have provided care in ICUs of hospitals of different levels of complexity. Access to potential participants was through the professional and personal networks of the research team (associate professors, collaborating professors, tutors, ICU nursing supervisors, ICU clinical colleagues…). Taking the objectives of this research into account, these people informed potential participants about the study. Participants who showed interest were contacted again by e-mail in which the study was explained in more detail, any queries were clarified and, if they agreed to participate, an individual interview was arranged. A total of 25 professionals were contacted, obtaining a final sample of 17 participants (Table 1) according to the saturation criteria of the thematic groups.12–14
Characteristics of the sample.
| Sex | n | % |
|---|---|---|
| Female | 15 | 88.2% |
| Male | 2 | 11.8% |
| Hospital | n | % |
|---|---|---|
| (Numerical code of the hospital) | ||
| 1 | 4 | 23.5 |
| 2 | 2 | 11.8 |
| 3 | 2 | 11.8 |
| 4 | 2 | 11.8 |
| 5 | 4 | 23.5 |
| 6 | 1 | 5.9 |
| 7 | 2 | 11.8 |
| The hospital’s complexity level | n | % |
|---|---|---|
| HGC | 8 | 47.1 |
| HCI | 9 | 52.9 |
| Professional experience (years) | n | % |
|---|---|---|
| >20 | 8 | 47.1 |
| >10 | 4 | 23.5 |
| 5−10 | 3 | 17.6 |
| <5 | 2 | 11.8 |
| <2 years | 0 | .0 |
| Professional experience in ICU (years) | n | % |
|---|---|---|
| >10 | 11 | 64.7 |
| 5−10 | 1 | 5.9 |
| <5 | 3 | 17.6 |
| <2 | 0 | .0 |
| No prior experience in ICU | 3 | 17.6 |
| Academic training | n | % |
|---|---|---|
| Degree | 7 | 41.2 |
| Postgraduate (specialist/masters/doctorate) | 10 | 58.8 |
| Expert | 4 | 23.5 |
| Specialist (EIR) | 1 | 5.9 |
| Other qualifications (bachelor’s degree) | 2 | 11.8 |
| Masters | 1 | 5.9 |
| Doctorate | 2 | 11.8 |
| Dependents | n | % |
|---|---|---|
| Yes | 8 | 47.1 |
| Minors | 8 (Mean of 2 children) | 47.1 |
| Adults | 0 | .0 |
| No | 9 | 52.9 |
EIR: Resident nurse; HCI: Medium complexity hospital; HGC: High complexity hospital; ICU: Intensive care unit.
The data were collected between June and August 2020. For this purpose, semi-structured qualitative interviews were conducted using the script shown in Table 2. Nine researchers with extensive experience as interviewers participated in the data collection with an average of 2 interviews each. Given the health emergency circumstances and the preventive measures during the phases of lifting of lockdown, the interviews were preferably conducted telematically through different applications for videoconferencing.15 One interview was conducted by telephone and another face-to-face in a work office in an ICU (which, at the time of the interview, had no COVID-19 patients). The interviews had a mean duration of 61 min with a range of 20−80 min. All the interviews were audio-recorded (with the explicit consent of the participants) and transcribed to facilitate subsequent data analysis. No visual recording of the interviews was made at any time (this was made clear telematically at the start of each interview by videoconference).
Interview script.
| Organisational aspects | To start with, I would like you to tell me about what your work was like on a typical day in your ICU, Emergency Department. |
| How did you organise your unit to care for all the infected people? | |
| What did you need (or would you have needed) to do your job well? | |
| Contagion prevention/safety | What were the safety measures in place in your unit to prevent your becoming infected? |
| What do you think of the measures or means that the organisation put in place for you to be able to do your job? | |
| Relations with the care team | What were relations like with the team members in your unit during care of/response to the pandemic? How would you assess the exposure of nurses compared to other professionals? |
| Personal/family/social impact | How has this experience – caring for COVID-19 patients – affected you personally? |
| Positive/negative balance | What was the hardest or most negative thing about this experience? |
| What aspects would you highlight as positive from this experience? |
Thematic discourse analysis was used according to the proposal of Braun and Clarke (2006).16,17 To this end, the material was read and reread, and general ideas were noted down. Then, initial codes were generated defined to express the meaning evoked and to guarantee the perspective of the context. The codes were then reorganised into thematic groups (a theme being considered as one that “captures” something important from the information in relation to the research question, representing a level of structured response or meaning). We started from a proposal of initial themes (in relation to the interview script), however, the possibility was left for new themes to emerge from the data. These initial themes were prevention of infection and safety, organisation and management of care, knowledge of the management of the critically ill COVID-19 patient and decision-making, interpersonal relationships, humanisation of care, and personal consequences.
Each of the 9 researchers performed the first coding of the interviews she had conducted, and defined the codes generated (in the form of a glossary of terms) and a first network of relationships representing, schematically, the meanings projected by the participant through their discourse. The main researcher condensed this initial coding work (with a total of 667 codes) by regrouping the codes according to the similarity of their meaning, leaving a list of 206 codes. From these, the interviews were recoded again using Atlas-ti software version 7.2. After this second coding, the codes were regrouped into groups of meanings. When each of the thematic groups had been worked on in depth, two meetings were organised as internal audits with the rest of the researchers. In addition, the final proposal of results was shown to two nursing care and care research managers show were experts in the area of intensive care for their critical appraisal. During the process of data collection and analysis, the research team adopted an attitude of constant reflexivity; we allowed ourselves to be surprised by theoretical emergence without our perspective being conditioned by clinical experience in different areas of critical patient care.
The study was approved by the Research Ethics Committee of the Universidad Autónoma de Madrid with code CEI-106-2063. All the participants were given written information about the project in supported verbally when they signed the informed consent form prior to the interview.
ResultsThe analysis of the interviews revealed one main theme “The value of human resources” and three sub-themes reflecting the nurses’ lived experiences “It’s not the beds, it’s the expert staff”, “Shouldering the patient’s burden”, and “Suffering because they have not cared well” (Fig. 1).
The value of human resources can be understood, from a simplistic and very operational perspective, as the degree of usefulness or aptitude of professionals to meet care needs. However, the participants’ discourse makes us consider it in terms of the value of the person (professional) who possesses, or to whom are attributed, positive qualities to undertake a given activity based on the paradigm of excellence.
It’s not the beds, it’s the expert staffThe admission of a large number of critically ill COVID-19 patients to ICUs has created an exceptional situation that has required the human teams in these units to be urgently reorganised. In particular, in relation to nursing staff, given the specific nature of the management and care of these patients, and despite having attempted to enlist nurses with ICU experience currently working in other units or levels of care, this provision of human resources has fundamentally involved recruiting inexperienced nurses. P_ICU_5. All kinds of people have come: people with experience in ICU, but who were working in other units, people from other communities, colleagues working in the private sector and doubling up in the public sector […] people who had finished the EIR […] people who had never worked before and people who came from the community. The picture was pretty bleak.
This implies that, most often the nurses worked in novel teams where those with ICU experience worked with a large number of colleagues with significant limitations and shortfalls in terms of competency. This circumstance highlights the value of human resources; as expressed by the participants “it’s not the beds, it’s the expert staff”. P_ICU_12. They said that whenever there was a ventilator, a physical space with an oxygen supply, a critical patient would be admitted. So, we went from the usual maximum of 12 beds to 52. Any corner was fine for them and there came a time when they were told to stop, because ventilators might still be coming from vets, from wherever, donated or whatever, but there were no more staff.
In the case of improvised ICUs, i.e., those created in peripheral spaces outside the intensive care departments (operating theatres, delivery rooms, recovery rooms or other spaces of varied non-clinical use), this term “novel” acquired a greater dimension, also incorporating other professionals (doctors and auxiliary nursing care technicians) without specialist training in the care of the critical patient. These teams could be described as open groups, i.e., heterogeneous (with professionals from different origins, backgrounds, and areas of specialisation), with their members constantly joining and leaving (due to relocations, leave due to COVID-19 or voluntary resignations) and with a dynamic of action centred on the here and now. In other words, the focus was on “getting on with” the work of the day and the most pressing demands without a more medium-term vision or a vision of continuity of care. P_ICU_1. At every turn people came and said “hello, they told me to come here, I’m Pepita and I’m a nurse or I’m such and such”. “Ah, well, OK, welcome. And that’s how it all started. It was all new people who came, who introduced themselves, we put on a sticker with a name and a category and that was it, that’s how it was. […] It was very chaotic, first because there were no working guidelines, not even the doctors (had) […] nobody knew how to manage them.
In these circumstances, expert or veteran nurses have played an essential leadership role in the management of care. The performance of this leadership role is related to the nurses' broad vision of the care processes, multidimensional perspective of care, deep knowledge of the patient, ability to interconnect different professionals to work under the same common objective and their communication and teaching skills. P_UCC_10. Nursing is more about battles and providing quick solutions […], You’re very clear about what you do, but then the range is very wide. So, there’s no physiotherapist and I have to do this, so I play the physiotherapist; they can’t make a call to the family and meet […] the different professional categories have their roles, their competencies. In the end, the nurse takes on so many roles […] in the end, we care for a person in different spheres, at a biopsychosocial level. So, there are changes that don’t escape us. I’m very clear about what my job is, what my functions are, what my competencies are. But the fact is that, apart from that, we cover a lot more, and so it’s not only care that’s the essence of nursing […].
In this leadership exercise, they recognise that they feel valued and empowered. They feel that they have carried the “burden of the COVID-19 patient” with a great responsibility that they define as “overwhelming”, “maximum exposure” and with a tremendous burden of suffering (these themes are developed below).
Shouldering the burden of the COVID-19 patientThe expert nurses acknowledge having “shouldered the burden” of the COVID-19 patient in ICU. This “shouldering the burden” involves management issues at all levels: structural and material resource management, human resource management, knowledge management and care management. P_ICU_10. You generally have the supervisor, but in these months, when everything has been so chaotic… having, for example, to set up two units (ICUs) from scratch… experience is a plus. You’ve had to manage how to set up the rooms, what material you're going to need. Even in the morning, having three units with so many staff on the payroll, the veteran nurses had to manage the resources and say: “no look, we’re going to send another veteran to the ICU and we’re going to go up to…”. In other words, we have not only had the technical management of material and so on, but also managing the human resources of staff of colleagues. Then there’s also the day-to-day management, how you’re going to manage your unit, how we’re going to organise the shifts for proning-deproning, now we’re going to see to hygiene this way…
From the perspective of the value of human resources, we will place special importance on the experience of care management in a novel team. The nurses’ discourse emphasises the urgent need to strategically organise the work and distribute the staff according to their level of competency to ensure daily care.
Given this situation of a lack of human resources with experience in the care of critical patients, different proposals for organising work arise, such working by task groups whose objective is to ensure sufficient and safe care while minimising the lack of knowledge of nurses who have been recently recruited or incorporated into the care team. Task or role-based working refers to the distribution of patients per groups of professionals who share tasks and responsibilities for the patients. This makes it possible to cover the competency limitations of some team members while training and accompanying them through the learning process. P_ICU_15. Suddenly, we’re working by function. One nurse gives the medication, another nurse prones. Well, that changes your perspective a little bit, you say “I thought I was never going to see this”, well, yes, you have seen it. In other words, that’s perhaps the biggest difference in the way of working, to change from caring for patients to working by function.
In this distribution of tasks, new roles arise for novel professionals who assist or support the rest of the team without assuming responsibilities directly related to patient management. P_ICU_8. Well, in this distribution of tasks, especially at the beginning, those who arrived who had never been here provided support from outside, they didn’t take on patients, many didn’t know the computer programme, so they didn’t even have to touch the computer. So, it was more a role of assistant, assisting the one who was inside. I used to call them messengers, we used to call them “passers-by”, because they were the ones walking along the corridor “go and get this, bring me a drip, hey, call the doctor on duty”.
This form of organisation has made it possible to arrange the dynamics of work to cover immediate needs (minimum care, which we will describe later). However, it creates significant differences in the distribution of tasks and, above all, in responsibilities for patients, with the expert nurses having to assume responsibility for ensuring the safety of the patient and the safety of the care team itself. Thus, there is talk of unreal nurse-patient ratios, i.e., on a quantitative level, ratios were covered, but the reality is that the veteran nurses worked with very over-sized ratios. P_ICU_7. The problem is that the ratio was a bit distorted because the nurse you were assigned as a companion could not take on the same as another nurse who knew the patient. P_ICU_5. Our ratio was 1:2 and the workloads became very large. We had to work in teams, which made it difficult, both due to the inexperience of working in teams, the work itself and the situation, because a lot of the work was ours. It was a bit chaotic in the end […] very suffocating, both in terms of workload, they’ve changed the way we act, the complexity of the patient, a lot of new people…
Training and accompanying novel professionals must be added to patient care. The expert nurses recognise that it has been a satisfactory experience in that the new professionals have been immensely helpful and committed to the team and have been very eager to learn. However, despite this, having to cover this training is interpreted as an additional burden that, at times, has put the veterans in situations of maximum physical and emotional stress. P_ICU_12. People were very willing and at the beginning you either did it yourself or you taught them…. But it reached a point where it was quite a burden, because… when you’ve already said the same thing 400 times, you've already given people a chance without saying “jeez, you should know this”, that is, not know it, but at least be alarmed or say “hey, something's up”… in the end you got up and did it or you stopped what you were doing and you went […]. So, we’ve been very burdened by the issue of training people […] I’m talking about physical and emotional burden. Physical because when we were distributing the patients there were some people who came and said: “no, because I’m new I don't take on patients”. You do take on patients because I can’t take four or five, you know? So, you take them and as far as we can we will help you, but you take them on.
The novel teams have also been joined by medical professionals with varied specialties and no experience in the care of critically ill patients. This, added to the demand for care that specialist doctors may have, has meant that the expert nurses have taken on the responsibility of making decisions and performing interventions that require a very high level of competency and responsibility. They mention this notion of feeling an “overwhelming responsibility”, as well as the imperative need to take on the leadership of the care team in critical situations in which they were the maximum point of reference in terms of expertise. P_ICU_7. (The doctors) also became aware of our work, especially when we were in the peripheral ICUs […] They could very often not be there in person, especially in the night shifts. So, we worked based on telephone communication […] and you would call them, tell them about it, or they would call you and ask you. […] I’ve felt much more valued, they’ve even recognised it, “we’ve realised how important the ICU nurse is”. […] In the end you were the one who detected something when they weren’t there. […] In the end you were their eyes where they couldn't be there. […] More than taking on roles, I think they let you decide, in the sense of “if you see that she’s hypotensive, you start the -nora(adrenaline)-, or if she needs more sedation, you sedate her”.
The participants also identify the nurse as the professional who has worked while being most exposed, i.e., closest to the patient, and spent the most hours at the bedside. This exposure is related to their potential, i.e., the ability to operate successfully in complex care scenarios. The nurses’ discourse reflects their flexibility and adaptability, and their ability to diversify to protect the team from exposure to contagion while ensuring patient safety by taking on the roles and tasks of other team members. P_ICU_2. The doctors […] didn't even have to put on their personal protective equipment (PPE) and go through. They did go through from their office… there were times when, if everything went more or less well and they (the patients) were stable, they didn’t even stay half an hour. But we were there all morning with the PPE. P_ICU_8. Yes, nurses have been the most exposed profession by far compared to the rest… because in the end practically all patient care depends on nursing. So, in the end you say “hey look, don’t go in (referring to the TCAE [assistant nursing care technician]), don’t expose yourself, I’ll go in, don’t worry” […] And with the doctors it was the same thing, in the end they were patients who were admitted for intubation. So that's where the doctor comes in, in that examination, that management, they were inside with us (it was shared between the two of us). But once the patient was stabilised, the nurses were the ones going in and out of the room).
The experience of the expert nurses is strikingly different from the subjective experience of the nurses recruited in newly created ICUs without previous ICU experience. The experience of the latter is marked by numerous difficulties in managing the critically ill patient. However, faced with the scenario of a novel team dealing with an exceptionally new and unpredictable situation, they find themselves in the dynamic of “giving their all” to respond to an unprecedented challenge where the notion of solidarity, willingness to help and group synergy become very strong and generate a feeling of moderate satisfaction. P_ICU_1. Everything had a very good vibe, because in general people were incredibly willing, everyone contributes, everyone helps and if you don’t know I’ll help you and I’ll do your work and mine, if necessary, don’t worry, so I’m really satisfied in this.
The discourse of the expert nurses is, however, marked by the experience of suffering. A suffering that, beyond the physical and emotional suffering shared by all the nurses who have cared for critical patients and their families in ICU, transcends a moral dimension. This discomfort is largely in response to the questions: Where am I? and What about the care?
The expert nurses recognise that they have been unable to meet the needs of the patients beyond the most basic questions. The question “Where am I?” would have a rhetorical character in the sense that nurses do not recognise themselves in a care scenario understood as a comprehensive approach to the patient, but rather in attending to the urgent (with the sole objective of guaranteeing the patient minimum stability that allows them to continue with the care of the rest of the patients in a catastrophic situation in which demands exceed resources). P_ICU_7. You didn’t work well because you couldn't give them the care that you (normally) give them. You’re left with the feeling… if it had been otherwise… maybe if we had worked better… It was a bit like “we have to keep them alive”, but we didn’t give them the best care because we couldn’t and, in fact, I think that luck had a lot to do with it, it wasn’t the same if the patient was admitted to the ICU as usual as if he was admitted to a bed that had been set up in a hurry. I’m left thinking that if they’d been admitted at another time, in another place, perhaps the end would have been different, that it wasn’t possible to do more, no, but that if the circumstances had been different, perhaps that’s always the thing.
In this sense, they speak of “war care” as opposed to “detailed care”, of “minimum care” versus “care” (as it is understood in essence). Thus, “war care” constitutes nursing interventions that aim to resolve the patient’s immediate serious situation to ensure survival. It means a reductionist, short-term view, situated in the scenario of resolving specific problems without getting to the root of the problem, in responding to the emergency situation and continuing to meet demand. P_ICU_10. I think that the care has not been the most appropriate or the best, and we haven’t been able to offer the care bordering on excellence as we would like. It was impossible for several reasons: on the one hand, the patient was in a very critical situation and so the first moments were all about techniques and saving the patient's life; on the other hand, you didn't just care for one patient, if we had 13 beds and we were… you might have to take 2 or 3 patients of that kind, so you couldn’t offer them the same dedication and the same care because you lacked hands […] It really was pure survival: for the patient to be kept well as far as possible. In other words, we were going to survive the shift and we could do no more.
“Detailed care” refers to the meticulous, specialist, protocolised, but at the same time individualised care provided in the ICU. This care is characterised by meticulousness, by the value of detail, of peculiarities, of singularity and of the relationship with the patient and the family. P_UCC_15. Well, I think that one of the characteristics that characterise special ICU services is the detail in which… I mean, your patients are cared for, procedures are performed. In the end, the nurse-patient ratio is two patients to each nurse. So, they are very closed departments that do things very meticulously according to a lot of protocols […] But the change from delivering super meticulous care for your patient, caring for your patients that you know inside out…
During the weeks of greatest demand for care, the structural limitations of many units, the lack of trained staff and the limited distribution of safety equipment (personal protective equipment) forced the organisation of nursing care based on “task-centred care” versus “patient-centred care”. In relation to this way of working, the nurses recognise that it was not possible to monitor the patient to have close command and control of their situation, but rounds of activities were conducted which, at an operational level, were practical but which reduced care to technical and procedural aspects. In this sense, they refer to “forgotten care”, care that has been neglected, that has been put to one side. P_ICU_4. A lot of care has been forgotten in the pandemic: care of central and peripheral pathways, change of medication systems… all of that has been… I think it has been like a war, we have left all the quality care behind, so to speak, in exchange for survival. P_ICU_8. Well, the way of working has not been as I was saying, as I would have liked, it has been a way of working that was beyond my control and I don’t like things being beyond my control, that has been a negative thing. P_ICU_10. In the end you devoted yourself to the most important things, to maintaining airways, to maintaining haemodynamic constants with the drugs and medication that are essential for these patients […] But I have noticed that there has been a lack of care. A critical patient needs many hours of nursing care at the bedside, and it’s not that we have neglected that part, it’s that there was no time or human resources, and it couldn’t be done.
Initially, in the context of chaos and imbalance between demand and response capacity, war care or minimal care were given priority, and detailed care gradually resumed later. However, the lack of expertise of many of the professionals caring for critical patients (in addition to the unfavourable learning conditions in which knowledge and skills were acquired during the pandemic) meant that this care did not take place and was not contemplated.
All this has had repercussions on the quality of care provided and, consequently, on the progress and prognosis of patients. The expert nurses have been vigilant in this care, trying, as far as possible, to ensure minimum quality of care and maximum patient safety. However, they feel powerless, stating that they “do what they can”. P_ICU_9. The most complicated thing would probably be […] working or dealing with so many new people. It's complicated because you can't be on top of it either. I’m not going to be controlling everything and then when you go in you see that they do things that, oh my God! […] So I think that it was all of them a bit and also talking to colleagues, I told you and you said that you found every mistake they had made in the cubicles, so you say… but of course it’s not… you arrived, you tried to solve it and that was it.
The nurses express a profound sense of frustration at not being able to care for patients under the usual and minimum established quality standards in the normal course of the ICU, in a controlled and meticulous manner. This situation generates a great deal of moral distress, interpreted as the pain perceived by the nurse in the belief that they have not cared for the patients according to the standards they consider acceptable (response to the inability to carry through a decision and/or ethical or moral action chosen). Despite this, they recognise that they have “given their all” by doing their best, making superhuman efforts to provide quality patient care, showing willingness and resignation. P_UCC_14. A burden, that is, a burden that I think these patients have borne and what seems to me to be the hardest thing is that in spite of everything they’ve had to go through, they’ve been left with this lack of care due a lack of nursing […] but bedsores at the sacrum level that’s inhuman, I mean, that’s inhuman.
The nurses also recognise that this experience has put them in an extreme situation where the essence of human suffering has been tremendously palpable. Contact with extreme situations has made them aware of dimensions of care that had been sidelined in their day-to-day professional practice. P_UCC_2. For me, the worst thing was the human suffering of those patients… the most tragic thing that has happened to me in all my working life, I’ve been working for almost twenty-two years… it was… I’ve never experienced such suffering, never in my life. That was what traumatised me the most and what still traumatizes me… I haven’t been able to get over it […] I’ve never seen such looks of fear, panic, and terror. What I’ve seen in those patients… it had never happened to me before and that’s what has shocked me the most and what has made me suffer the most.
Amidst so much chaos, so much demand, so much prioritisation, so much war care and so much neglected care, the expert nurses have restored and attributed exceptional value to care of the spiritual dimension. Faced with their helplessness in not being able to save the lives of many patients, they had an urgent need to accompany them in death and say goodbye. The need for interconnectivity for mutual relief, for mutual accompaniment, to manage shared suffering emerges very strongly. The nurses have become more aware of the value of their presence and the meaning of care, and in this scenario, they meet again and relieve their own distress by doing what they do best, caring. P_UCC_12. I said, “he can’t stay like that, I mean, he can't die and leave like that”. So, well, it was a horrible morning… but I said “well, if I have to leave later, then I’ll leave later”: I stayed with the patient, held his hand (I could hold his hand, with the gloves and the equipment, I was able to come closer to him). I stayed to hold his hand and that gave me a lot of peace, a lot of calm.
The study shows how expert ICU nurses fulfilled their professional role and duty in relation to the care provided during the COVID-19 pandemic: expert nursing practice, described by Patricia Benner (1992)18 and echoed in this context by authors such as Kubsch and Tyczkowski (2020),19 which highlights different degrees of competency acquired over time and reflective and critical experience.
The expert ICU nurses demonstrated their ability to deliver advanced care, taking on the management of complex and rapidly changing situations. They did so through their ability to link observed needs and demands with resources and interventions in a fluid, holistic and creative way, providing innovative solutions.20,21 This advanced level of competency implies the ability to see beyond, contemplating the specific needs of the person and family, as well as those of the therapeutic teams, to respond to their needs individually and with existing resources. It also involves accompanying and advising less experienced nurses, promoting care based on critical and ethical thinking.22
The expert ICU nurses emerged as professional leaders in critical patient care during the pandemic, developing leadership as per the characteristics proposed by Raso (2020)23 in an extreme situation: quick thinking, incident command systems, flexibility, communication, confidence, calm, moral courage, visibility, disciplined decision-making, and care (compassionate leadership).
Their holistic vision enabled them to exercise leadership in a multidisciplinary context. Their experience helped reorganise work, distributing it according to competency level and assuming greater responsibility for the care provided. Their professional background, focussed on the patient, drove them to provide the best possible care,24 demonstrating the union of expertise, imagination, intelligence, and reflection, which served to improve work performance in such adverse situations.
The findings highlight the leading role of expert nurses in the fight against COVID-19. Health managers and policy makers need to harness the knowledge, experience, and support of nurse leaders in clinical settings. This will undoubtedly contribute to bridging the gaps in leadership24,25 driven in part by the absence of senior nurses in decision-making bodies. One of the main priorities to overcome COVID-19, as proposed by the International Council of Nurses, is to involve nurse leaders in political decision-making.26 Likewise, the WHO27 highlight the need for action to strengthen nurse leadership globally through developing an influential role in health policy, as well as in decision-making and the management of health and social care systems.
This study also helps highlight the need to develop the specialty of intensive care nursing within the framework of the Spanish national health system, along the lines of other European countries such as Germany and Denmark.
The “war care” offered in ICUs to meet the high demand of COVID-19 patients has also highlighted the need to promote the humanisation of care in the post-COVID era.28–30 ICUs need to implement measures to reduce the social isolation of these patients and facilitate contact with, and potentially saying goodbye to, their loved ones.28 It is also essential to promote the psychological well-being of nurses.4,28–32
The results of this study are consistent with those of other countries where nurses have been primarily responsible for the care of a large number of patients. In Spain, this crisis has highlighted the urgent need to implement measures to ensure the provision of care in terms of patient safety, adapting nurse-patient ratios to patients’ characteristics and needs and to the expertise of the care team,30,33 and to provide the multidisciplinary teams of ICUs job stability. New forms and philosophies of human resource management need to be developed, which consider the levels of competence of health professionals and adapt to the level of care required by patients.
The emotional and moral distress experienced by the nurses revealed in the findings of this study is related to their failure to “care well” and their inability to maintain the high quality of nursing care customary in ICUs. In this sense Crigger (2004)34 highlights the ideal of “perfection” in which health professionals are educated, which hinders their ability to emotionally manage situations in which they perceive that they have not conducted their activity in accordance with standard practice. Thus, “moving away” from standard care would have a devastating effect, making them, in a way, “second victims” (a term described by Wu (2020)35 to refer to the impact on healthcare professionals of failures in patient care – first victims – with emotional reactions similar to post-traumatic stress). Although during the pandemic, health professionals were provided with occasional psycho-emotional support, the results of the study highlight the need for institutionalised support that responds to individual, and group needs and lasts over time.36
ConclusionsExpert ICU nurses have played a leading role in the care teams during the first wave of the pandemic, demonstrating their potential to manage complex clinical situations. They have acted as mentors to novel professionals and shouldered the patient burden in situations of scarce material and human resources (experts), chaos and uncertainty, demonstrating a remarkable capacity for adaptation.
The impossibility of continuing to care in the usual way, having to prioritise war care (minimum care, survival care) over detailed care (individualised care, “caring”) and the need to organise this on a task basis (versus patient-centred care) has been accompanied by a profound experience of moral distress, thus making them “second victims” of the pandemic.
The presence and accompaniment of patients and families has taken on special significance for nursing professionals, becoming a way of relieving mutual suffering.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank all the nurses who, while still coming to terms with the experience of the first wave of the pandemic, were generous enough to share their experiences with us. This was certainly another gesture of care and commitment.
Please cite this article as: González-Gil MT, Oter-Quintana C, Martínez-Marcos M, Alcolea-Cosín MT, Navarta-Sánchez MV, Robledo-Martín J, et al. El valor del recurso humano: experiencia de profesionales enfermeros de cuidados críticos durante la pandemia por COVID-19. Enferm Intensiva. 2022;33:77–88.