Multiple attempts during peripheral cannulation can have major consequences for patients, relatives, and healthcare professionals, therefore we set out to determine the extent of this problem in a paediatric intensive care unit (PICU).
ObjectivesThe main aim was to describe peripheral venous catheter (PVC) and peripherally inserted central catheter (PICC) cannulation in children in the PICU. Secondary objectives were to determine the success rate of the first cannulation attempt, to quantify patients with difficult venous access (DVA), and to explore the association between DVA and sociodemographic, technique and nursing-related characteristics.
MethodA cross-sectional descriptive study. Consecutive sampling was used to recruit patients aged 0-18 years admitted to the PICU who required peripheral venous cannulation. An ad hoc questionnaire was used for this purpose, including the presence of DVA as an independent variable.
ResultsA total of 163 venous cannulations were reported. A total of 55.8% (91) were performed in patients under 1 year of age. Of these, 38.7% (63) were successful on the first attempt and 36.8% (60) had DVA. When there was DVA, 85% (51) of patients had complications, median time to cannulation by short CVP was 30 minutes [15-53] and 2 or more nurses were required on 80% (48) of occasions.
ConclusionsWe found a low success rate at first attempt and a high proportion of DVA. More nurses and time were employed during cannulation and complications increased if the patient had DVA. A statistically significant association was found between DVA and age, weight, poor perfusion, veins that were neither visible nor palpable, DIVA score ≥ 4, history of difficult intravenous access, complications, number of nurses and time spent.
Los múltiples intentos durante la canalización periférica pueden producir importantes consecuencias que afectan a pacientes, familiares y profesionales, por ello se planteó la necesidad de conocer la dimensión de este problema en una unidad de cuidados intensivos pediátricos (UCIP).
ObjetivosEl objetivo principal fue describir la canalización de catéter venoso periférico y catéter central de inserción periférica en niños de UCIP. Como objetivos secundarios se propuso determinar la proporción de éxito en el primer intento de canalización, cuantificar los pacientes que presentan vía venosa difícil (VVD), así como explorar la asociación entre la aparición de la VVD y las características sociodemográficas, las relativas a la técnica y a las enfermeras.
MétodoEstudio descriptivo transversal. Mediante muestreo consecutivo se reclutaron pacientes entre 0 y 18 años ingresados en UCIP que precisaron canalización de acceso venoso periférico. Para ello se utilizó un cuestionario ad hoc incluyendo la presencia de VVD como variable independiente.
ResultadosSe recogieron 163 canalizaciones venosas. El 55,8% (91) se realizaron en pacientes menores de 1 año. El 38,7% (63) acertó en el primer intento y el 36,8% (60) presentaron VVD. Cuando aparecía VVD el 85% (51) de los pacientes tuvieron complicaciones, la mediana de tiempo para la canalización mediante catéter venoso periférico corto fue de 30 minutos [15-53] y se precisaron 2 o más enfermeras en el 80% (48) de las ocasiones.
ConclusionesSe encontró un bajo porcentaje de acierto al primer intento y una proporción elevada de VVD. Aparecía un mayor número de enfermeras y de tiempo empleado durante la canalización y un aumento de las complicaciones si el paciente presentaba VVD. Se encontró asociación estadísticamente significativa entre VVD y edad, peso, mala perfusión, vena no visible ni palpable, puntuación en la escala DIVA ≥ 4, historia de VVD, complicaciones, número de enfermeras y tiempo empleado.
What is known/what does this paper contribute?
Different authors have described a success rate from 46% to 76% in the first attempt at gaining access to a peripheral vein in paediatric patients in emergency units or paediatric wards. Difficult venous access (DVA) is defined in the literature as several failures to gain access; in 2004 Gónzalez was more specific, establishing 2 failures.
This study has the aim of identifying difficult venous access in the patients of an intensive care paediatric unit, based on the aforementioned specific definition. It explores its association with different factors and what leads to success at the first attempt. This field of research has hardly been studied, so that this study makes an original and relevant contribution.
Implications of the study
In paediatric patients the aim is to achieve successful access at the first attempt, to prevent multiple negative consequences. The starting point to reduce the number of venepuncture attempts is to quantify the size of the problem of difficult venous access. This will make it possible, if necessary, to implement interventions which help in this respect, such as the use of facilitating technologies, decision-making algorithms and predictive tools that aid the identification of patients with difficult venous access.
The catheterization of venous access is one of the most widely used techniques in hospitals for the administration of intravenous therapies and the extraction of blood samples.1,2 Venous access is defined as the procedure which communicates a vein with the exterior using a catheter.3 In intensive care units (ICU) all of the patients are fitted with some type of venous catheter, due to the need for treatment with an immediate effect in emergency situations or the frequent extraction of blood samples.4
Different types of catheters may be used in paediatric medicine, depending on the diagnostic and therapeutic needs of the patient, as well as the duration of treatment and the nature of the solution to be infused: a short or medium length peripheral venous catheter (PVC), a peripherally inserted central catheter (PICC) and a central venous catheter (CVC). Complications may arise during insertion as well as during use (pain, haematoma, arterial puncture, nerve injury, extravasation, phlebitis, thrombosis, infection or catheter obstruction). The complications associated with central venous catheters are more severe and put the life of the patient at risk. These complications include air embolism, pneumothorax or arrhythmia.5–7
Venepuncture for PVC and PICC usually takes place in the extremities, and it is a technical responsibility of nurses. However, the catheterization of venous accesses in children is more complicated than it is in adults, due to the characteristics of paediatric patients. Children’s veins are smaller in calibre and their surface vasculature is hardly developed and sometimes anomalous. They also have thick subcutaneous tissue, which hinders the palpation and visualization of the blood vessels.8 Another additional drawback is that children do not usually cooperate if they are not sedated, increasing the difficulty of catheterizing venous accesses.8 Several risk factors may also hinder a successful insertion, such as: being under 3 years old, weighing less than 5kg, prematurity, obesity, skin colour, dehydration or sepsis, vasoconstriction, suffering a chronic illness, having needed intravenous treatments in the past, and the experience of the nurse who attempts the insertion.8 In 2012 De Negri et al.9 described other risk factors such as malnutrition, the previous use of CVC, a history of phlebitis or previous history of difficult venous access.
The literature contains a definition of a patient with difficult venous access (DVA) that occurs when an experienced nurse is unable to catheterize a PVC using conventional methods after 2 attempts.10 These conventional methods consist of the application of a tourniquet, the lowering of the limb and the visualization and palpation of the target vein.11 Although this definition of DVA does not determine which criteria to use for a nurse to be considered experienced, the study by Larsen et al.12 stated that nurses with more than one year of experience achieved a higher percentage of successes when catheterizing a PVC. 8%-16% of adult patients have DVA when an attempt is made to insert a PVC, and this rises to 37% in patients of paediatric age.13 More than one attempt is required in 20%-30% of children even when conditions are ideal, and this increases to up to 50% in those who are less than one year old.8 In 2009 Kuensting et al.8 estimated that an average of 2.2 attempts were necessary to insert a PVC, taking half an hour to achieve this and failing to achieve a PVC in 5% of patients.
In 2008 to detect patients with DVA Yen et al.14 designed the Difficult Intravenous Access Score (DIVA score) for the paediatric population. This scale consists of 4 items: a visible vein and a palpable vein after the application of a tourniquet, age and a history of prematurity. This scale was subsequently validated and adapted for use in paediatric emergencies and for adult patients in surgical environments.15,16
These instruments were designed to predict the probability of failure of the first attempt at venous access, and to evaluate the need for unconventional techniques to aid access, such as transillumination devices, infrared light or ultrasound (US).11 Transillumination devices illuminate and locate subcutaneous veins using cold light.11 Several studies in which this device was used to achieve a PVC in children showed a reduction in the risk of failure in children under the age of 2-3 years, as well as shorter time taken to gain access.17–19 Infrared light is used to contrast blood vessels from the rest of the skin, and it has also been used to gain venous access during PVC in paediatric patients, where only patients with DVA obtained a higher success rate in achieving venous access at the first attempt.8,20 US is the most widely used technique in recent years, and it consists of a transducer which emits ultrasound waves that return a two-dimensional image showing the vessels and nearby structures, making it possible to guide the catheter point.16,21 The use of US for venous access in PICC has also been shown to lead to a lower number of failed attempts,13 reducing the appearance of complications such as haematomas and thrombosis.22 In paediatrics the evidence for the use of US for venous access in PVC is weak, although some results indicate that it increases the percentage of successes and reduces the time taken to perform the technique, with fewer attempts and re-aiming the catheter less often.2,23
Thus, multiple attempts at peripheral venous access reduce the vascular availability of the patient, increasing the risk of complications arising and delaying the start of treatment.8 Moreover, sometimes insertion or delay in withdrawing a CVC is the sole alternative to keep some type of venous access. Due to this bacteraemia associated with CVC are the most common nosocomial infections in the paediatric population, leading to longer hospitalization, higher costs and increased mortality.24 The presence of CVC is also a predisposing factor for thromboembolism in children, and up to 20% of the patients with catheters of this type develop thrombosis.25 Likewise, repeated attempts at venous access cause worry and dissatisfaction in the parents and frustration in the nurses, as well as pain and anxiety in the child.8 It must be remembered that small and even new-born children feel pain, and that their memories of pain may have physiological and psychological consequences in the future, causing poorly adapted responses to pain when they are adults.26
The main aim of this study is to describe venous access for PVC and PICC in children in a paediatric intensive care unit (PICU). The secondary aims are to determine the proportion of first attempts at venous access are successful, to quantify the patients with DVA and to explore the association between the appearance of DVA and patients’ sociodemographic characteristics and those of the technique used and the nurses.
MethodologyStudy design and populationA descriptive transversal study was designed to cover the period from 1 April 2019 to 31 October of the same year. Patients aged from 0 to 18 years were included who were admitted to the 16-bed PICU of a tertiary hospital and who required a short PVC (angiocatheter) or a long one (Seldinger’s technique), or a PICC.
The inclusion criteria consisted of the need for a short or long PVC or a PICC, and the consent of the legal tutors and/or the minor. The exclusion criteria were the necessity of creating venous access in an emergency situation (understood as a critical situation with evident danger for the life of the patient, requiring immediate action), as well as not filling in the part of the questionnaire that indicates the number of attempts that were necessary to gain venous access.
Data gathering processAfter a bibliographical review an ad hoc questionnaire was designed by the whole research team, with the presence of DVA as an independent variable and the following dependent variables:
- •
Sociodemographic and clinical data: age, sex, weight, medical diagnosis at admission and history of prematurity.
- •
Data on the technique used and venous access: catheter type, access zone, use of sedation, alteration in peripheral perfusion (presence of vasoconstriction, hypovolaemia or hypoventilation) and data corresponding to the limbs (the presence of any deformity, rigidity, oedema, lack of cutaneous integrity or other visible physical alterations that may affect venous access), history of DVA, previous recent attempts to gain venous access, a visible and/or palpable vein after applying the tourniquet, DIVA score, appearance of complications, rejection of the technique, alternative techniques, duration of the technique, successful venous access at the first attempt and total number of punctures.
- •
Data in connection with the nurses: professional experience, paediatric experience and the number of nurses who attempt venous access.
- •
Presence of difficult venous access: according to Gónzalez10 DVA is defined as when an experienced nurse is unable to create a PVC in 2 attempts using conventional means. DVA is also considered to exist when the technique is ruled out at any moment of the procedure, regardless of the number of punctures, due to a lack of available vessels or the high probability of failure perceived by the nurse.
The said ad hoc document included the DIVA score.14 This instrument is composed of 4 items: visible veins after the application of a tourniquet, palpable veins after a tourniquet, patient age and a history of prematurity. Each variable is awarded a score, and when the final score is equal to or greater than 4 there is a 50% chance of failure at the first attempt. Its items were included separately in the technique characteristics, so that their possible relationship with the appearance of DVA could be evaluated. I.e., once the questionnaires had been completed, the items were used to obtain the DIVA score.
Yen et al.14 reported that the area under the DIVA score ROC curve was 0.67, while the acceptable value would be 0.7; nevertheless, they stated that a high discriminatory capacity was not so important in this predictive rule, as the consequences would be minimum. Subsequently, the validation by Riker et al.15 showed an area under the curve of .72 (CI 95% [.67, .78]) and the validation by O'Neill et al.27 showed an area under the curve of .67; sensitivity when there was a score of 4 amounted to 75.9%, specificity was 51.8%, the positive predictive value was 84.4%, the negative predictive value was 37.7%, and the probability ratio was 1.6. This scale has yet to be transculturally adapted and validated in Spanish.
A guide was appended to the questionnaire to resolve doubts about recording the variables. A pilot study of the questionnaire content was carried out with 8 nurses in the unit. At the end of the design phase the unit nurses were trained in filling out the questionnaire, in a session in which the inclusion and exclusion criteria were explained, together with the definition of each variable, how to measure the time spent in gaining access to a vein, the procedure for signing the informed consent document, and the method for filing the completed questionnaires.
The questionnaires were collected consecutively when a patient required a peripheral venous access, including all of the attempts that were necessary until a successful access was created or the attempt was abandoned.
After a venous access had been created, the nurse in charge of the patient filled out the questionnaire and filed it. Sociodemographic and clinical data were extracted from the patient’s history by the said nurses, who also measured the time taken to achieve access using the headboard monitors or their mobile devices.
Ethical considerationsThe project was approved by the Research Commission and Ethics Committee of Hospital Universitario 12 de Octubre. The norms governing good clinical practice were followed at all times, guaranteeing compliance with the principles of the Helsinki Declaration on research with human beings (the World Medical Association, Helsinki Declaration, 2013). The anonymity of the participants was also guaranteed, together with the confidentiality of the information according to the stipulations of Organic Law 3/2018, of 6 December, on the Protection of Personal Data and Guarantee of Digital Rights.
The tutors of the minors who were admitted were verbally informed prior to carrying out the technique, and subsequently they were given the written informed consent document. When the tutors had any difficulty in understanding the Spanish language an interpreter was used, usually a family member with appropriate knowledge of the language, so that they were able to transmit our information to them correctly. Patients aged from 12 to 16 years old were also given an adapted informed consent document, accepting their opinion according to their age and degree of maturity, as well as their clinical situation (the Oviedo Agreement, 1997).
Data analysisData were revised and screened before processing them statistically using v25 of the IBM® SPSS package of programmes. Qualitative variables were described using frequencies and percentages, while quantitative variables were described using average and the standard deviation or the median and interquartile range, depending on whether or not they followed normal distribution. The Kolmogorov-Smirnov normality test was applied. For bivariate analysis between the independent variable DVA and the relevant dependent variables (sociodemographic characteristics and those in connection with techniques and the nurses) the following non-parametric statistical tests were used: Chi-squared, Mann-Whitney U test and Spearman’s correlation. Statistical and inferential analysis was performed with a 95% confidence interval and a level of statistical significance of P<.05.
Results163 peripheral vein access interventions were included during the period studied, of which 16 were PICC. The demographic data showed that 68.7% of the sample were male (112) and that 55.8% (91) were younger than 1year old. Diagnosis at admission, weight and history of prematurity are shown in Table 1.
Sociodemographic and clinical characteristics of the sample.
| Variables | N=163 (100%) |
|---|---|
| Age in yearsa | |
| <1year | 91 (55.8) |
| 1-3 years | 18 (11) |
| >3 years | 54 (33.1) |
| Sexa | |
| Female | 51 (31.3) |
| Male | 112 (68.7) |
| Weight in kilogrammesb | 6.4 [4-18] |
| Type of diseasea | |
| Multiple diagnoses | 29 (17.8) |
| Cardiac surgery | 25 (15.3) |
| Respiratory | 23 (14.1) |
| Airway surgery | 21 (12.9) |
| Digestive surgery | 14 (8.6) |
| Neurological | 13 (8) |
| Cardiovascular | 13 (8) |
| Infectious | 7 (4.3) |
| Orthopaedic surgery | 7 (4.3) |
| Metabolic | 5 (3.1) |
| Neurosurgery | 2 (1.2) |
| Renal surgery | 2 (1.2) |
| Not recorded | 2 (1.2) |
| History of prematuritya | |
| Yes | 35 (21.5) |
| No | 128 (78.5) |
Respecting the variables connected with the venous access technique used, the type of device used was fundamentally a short PVC, in 89.6% (146) of cases. The upper limbs were used the most often for venous access, in 69.5% (98) of the occasions, while the lower limbs were used in 20.6% (29) cases, the epicranial zone was used in 6.4% (9) cases, and other locations such as the exterior jugular vein were used in 3.5% (5) cases. The patient was sedated prior to the technique in 39.9% (65) cases, and perfusion alterations occurred in 38% (62) cases, or solely in the limbs in 21.5% (35) cases. 83.5% (136) of the patients had already undergone recent previous attempts at venous access. During peripheral venous access catheterization a vein was visible in 73.6% (120) cases, and a vein was palpable in 61.3% (100) cases.
38.7% (63) of first attempts were successful. When the first attempt failed, 2 further attempts were made in 27% (44) cases, 3 attempts were made in 12.9% (21) cases, while 9.2% (15) cases required 4 attempts and in 12.2% (20) cases there were 5 or more attempts. The median number of punctures was 2 [1-3]. 36.8% (60) of the sample had DVA with 2 failed attempts or rejection of the technique. In the case of PICC, 74.3% (12) of the venous access had to be repeated more than once.
The technique was abandoned in 13.5% of the total sample (22). The alternatives used after the technique was abandoned were: US-guided catheterization in 18.2% (4) cases, catheterization of a CVC in 9.1% (2) cases, and in 13.6% (3) cases venous administration was switched to oral administration. Other options were used in 59.1% (13) of the patients in whom peripheral venous access had been abandoned, such as administering intravenous medication intermittently rather than in continuous perfusion.
Several complications arose during the attempts at peripheral venous access. These consisted of tearing of the vessel or haematoma in 46% (75) cases, extravasation in 8.6% (14) cases and puncture of an arterial vessel in 1.8% (3) cases. Nevertheless, when the patients with DVA are differentiated from those without DVA, the DVA group had complications in 85% (51) punctures, vs 28.2% (29) n the group of non-difficult venous access (NDVA). A statistically significant association was found (P<.01) between the presence of complications and DVA.
When the first attempt at venous access failed, the median time taken to achieve it was 16minutes [10-39], while the median time taken for a successful first attempt was 5minutes [2-10]. On the other hand, the median time taken to achieve a PICC when the first attempt had failed was 32.5minutes [12.5-53.75].
The median time taken to create a PVC venous access in the DVA group was 30minutes [15-53], vs 5minutes [3-14.5] in the NDVA group, with a statistically significant association (Z=7.08; P<.01). Nevertheless, it took longer to create venous access for a PICC in the DVA group (5), with a median time of 50minutes [27.5-70], as well as in the NDVA group (11), at 30minutes [10-30].
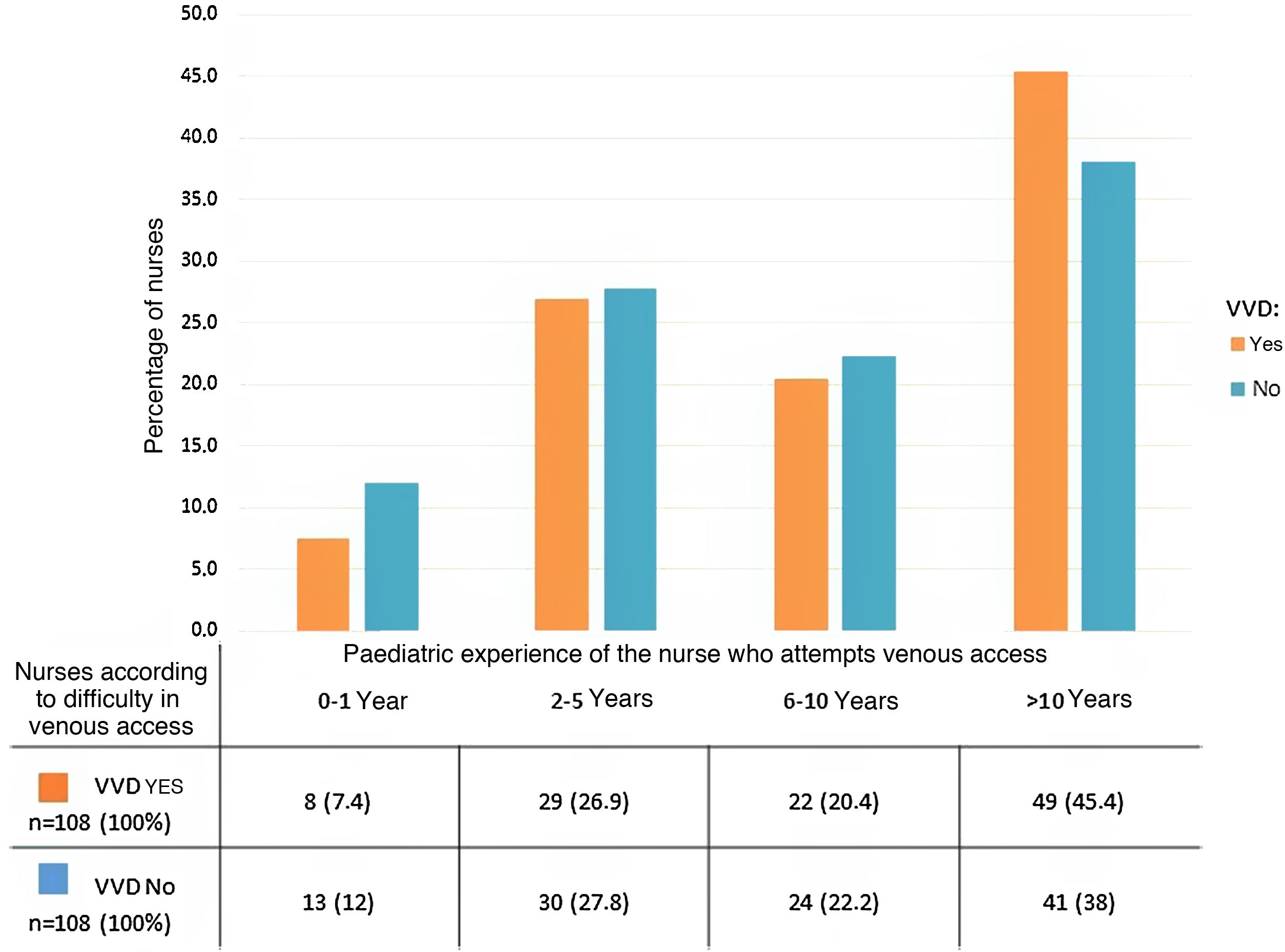
Respecting the number of nurses who were necessary to create a venous access using each technique, a single nurse did so in 95% (98) of the times when the patient had NDVA and only in 20% (12) cases when the patient had DVA. The median number of nurses in the DVA group was therefore 2 [2-3]. When the nurses’ paediatric experience was compared, a median of 9.5 years [3-13] was found in the DVA group, and this is similar to the 9 years [4.5-24] in the NDVA group, without any statistically significant differences (Fig. 1). No statistically significant difference was found when the total number of punctures was crossed with the length of paediatric experience (r=0.2; P=.16).
Lastly, a statistically significant association was found between the presence of DVA and the following variables: age, correct peripheral perfusion, a history of DVA, visible vein after tourniquet, palpable vein after tourniquet and the DIVA score (Table 2). A statistically significant association was also found between paediatric patient weight and the total number of punctures that were necessary, as heavier patients required fewer punctures (r=–0.33; P<.01).
Bivariate association between difficult venous access and dependent variables.
| Variables | Difficult venous access§ | Non-difficult venous access | P value |
|---|---|---|---|
| n=60 (100%) | n=103 (100%) | ||
| Agea | |||
| <1year | 44 (73.3) | 47 (45.6) | p=.01 |
| 1-3 years | 6 (10) | 12 (11.7) | |
| >3years | 10 (16.7) | 44 (42.7) | |
| History of prematuritya | |||
| Yes | 14 (23.3) | 21 (20.4) | p=.65 |
| No | 46 (76.7) | 82 (79.6) | |
| Use of sedationa | |||
| Yes | 24 (40) | 41 (39.8) | p=.98 |
| No | 36 (60) | 62 (60.2) | |
| Alterations in limbsa | |||
| Yes | 14 (23.3) | 21 (20.4) | p=.65 |
| No | 46 (76.7) | 82 (79.6) | |
| Correct peripheral perfusiona | |||
| Yes | 23 (38.3) | 78 (75.7) | p<.01 |
| No | 37 (61.7) | 25 (24.3) | |
| Recent puncturea | |||
| Yes | 53 (88.3) | 83 (80.6) | p=.12 |
| No | 6 (10.2) | 20 (19.4) | |
| History of DVAa | |||
| Yes | 47 (78.3) | 51(49.5) | p<.01 |
| No | 13 (21.7) | 52 (50.5) | |
| Visible vein after tourniqueta | |||
| Yes | 37 (61.7) | 83 (80.6) | p<.01 |
| No | 23 (38.3) | 20 (19.4) | |
| Palpable vein after tourniqueta | |||
| Yes | 25 (41.7) | 75 (72.8) | p<.01 |
| No | 35 (58.3) | 28 (27.2) | |
| DIVA score≥4a | |||
| Yes | 42 (70) | 41 (39.8) | p<.01 |
| No | 18 (30) | 62 (60.2) | |
DIVA: Difficult Intravenous Access Score; DVA: Difficult Venous Access (when an experienced nurse using traditional technique is unable to achieve venous access in 2 attempts).
A very low success rate for the first attempt at the creation of a peripheral venous access was found, at only 38%, with an average of 2 attempts. This fact contrasts with those in previous studies, which show more favourable success rates for the first attempt, at 46%-76%. Nevertheless, the average number of attempts in the total sample and the estimated time are similar to those of the studies by the said authors, who report from 1.75 to 2.3 attempts.8,14,28–30
This difference may be due to the fact that the sample in this study was completely composed of PICU patients who had highly complex chronic conditions which involved long stays and several re-admissions, so that their available veins had usually deteriorated. On the contrary, in the said studies the samples corresponded to emergency departments or general paediatric units. Rauch et al.17 state that in certain clinical environments with a large number of children with fragile and/or chronic conditions, the frequency of DVA may be higher. Additionally, if we examine the age distribution, almost half of the sample were unweaned babies of less than one year old. Their anatomical characteristics, low weight and lack of collaboration considerably increase the probability of failure.8,9 Lininger et al.28 and Black et al.29 report that the success rate in the first attempt for children who are still on a milk diet may be only 33%, which is closer to our results.
Based on the definition by Gónzalez10 we find that 36.8% of the sample had DVA with 2 or more failed attempts, or that access was impossible. This means that 4 of every 10 children required more than 2 punctures to achieve venous access.
Such a high proportion of punctures involves numerous adverse events which have been described by several authors, and which our patients experience every time they require the catheterization of a peripheral venous access.8,17 To this we can add that these patients are admitted with complex diseases (multiple diagnoses, cardiac and respiratory surgery), generally for a long time. This means that as they repeatedly undergo such a high proportion of punctures they eventually suffer a fall in vascular availability, making catheterization impossible and thereby aggravating the situation.31,32 It is therefore clear that DVA leads to an increase in complications, as different authors state.8,17 Haematomas were the most frequent complication, which coincides with the description by De Negri et al. in 2012.9
The estimated time taken to catheterize a venous access increases up to six times more when there is DVA. Larsen et al.12 estimate the time required for catheterization in patients who needed 2 or more punctures to stand at 28.43minutes (SD 28.06), with a median time of 20minutes. These times are very similar to those in our study. This causes a delay in treatments,8,10,17 and if we add the fact that no PVC was achieved in 13.5% of the sample, it may be necessary to seek alternative techniques such as brusquely giving certain medication orally, or the creation of CVC access to guarantee venous access in case of emergency, all of which involve an increase in the probability of bacteraemia.
The nurse-patient ration in the PICU where the study took place is 1:2. However, it is at care level III, and the majority of its patients are at level IV complexity (according to the Therapeutic Intervention Scoring System-28 [TISS-28]) measurement scale.33,34 The nurse - patient ratio should therefore stand at 1:1 or even 2:1.35,36 This means that there is a major work overload, and this increases considerably when there is a case of DVA, as if we take into account the results the need for two or more nurses increases by 75%, so that up to 3 or 4 nurses are necessary in 26.4% of cases. Moreover, the estimated time to create a venous access is 30minutes, so that the care provided by the nurses who are involved in the technique is delayed by this amount of time, multiplied by 2 due to the 1:2 nurse-patient ratio.
Kalish37 defines this situation as missed nursing care, i.e., “any aspect of care that the patient requires and which is omitted (partially or completely) or is delayed”. This concept is closely linked to the quality of care and patient safety. Therefore, any delay in the provision of care as the result of the difficulty of performing the technique in question will directly affect the quality of care and patient safety, as well as the satisfaction of the patient, their family and the professionals involved.38–41
With respect to the association of certain factors with the presence of DVA, although previous studies have described a major causal relationship between a history of prematurity and failure of the first attempt, this study found no statistically significant association between them.14 This may be due to the small sample, as this circumstance arose in very few occasions.
Nor was the use of sedation found to be associated with DVA in a statistically significant way. We found the explanation for this in the fact that the state of sedation of the individual was not recorded using a validated scale, so that in spite of having been given sedation, it is possible that a child was not properly sedated, so that as they did not cooperate, they hindered the technique, as several authors mention.8,30 Larsen et al.12 define the cooperation of paediatric patients as one of the factors most strongly associated with a successful first attempt at creating venous access.
We found no association between nurses’ experience and the probability of more than 2 failed attempts at venepuncture. The reason for this was found to lie in the long experience of the nurses in our unit. Larsen et al.12 state that nurses with less than one year’s experience have the greatest difficulty in performing the technique, and they found no significant association with success in the first attempt, and nor did Black et al.,29 who also found no association between the percentage of success and nurses’ years of experience.
Patients with a history of DVA and more than 2 failed attempts at venous access using the traditional technique or who display a predisposition to DVA should be subjected to beneficial techniques such as infrared, transillumination or US.8,17,22,42–44
In their research into US technique, Benkhadra et al.23 studied a population under the age of 3 years old. They found that less time was needed (6 times faster than with the usual technique) and there was a higher success rate in achieving access at the first attempt (85% vs 35%), so that they recommend that US should be used in small children with DVA. Doniger et al.45, with a small sample, found it took less time to create an access (down from 14.4minutes to 6.3minutes), a fall in the number of attempts (from 3 to one) and fewer occasions when the catheter had to be re-orientated (from 10 to 2). The results of Otani et al.46 show that results with the use of US are worse in terms of the time taken and the success rate. However, the recent study by Vinograd et al. in 201947 gives hopeful results, with a 30% improvement over traditional methods.
US-guided venous access may therefore be an alternative solution for the problem found. Nevertheless, in paediatrics, although the literature shows a tendency towards improvement in the first attempt, and even scientific societies have issued recommendations on the use of US in cases of DVA,43 no results are completely conclusive, so that this field should be studied in future lines of research.
Due to all of the above considerations it is necessary to reduce such a high percentage of DVA cases. Predictive tools should be created for this purpose, such as the DIVA14 predictive scale. These help us to detect which patients may have DVA, so that the beneficial methods described above can be considered for use. Although the said scale has not been validated in Spain, we found an association between the existence of DVA and the DIVA scale when it stood at 4 or more, so that it may be useful to adapt and transculturally validate it for use as a predictive tool. It is also necessary to implement decision-making algorithms and protocols according to the difficulty of venous access, as well as recommendations in clinical practice guides for achieving venous access in paediatric cases.
In their pre - post study Hartmant et al.48 state that the implementation of a DVA decision-making algorithm reduces the general number of attempts required to insert a peripheral catheter and the number of staff who attempted the technique per episode. Sou et al.49 reported that the use of US together with a decision-making algorithm improved the time used and first attempt success rate: 9 of every 10 catheters are implanted at the first attempt.
Schults et al., in 2019,50 state that the aim in children is to achieve a successful peripheral venous access at the first attempt, and these technologies should be used together with trained staff and predictive tools that help to identify patients with DVA, as well as clinical practice guides that set out a clearly defined strategy.
The chief limitation of this study is that the sample was exclusively recruited in the paediatric ICU of a single hospital, so that the results could only be extrapolated to a similar population. On the other hand, it is impossible to evaluate the difficulty of the technique depending on the use of sedation, as the degree of the latter was not recorded. This means that the degree to which the patient collaborated is not known. The measurement of the time taken to achieve access may be variable, because it was performed by different individuals without distinguishing between their use of patient headboard monitors or personal devices as timers. Lastly, the DIVA score has yet to be transculturally adapted and validated in our language, so that the DIVA variable was only shown to gauge whether it was associated with the presence of DVA according to the established definition, and the degree to which it may prove useful in the future.
ConclusionsThis study found a low percentage of successful first attempts and a high proportion of patients with DVA. If a patient had DVA then complications increased, requiring a higher number of nurses and more time to create the access. A statistically significant association was also found between the appearance of DVA and variables such as age, weight, poor peripheral perfusion, veins that were neither visible nor palpable, a DIVA score≥4, a history of difficult venous access, complications, the number of nurses and the time taken.
Conflict of interestsMaría de la Vieja received a grant from the intensification programme for research work in the area of nursing in the Hospital 12 de Octubre during the year 2019. The authors have no conflict of interests to declare.
We would most sincerely like to thank the whole nursing team in the PICU of Hospital Universitario 12 de Octubre, as this study was made possible by their collaboration and support.
Please cite this article as: de la Vieja-Soriano M, Blanco-Daza M, Macip-Belmonte S, Dominguez-Muñoz M, López-Sánchez E, Pérez-Pérez E. Vía venosa difícil en una unidad de cuidados intensivos pediátricos. Enferm Intensiva. 2022;33:67–76.