End-stage heart failure (HF) is a condition whose only successful long-term treatment, with a survival of more than 10 years, is heart transplantation. However, limited organ availability and the progressive increase in the number of patients with advanced HF have served as an impetus for the development of implantable mechanical assistive devices.
AimTo provide an overview of postoperative management and nursing care after the implementation of a Total Artificial Heart (TAH).
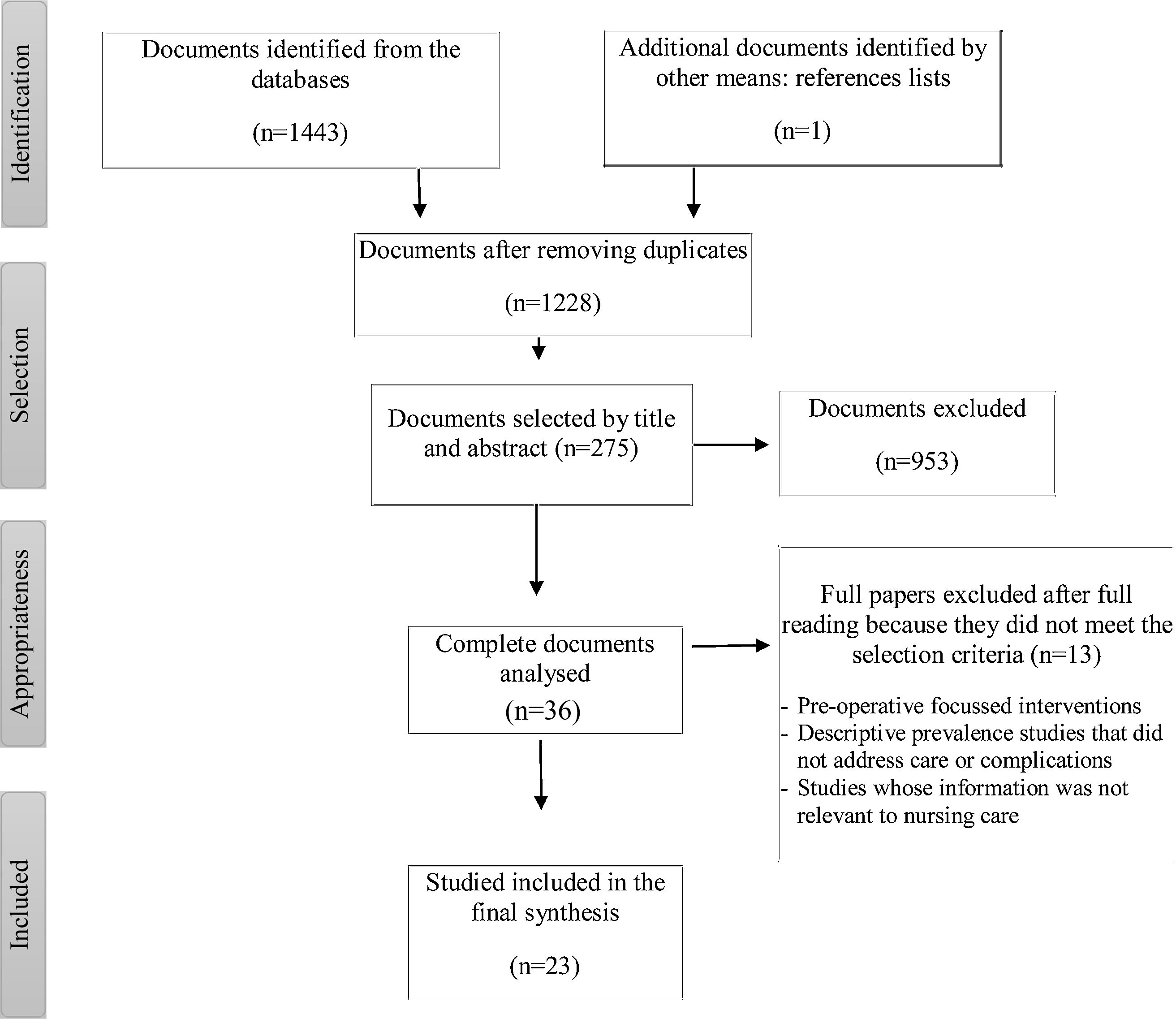
MethodsA scoping review was carried out by consulting the PUBMED, CINAHL, and COCHRANE databases. From all the documents located, information was extracted on the date of publication, country of publication, type of study, and results of interest to answer the research question. In addition, the degree of recommendation was identified.
ResultsTwenty-three documents were included in the scoping review. Results were classified in relation to: 1) description of the CAT SynCardia®; 2) nursing care in the immediate postoperative period (management of the device and management of hematological, infectious, nephrological, nutritional complications, related to immobilization, sleep-rest disturbances, psychological disorders, and patient and family education); and 3) follow-up at home.
ConclusionsThe complexity of implantation of the TAH, the multiple related complications that can arise during this process, both in the immediate post-operative and late, require a standardised and multidisciplinary management. The absence of standardised protocols raises the need for future studies to measure the effectiveness of care in patients with TAH. A multidisciplinary approach is crucial. Nurses must acquire autonomy and involvement in decision-making and develop competencies to address the patient's and family's physiological and psychosocial needs.
La insuficiencia cardíaca (IC) terminal es una afección cuyo único tratamiento exitoso a largo plazo, con una supervivencia de más de 10 años, es el trasplante cardíaco (TC). Sin embargo, la disponibilidad limitada de órganos y el aumento progresivo del número de pacientes con IC avanzada han servido de impulso para el desarrollo de dispositivos de asistencia mecánica implantables y corazón artificial total (CAT).
ObjetivoProporcionar una visión general del manejo postoperatorio y los cuidados de enfermería después de la implantación de un CAT.
MétodosSe realizó una revisión de alcance consultando las bases de datos, PUBMED, CINAHL y cochrane. De todos los documentos se extrajo información sobre la fecha de publicación, país de publicación, tipo de estudio y resultados de interés para responder a la pregunta de investigación. Además, se identificó el grado de recomendación.
ResultadosSe incluyeron 23 documentos en la revisión. Los resultados se clasificaron en relación con: 1) la descripción del CAT SynCardia®; 2) la atención de enfermería en el postoperatorio inmediato (manejo del dispositivo y manejo de las complicaciones hematológicas, infecciosas, nefrológicas, nutricionales, relacionadas con la inmovilización, alteraciones del sueño-descanso, alteraciones psicológicas y la educación al paciente y familia); y 3) el seguimiento en domicilio.
ConclusionesLa complejidad de la implantación del CAT, las múltiples complicaciones relacionadas que pueden surgir durante este proceso, tanto en el postoperatorio inmediato como tardío, requieren un manejo estandarizado y multidisciplinario. La ausencia de protocolos estandarizados plantea la necesidad de futuros estudios para medir la efectividad de los cuidados en pacientes con CAT. El abordaje multidisciplinar es crucial. Las enfermeras deben implicarse y adquirir autonomía en la toma de decisiones y desarrollar competencias para atender las necesidades fisiológicas y psicosociales del paciente y la familia.
The total artificial heart (TAH) is indicated for patients with acute or decompensated chronic irreversible biventricular failure, at high risk of imminent death, who are candidates for transplantation and for whom a suitable donor is not available. Most of the patients who receive a TAH are seriously ill; this is a highly complex therapy requiring trained and skilled professionals for appropriate management.
What it contributes?The analysis in this scoping review highlights the complexity of care for patients who have had a TAH implanted. It describes the management of the device, the main complications and the care to prevent them. However, low evidence was found in the articles reviewed and a lack of standardisation in the management of these patients.
ImplicationsThere are many divergences in patient care. Therefore, more intervention research is needed to fill this gap and to identify the most appropriate care for patients with a TAH and their families. It is also crucial that the entire healthcare team receive training, where nurses achieve autonomy, are involved in decision-making, and develop competencies to address the physiological and psychosocial needs of the patient and their family.
End-stage heart failure (HF) is a condition for which the only successful long-term treatment is heart transplantation (HT).1 However, the limited availability of organs and the progressive increase in the number of patients with advanced HF have resulted in the development of implantable mechanical assist devices.1–3
Continuous-flow left ventricular assist devices (LVADs) can provide circulatory support for many patients with end-stage HF, with outcomes very comparable to heart transplantation.1 However, there is a subset of patients with biventricular heart failure or structural abnormalities that preclude LVAD placement, and who require support with a biventricular assist device or total artificial heart (TAH).1–3
The CAT SynCardia® (SynCardia Systems, Tucson, AZ, USA) is currently the only heart available for clinical use approved by the Food and Drug Administration (FDA) as a bridge to transplantation. It has evolved from the Jarvic-7® (1985), later named CardioWest® C-70 TAH (1991), and is currently marketed as SynCardia® TAH (2004).4
The most common indications for TAH placement are severe biventricular failure, irreparable ventricular anatomical defects, acute myocardial infarction complicated by ventricular septal defect, post-transplant cardiac allograft failure, massive ventricular thrombus, refractory ventricular arrhythmias, hypertrophic/restrictive cardiomyopathies, complex congenital heart disease,5 and patient with cardiogenic shock unresponsive to vasoactive drugs at high risk of sudden death.6,7 Otherwise these are patients with acute or decompensated chronic irreversible biventricular failure, at high risk of imminent death, who are candidates for transplantation and for whom no suitable donor is available.4,8
The INTERMACS (Interagency Registry for Mechanically Assisted Circulatory Support) classification is a tool for stratifying patients with advanced HF into seven levels, based on their haemodynamic profile and degree of target organ damage. It allows better selection of LVAD/TAH candidates by predicting mortality and postoperative complications.4,8 Most patients who receive a TAH are critically ill, with an INTERMACS profile of 1 or 2, and 20% are on extracorporeal membrane oxygenation.4
TAH provides patients with effective circulatory support and allows end-organs to recover from the initial hypoperfusion injury. More than 60% of patients implanted with a SynCardia® TAH will later undergo transplantation, with a one-year survival rate of 70%.4,7 These patients require complex management by professionals with experience in the field of mechanical circulatory suppport.7
Despite the importance and complexity of nursing care in these patients and its implication for the success of the therapy, there is a lack of scientific evidence on the standardised management of these patients. Therefore, in consideration of the emerging need in our hospital to provide quality care to these patients, this scoping review was carried out with the aim of providing an overview of the key aspects of providing holistic nursing care to these patients and their families.
MethodologyDesignWe conducted a scoping review, following the recommendations of the Joanna Briggs Institute (JBI),9 based on the theory proposed by Arksey and O’Malley10 and updated by Levac et al.11
This type of review enables a broad analysis of an area of interest to identify gaps in knowledge, clarify key concepts, and report the types of evidence to guide clinical practice.9–11
We followed the following steps: a) define the research question and objective; b) describe the search strategy and identify relevant studies; c) determine the inclusion criterion and select studies; d) extract and analyse the information; e) report the results in relation to the research question and objective, and f) optionally consult with experts.11
To improve the quality and transparency of the research, we used the PRISMA-ScR checklist.12
Research questionThis review was guided by questions relevant for nurses to provide holistic care to patients undergoing TAH placement, prior to transplantation:
- -
What are the characteristics of a TAH and how is it managed?
- -
What are the main complications that the patient may suffer?
- -
What are the nursing care needs of patients and families after TAH implantation?
We searched the electronic databases PUBMED, CINAHL, and Cochran Library. We also undertook a hand search of journals specialising in the topic of interest and publications were reviewed using the snowballing technique. We undertook the search in 2017 and it was updated in 2021. English search terms (Total Artificial Heart, Syncardia and Cardiowest) were combined with Boolean OR (("Total artificial heart") OR (Syncardia)) OR (Cardiowest). We did not include terms such as "nursing care" or "postoperative care" because previous searches had missed important information to meet the objective of this review.
Limits were year of publication (2007–2021), age (patient >19 years), language (English and Spanish), and species (human).
Selection criteriaPublications related to nursing care and targeted interventions focusing on the postoperative period were included. In addition, publications addressing complications were selected. Finally, and in addition to the above criteria, publications providing a description of TAH and its management were also considered.
Studies related to other types of mechanical support or other types of TAH and those with information not relevant to nursing care were excluded.
After applying the selection criteria, a total of 23 papers were included in the review. The selection process can be seen in the PRISMA-ScR flow chart in Fig. 1.
Data extraction and analysisInformation on author, date and country of publication, objective, methodology, and type of study and outcomes of interest were extracted from the selected papers, as shown in Table 1.
Main characteristics of the articles included in the scoping review.
| Author/year/country | Objective | Methodology | Main findings | Grade of evidence (GRADE) |
|---|---|---|---|---|
| Nguyen et al. (2017)2 | To describe the centre's experience with total artificial heart (TAH) patients. | Retrospective study reviewing the medical records of 13 patients. | Outcomes and complications during TAH support are described. Postoperative bleeding, infection, acute renal failure, and respiratory failure are the most frequent complications. In addition, neurological events (ischaemia and haemorrhage), mediastinitis, sepsis, and pneumonia. | Very low |
| Canada | ||||
| Yaung et al. (2017)7 | To describe the history, indications, and perioperative care of TAH, with special emphasis on postoperative complications. | Literature review. | Indications, history, device description, pre-, intra-, and postoperative management are detailed. Post-operative haemodynamic management, mechanical ventilation support, renal and haematological disturbances, antimicrobial therapy, and transition from the intensive care unit to the ward are detailed | Low |
| USA | ||||
| Shah et al. (2013)14 | To describe the incidence and risk factors for driveline fracture after TAH implantation. | Retrospective clinical case review study of 66 patients. | Six patients presented with driveline fracture requiring repair all occurring with the portable Freedom driver. The most common areas of driveline fracture are near the connectors. None of the fractures resulted in severe haemodynamic compromise or death. The fracture was related to patient movement and waiting time to transplant. | Low |
| USA | ||||
| Parker et al. (2014)15 | To review indications, show imaging findings after TAH implantation and its complications. | Literature review and retrospective clinical case review study of 66 patients. | TAH implantation is an effective therapeutic option for the treatment of patients with end-stage biventricular heart failure. | Low |
| USA | Complications include: thrombotic risk (although less than other devices), bleeding, infection and driveline complications. | |||
| SynCardia Systems (2015)16 | To describe the device and its accessories; modes of operation; required monitoring and postoperative management of the patient. | Instruction manual | The components, the mode of operation of the ventricles, the different drivers, their operating modes and their connection to the device, and monitoring parameters, waveform morphology and alarms are described. | Low |
| USA | Post-operative care and management is detailed. | |||
| Copeland et al. (2012)17 | To describe the experience with implantation of the SynCardia® TAH, its indications, safety, and efficacy | Retrospective descriptive study of 101 patients. | Thirty-two patients died of multi-organ failure, pneumonia or pulmonary oedema, sepsis, neurological events, pancreatic abscess, intestinal ischaemia, and disseminated intravascular coagulopathy. | Low |
| USA | ||||
| Gaitan et al. (2011)18 | To review the historical development, current situation and management of the TAH. | Literature review. | The history and various devices prior to the SynCardia®, device components, indications, preoperative and intraoperative anaesthetic management, surgical technique, postoperative management and outcomes since 2004 are detailed. | Low |
| USA | ||||
| Kasirajan et al. (2012)19 | To review indications, surgical techniques and outcomes for the TAH. | Literature review and retrospective clinical case review study of 55 patients. | The following complications are specified: bleeding and tamponade, exacerbated renal failure requiring an extra-renal clearance technique, chronic anaemia (although with good tolerance to activity and resolving after transplantation), surgical wound infection and displacement of central venous catheters. | Low |
| USA | ||||
| Wong et al. (2011)20 | To describe the intraoperative and postoperative nursing care after TAH implantation. | Description of 1 clinical case. | The most important post-operative care (monitoring, early extubation, rehabilitation, and feeding), anticoagulation protocol and health education after ICU and before discharge are detailed. | Very low |
| Australia | ||||
| Presti and Crenshaw (2021)21 | An overview of mechanical devices and the TAH, their daily management and complications, to improve the education and training of nurses. | Literature review of 78 studies. | The following care is described: monitoring, optimising preload and afterload (volume and vasomotor tone), anticoagulation, patient education, inclusion of the caregiver. | Low |
| USA | The main complications are: stroke, infection, haemorrhage, thrombosis, renal failure, and chronic anaemia. To reduce the risk of cardiac tamponade, it is appropriate to delay sternal closure for the first 24−48 h postoperatively. | |||
| Demondion et al. (2013)22 | To describe the hospital experience with TAH patients and their management as outpatients. | Retrospective study of clinical case descriptions of 27 patients. | Fifteen patients died of multi-organ failure (46.6%) while on the TAH and 12 patients were discharged home. Seven patients were readmitted due to device infection, 3 due to technical problems with the driver and 4 due to other causes. Patients going home with a TAH and their families are trained (device, anticoagulation…) by a multidisciplinary team (nurse, anaesthesiologist and surgeon), with subsequent follow-up. | Very low |
| Francia | ||||
| Zimmerman et al. (2010)23 | To describe the complications related to the insertion of central venous catheters in patients with a TAH. | Retrospective study of clinical case descriptions of 2 patients. | Both patients suffered device failure with right ventricular obstruction, resulting in death. | Very low |
| USA | ||||
| Roussel et al. (2009)24 | To describe the comorbidity and survival of patients with a TAH. | Retrospective study of clinical case descriptions of 42 patients. | Complications described are device fit problems, air leakage due to driveline fracture, infections, neurological events, surgical re-interventions due to bleeding and/or tamponade, extrathoracic bleeding, renal dysfunction, respiratory problems, haemolysis and gastrointestinal problems, multi-organ failure. | Low |
| France | ||||
| Friedline et al. (2012)25 | To describe the clinical case of a patient with a TAH connected to the portable Freedom driver. | Description of 1 clinical case. | The portable Freedom driver has benefits such as increased mobility, lower cost, and improved quality of life. It allows for activities outside the hospital. It is important to educate the family on the care and maintenance of the driver. | Very low |
| USA | ||||
| Allen et al. (2009)26 | To describe the care of a patient undergoing TAH implantation. | Description of 1 clinical case. | The TAH and its components, important aspects before implantation, postoperative care, and psychosocial considerations are described from a multidisciplinary point of view. | Very low |
| USA | The main postoperative care issues are anticoagulation therapy, infection prevention, nutrition, mobilisation, management of psychosocial conditions (anxiety, depression, isolation, body image disturbance), and sleep regulation. | |||
| Tang et al. (2014)27 | To review the indications, management and outcomes of TAH. | Literature review and description of a clinical case. | The most frequent postoperative complications described are bleeding and cardiac tamponade. As a strategy, delayed sternal closure is proposed. Anticoagulation is started 24 h after chest closure. Heparin is avoided to minimise the risk of heparin-induced thrombocytopenia. The goals are an INR 2−3 and platelet function 20%-40% normal. | Low |
| USA | Renal failure increases after TAH implantation. Administration of atrial natriuretic peptide after ventriculectomy appears to have renal protective effects. | |||
| Anaemia following TAH implantation can be significant and persistent, but is well tolerated. | ||||
| Spilopoulos et al. (2015) 28 | To describe the experience of delayed sternal closure in patients with TAH. | Retrospective clinical case review study of 27 patients. | Delayed sternal closure appears to be an effective strategy, and contributes to a decrease in postoperative complications. Criteria to be considered are negative fluid balance, stable TAH function, and absence of bleeding or coagulopathy. | Low |
| Alemania | ||||
| Taimur et al. (2018)29 | To evaluate current practices for infection prevention in TAH recipients among different programmes. | Retrospective review of medical records of 13 patients (2012−2015). | Infections in mechanical assist devices are the most serious complications leading to increased morbidity and mortality and decreased quality of life for patients. Eighty percent of the centres have a standard protocol for surgical infection prophylaxis. Infections occurred after surgery in 52.2% of the centres. During the first month after TAH, bacteraemia accounted for 27.3%, transmitted infections 27.2%, pulmonary infections 9%, and mediastinal infections 18.2%. The mean post-TAH death rate due to infection was 14.5%. If device infection is suspected, cultures from the exit site of the cannulae, blood cultures should be taken and the infectious diseases department consulted | Low |
| USA | ||||
| Fernández et al. (2014)30 | To describe the early mobilisation of patients after TAH implantation. | Description of a clinical case. | In the second week of treatment the patient is able to walk with minimal assistance. The patient experiences changes in ventricular volumes depending on the postoperative day and the exercise performed, but exercise progress and tolerance is not affected. Early mobilisation is well tolerated and safe for the patient. | Very low |
| USA | ||||
| Nicholson et al. (2010)31 | To describe the TAH as a bridge to transplantation and physical therapy management, compared to left ventricular assist devices | Literature review and description of a clinical case. | The first 3 weeks of mobilisation are active and actively assisted movement exercises, progression of bed mobility, sitting and standing activities to increase tolerance to progressive and upright ambulation. During week 3 after TAH implantation the patient progresses to being able to perform therapeutic standing exercises and ambulation with a wheeled walker. Physiotherapists can provide evidence-based therapy for TAH patients using previously established guidelines for patients with heart failure and mechanical circulatory support. | Very low |
| USA | ||||
| Bellotto et al. (2011)32 | To describe the case of a TAH patient undergoing a strength and endurance training programme. | Description of a clinical case. | The programme of breathing exercises, aerobic training and calisthenics, and its evaluation by cardiopulmonary exercise test are detailed. The patient experiences an increase in peak oxygen consumption and an improvement in recovery kinetics during the 29-weeks training period. | Very low |
| Italia | ||||
| Brown et al (2020)33 | To describe a six-session cycle ergometry training programme for patients with TAH. | Description of a clinical case. | A training programme is described based on monitoring, symptom recording and the recommendations for the TAH. The patient improved his distance pedalled by 320% and functional capacity. He was subsequently discharged from hospital and successfully transplanted. | Very low |
| USA | ||||
| Savage et al (2014)34 | To describe the experience of patients with a TAH who are awaiting heart transplantation. | Phenomenological study. Unstructured interviews. | The overall theme is "Hope for the future". The 4 sub-themes include "Reflections", "For better or for worse", "The secret club", and "Coping and adaptation". | Very low |
| USA | In relation to "Hope for the future" participants discuss the feeling that life has become "very difficult" due to their limiting symptoms. The TAH gives them hope for the future because they find that they can do simple activities without becoming fatigued or out of breath. | |||
| "Reflections" deals with the severity of their illness and the desire to return home after the transplant. "For better or for worse" is about how their symptoms and heart function improve after TAH, but they are still restricted by technology. | ||||
| “The secret club” reflects that neither patients nor families want to be part of the "club" but feel supported by staff and other patients in coping with their situation. "Coping and adaptation" describes how patients tended to accept their circumstances. |
We used thematic analysis for the synthesis of the findings, providing an overview of the available evidence. The analysis was peer reviewed by four researchers and then cross-checked with the research group.
In addition, each of the studies was assessed according to the quality of the evidence, based on the GRADE working group guidelines (Grading of Recommendations, Assessment, Development, and Evaluation)13 (Table 1). It should be noted that this evaluation system was used for illustrative purposes and no studies were eliminated due to this criterion, because of the scarcity of high-quality studies.
ResultsFollowing the analysis of the available evidence, the results were grouped into three main themes, which in turn comprise several sub-themes, as shown in Table 2.
Outline of results.
| Themes and subthemes |
|---|
| 1) Description of the SynCardia® TAH |
| 2) Postoperative nursing care |
| 2.1) General management and monitoring considerations |
| 2.2) Management of the device |
| 2.3) Care related to major complications |
| 2.3.1) Thromboembolic events |
| 2.3.2) Haemorrhage |
| 2.3.3) Cardiac tamponade |
| 2.3.4) Delayed chest closure |
| 2.3.5) Anaemia |
| 2.3.6) Infection |
| 2.3.7) Renal disturbances |
| 2.3.8) Nutritional disturbances |
| 2.3.9) Physical mobility disturbances |
| 2.3.10) Sleep-rest disturbances |
| 2.3.11) Psychological aspects |
| 2.4) Educating the patient and family in self-care |
| 3) Home follow-up |
The SynCardia® TAH is a biventricular pulsatile pneumatic device that replaces the function of the heart and pumps blood into the pulmonary and systemic circulation.14,15
It consists of two independent artificial ventricles, externally connected by Velcro, containing four mechanical valves that allow unidirectional flow. Each artificial ventricle is divided by a flexible polyurethane diaphragm that separates the blood chamber from the air chamber. The artificial left ventricle (LV) is attached to the left atrium and native aorta via atrial connectors and Dacron grafts. Similarly, the artificial right ventricle (RV) is connected to the right atrium and native pulmonary artery (Table 3 Picture 3.1.).1,2,15 Therefore, complications related to native valve disease, rhythm disturbances, and ventricular dysfunction are eliminated.14 The capacity of the ventricles can be 50 or 70 ml and can generate a cardiac output of up to 7.5 and 10.5 l/min respectively. The choice of one or the other will depend on the patient's body surface area (50 ml < 1.85 m2; 70 ml > 1.7 m2 and thoracic diameter ≥ 10 cm).1,16,17
The ventricles are connected to an external Companion 2 driver (Table 3 Picture 3.2) via two pneumatic drivelines that are tunnelled through the chest wall.16 The vacuum generated by the driver and supplied by the pneumatic lines displaces the diaphragms downwards, allowing blood to enter the ventricles. To eject the blood, a pulse of air moves the diaphragms to the top of the ventricles and the 4 valves ensure unidirectional ejection.15,16,18
The Companion 2 driver contains a driver or operating unit. This driver contains two pressurised air tanks, a vacuum pump, a control panel, and three batteries (one internal and two external). It must be connected to the mains and can be powered by batteries for transfer.15,18 In the event of failure, it can be replaced by a spare driver or a hand pump. In addition, it can be coupled to another driver system (Caddy), facilitating intra-hospital transfer (Table 3 Picture 3.3).
The control panel is used to programme the operating parameters (suction, heart rate (HR), and % systole and diastole), and to display diagnostic and monitoring data, flow, and flow and pressure waveform morphology, trends and alarms.15,16 It is for hospital use only.16
To facilitate patient autonomy and mobility and discharge home, the portable Freedom Driver®, a smaller and lighter pneumatic device, was approved in 201416 (Table 3 Picture 3.4). It displays cardiac output (CO), left filling volume (FV), and HR, the only adjustable parameter on this driver, and alarms with different priority.16 It is powered by 2 lithium batteries that provide 3 h of autonomy and can be connected to the mains. It can be carried in a backpack or shoulder bag.2,15
Postoperative nursing careThe focus of postoperative patient care is to maintain optimal haemodynamic status to recover the various organs and prevent actual and/or potential complications related to the TAH.18,19
General management and monitoring considerationsRoutine monitoring includes invasive blood pressure (BP), central venous pressure (CVP), oxygen saturation (SpO2), HR, VF, and left and right CO.20,21 Electrocardiography is not necessary because the native heart has been explanted.21
The TAH is preload dependent. Therefore, it will be necessary to optimise intravascular volume and vasomotor tone. If necessary, vasodilators will be used to prevent increased systemic vascular resistance and hypertension or, alternatively, vasoconstrictors will be necessary if the patient has vasodilatation and decreased preload.18,20,21 Chronotropic and inotropic drugs are not necessary, because the native myocardium has been removed.14,18,20 In the event of cardiorespiratory arrest, defibrillation and cardiac massage are ineffective.16
Another important aspect is related to the insertion of central lines. Central venous catheter (CVC) entrapment is a rare but present complication, which can result in the death of the patient.15,22,23 No catheter should be in close proximity to the valves of the TAH, as it could be suctioned and cause malfunction, resulting in haemodynamic collapse.16–21,23,24 Peripherally inserted CVCs are also dangerous, as the tips can migrate distally when the arm is raised and be similarly trapped by the mechanical valves.19 Regular radiological checks are important23 and whenever a sudden and unexplained decrease in CO occurs, and the need for the CVC must be assessed daily.16
Moreover, the TAH contains ferromagnetic components and therefore MRI is contraindicated.16
Management of the deviceThe most important aspects of device management include daily checks of parameters, waveforms, and alarms, and checking for kinks in the drivelines.19,20
To maximise CO and optimise perfusion of peripheral organs it is necessary to adjust the parameters of the TAH,19,20 according to patient characteristics, afterload, and volaemia. The goal is to achieve partial filling and complete ejection. Partial filling allows for increased volume to be taken up in the event of increased patient needs due to increased physical activity.16 Partial FV should be maintained between 50−60 ml for 70 ml devices or 30–40 ml for 50 ml devices.14 Full ejection is achieved by presetting an ejection pressure higher than the patient’s afterload.16 In addition, together with a high HR, blood stasis is minimised and the risk of thromboembolism is decreased.19,25
The waveform morphology provides information on the performance of the device. The pressure waveform assesses whether ejection is complete and the flow waveform assesses whether filling is partial (Table 3 Picture 3.5).
There may be problems with the drivelines such as kinks or fractures that could cause air leakage. These are identified audibly and/or with low flow alarms.16 They tend to be more frequent during mobilisation and with the portable driver.14,15 In addition, driver malfunctions may occur, requiring driver replacement.22,24,25
Care related to main complicationsIt is important that assessment and care are directed towards preventing the following complications (Table 4).
Complications, assessment and care, and level of evidence.
| Main complications | Assessment and care | level of evidence (GRADE) |
|---|---|---|
| Thromboembolic events | • Administration of platelet antiplatelet therapy and perioperative anticoagulation18–22,24,26 | Low–very low |
| • Maintain partial thromboplastin time (PTT) range > 50 s and INR 2.5–3.016 | ||
| • Monitor haematological status daily (blood work)26 | ||
| • Daily monitoring for signs and symptoms of bleeding and checking the driveline orifices,26 | ||
| • Early mobilisation of the patient to prevent deep vein thrombosis20 | ||
| Bleeding | • Assess drain debit, haemoglobin, systemic perfusion7,20 | Low–very low |
| • Monitor signs of hypovolaemia (flattening of the arterial line waveform, decreased FV and CO, fall in CVP and BP, oliguria and lactic acidosis)7,20 | ||
| Cardiac tamponade | • Assessment of haemodynamic status (decreased CO and increased CVP).17 | Low |
| • Monitoring of waveform morphology of the filling phase of the TAH (shows early filling).15 | ||
| • Assessment of tests; 1) chest X-ray (changes in cardiac silhouette contour)15; 2) echocardiography15; 3) surgical exploration.15 | ||
| • Maintain chest drains for at least 1 week.19 | ||
| Delayed chest closure | • Criteria to be considered for closure: negative fluid balance, stable haemodynamic and TAH function parameters and absences of bleeding or coagulopathy.28 | Low |
| • Withdrawal of mechanical ventilation once the chest is closed7,18 | ||
| Anaemia | • Assess haemoglobin levels, systemic perfusion7,20 | Low–very low |
| • Avoid blood transfusions, unless patients are symptomatic or signs of poor perfusion18,19 | ||
| Infection | • Taking cultures from the exit site of cannulae, blood cultures and assessment by the infectious diseases department29 | Low–very low |
| • Early extubation and early removal of invasive lines7,18,20 | ||
| • Aseptic care of urinary catheter and parenteral antibiotherapy15,17,26 | ||
| • Care of drivelines: emphasising the following aspects: hand washing, aseptic technique, assessment of the orifice, keeping the dressing dry, and only using water-soluble antiseptics.16 | ||
| • In patients with delayed chest closure, change the dressing covering the polytetrafluoroethylene membrane sewn to the skin edges daily and using aseptic technique26,28 | ||
| Renal disturbances | • Monitoring of urine output and renal function.19 | Low–very low |
| • Use of synthetic atrial natriuretic peptide if there is oliguria without decreased TAH flows, tamponade or hypovolaemia19,27 | ||
| • Extrarenal clearance procedure19,24 | ||
| Nutritional disturbances | • Early initial of oral nutrition20,26 | Low–very low |
| • Assessment by a nutritionist26 | ||
| • Administer a low-sodium, high-calorie, high-protein, and supplemented diet26 | ||
| • Present meals in an appealing manner, or administer appetite stimulants16 | ||
| Physical mobility disturbances | • Use pre-established protocols30,31 | Low–very low |
| • Physical rehabilitation and early ambulation20,26,30 | ||
| • Respiratory physiotherapy20,32 | ||
| • Progressive physical therapy both in activity and duration and guided by physiotherapists30–32 | ||
| • Monitoring pain, driver parameters, and signs and symptoms of exercise intolerance30–32 | ||
| Sleep-rest disturbances | • Group activities together and minimise interruptions to facilitate patient sleep and rest26 | Very low |
| Psychological aspects | • Encourage contact with family and loved ones, listening to music or other pleasurable activities26,34 | Very low |
| • Emotional support of family.22,26,34 | ||
| • Multidisciplinary approach encompassing all the needs and concerns of the patient and family26 |
The SynCardia® temporary TAH has a shorter flow path than any LVAD and there is no contact between the blood and the cannulae.24 However, platelet interactions with the non-biological surfaces of the device result in continuous protein activation, increasing the risk of thrombosis despite therapeutic anticoagulation.15 Thrombotic complications include pulmonary, arterial, visceral, retinal, and neurological complications.15,18 Neurological complications are rare and no significant neurological deficits have been observed in most transient ischaemic attacks.15,17
Administration of antiplatelet aggregation and perioperative anticoagulation contribute to the prevention of thrombosis.18–22,24,26 The level of anticoagulation will depend on the clinical status of each patient, with targets of partial thromboplastin time (PTT) > 50 s and INR 2.5–3.0.16 In the literature reviewed, we found differences in these ranges (INR 2−3.5,19,22,24,27 PTT 60–80 s24,26) and in the drug therapy used (aspirin, dipyridamole, pentoxifylline, heparin, warfarin, and/or bivalirudin).2,17,20,26,27
Daily monitoring of haematological status (blood tests, signs and symptoms of bleeding, and checking the driveline orifices)26 and early mobilisation of the patient to prevent deep vein thrombosis are of utmost importance.20
HaemorrhageMost haemorrhagic events occur in the chest or mediastinum and may cause cardiac tamponade requiring reoperation.15,22,28 Rarely, suture dehiscence may occur at anastomoses requiring immediate surgical repair.15
Furthermore, the obligatory use of anticoagulation and antiplatelet therapy predisposes patients to late haemorrhage, both intrathoracic and extrathoracic.15,17,24,25
In this regard, the nurse should assess drain debit amount, haemoglobin, systemic perfusion, and signs of hypovolaemia (flattening of the arterial line curve, decrease in VF and CO, fall in CVP and BP, oliguria, and lactic acidosis).7,20
Cardiac tamponadeRarely, pericardial haemorrhage can lead to cardiac tamponade,15,24 and can rapidly cause haemodynamic collapse (decreased CO and increased CVP).17 The waveform morphology of the filling phase shows early filling. In addition, changes in the contour of the cardiac silhouette can be observed on X-ray.15 The diagnosis will be confirmed by echocardiography, or surgical exploration.15
Maintaining chest drains for at least one week can prevent cardiac tamponade.19
Late chest closureThe high incidence of haemorrhagic complications with the need for re-exploration after implantation has led to the use of delayed sternal closure strategies.28 These allow easier access to deal with perioperative haemorrhage and thus decrease the risk of cardiac tamponade.19,28
There is no standardised protocol for chest closure.15,28 Spiliopoulos et al.28 describe criteria to consider such as negative fluid balance, stable haemodynamic and TAH parameters, and absence of bleeding or coagulopathy.28 Mechanical ventilation should be withdrawn once the chest is closed.7,18
AnaemiaSevere anaemia is frequently described while the patient has a TAH.18,19,25 The origin is multifactorial, although frank haemolysis is common. Kasirajan et al.19 propose lowering the ejection pressure to improve it.
Despite anaemia, patients show reasonable exercise tolerance with minimal symptoms.19 It is recommended that blood transfusions are avoided unless patients are symptomatic or there are signs of poor perfusion,18,19 because they may generate antibodies making transplantation difficult.18
InfectionPostoperative infection is one of the most common complications. These include respiratory infections (bacterial pneumonias), bacteraemia, and urinary tract infections.7,15,17,22,24,29 Less common are sepsis, mediastinitis, sternal wound, or device infection.12,17,22,24,29 The latter are the most serious complications, increasing morbidity and mortality and reducing the patients’ quality of life.29 If suspected, cultures of the cannulae exit site and blood cultures should be taken, and the infectious diseases department should assess.29
Early extubation, early removal of invasive lines,7,18,20 aseptic care of the urinary catheter, and parenteral antibiotherapy15,17,26 reduce the risk of infection.
Infections related to the lead lines are particularly important,7,15,22 and can affect the exit site and progress upwards to contaminate the subcutaneous tunnel and the implanted ventricles. In addition, increased patient activity can cause trauma and loss of the skin barrier, providing an opportunity for bacterial overgrowth.22 There is controversy regarding the care of drivelines. The manufacturers only recommend following the protocols of the hospital and the specialist nurse. Hand washing, aseptic technique, assessment of the orifice, keeping the dressing dry and using only water-soluble antiseptics are emphasised. Ointments can delay tissue growth around the drivelines.16 Allen et al.26 emphasised the importance of performing aseptic technique twice/day or once/day if there is no exudate. Demondion et al.22 describe cleaning with hypertonic solution, once/day in the event infection or every 2 days if there is no infection and when the orifice has healed. Taimur et al.29 warn of the need to follow a strict protocol that includes dressing changes every 24 h until the TAH is explanted, an aseptic technique using a ChloraPrep® single application kit (2% chlorhexidine gluconate and 70% isopropyl alcohol), and covering the orifice with Tegaderm dressing, and daily follow-up by the specialist multidisciplinary team.
In patients with delayed chest closure, only change of the dressing covering the polytetrafluoroethylene membrane sewn to the skin edges is described. This should be done daily using aseptic technique.26,28
Renal disturbancesAcute renal failure is common after TAH implantation due to decreased secretion of atrial natriuretic peptide, although in most cases it evolves favourably.19,24 Therefore, diuresis and renal function should be monitored. In some cases, if there is oliguria, without decreased TAH flows, tamponade or hypovolaemia, use of synthetic atrial natriuretic peptide may be beneficial.19,27 In several of the studies reviewed, patients required extrarenal clearance procedures.19,24
Nutritional disturbancesPatients may have nutritional deficiencies due to previous HF and present with poor appetite, low weight, and decreased albumin and pre-albumin levels. It is therefore necessary to initiate oral nutrition early as it is crucial for recovery.20,26 Assessment by a nutritionist is recommended and a low-sodium, high-calorie, high-protein diet with supplements should be given.26 It may also help to present meals in an appealing way, or to administer appetite stimulants.16
Impaired physical mobilityAlthough there are no specific guidelines, pre-established protocols have been observed to provide good results.30,31
Physical rehabilitation and early ambulation help prevent muscle atrophy, respiratory complications, and risk of infection, leading to better outcomes after transplantation.20,26,30 Physical exercise can improve and reverse symptoms, complications, and survival in patients with heart failure.32 Respiratory physiotherapy helps to train the respiratory muscles, increasing lung capacity, favouring recovery.20,32 Brown et al.33 describe the implementation of a six-session programme in a patient after TAH implantation. It lasted 4 weeks with progression of intensity and duration individualised according to the presence of subjective symptoms, haemodynamic data, and according to the recommendations for the artificial heart. Over the six sessions, the patient tolerated the exercise well, showed good tolerance, had fewer adverse effects and improved pedalling distance.33
Physical therapy should be guided by physiotherapists30–32 and be progressive in both activity and duration. The sequence can be passive and active mobilisation in bed, transfer from bed to chair, cycling and ambulation.30–32 Electrostimulation can sometimes be used to acquire greater muscle strength.32
Pain management related to surgery is important for comfort and to improve recovery and healing.20,26 Pain, driver parameters, and signs and symptoms of exercise intolerance need to be monitored.30–32 We found no studies on which therapy or which techniques may be most effective in pain control.
Sleep-rest disturbancesPatients and their families report that the noise from the device is disturbing22,26 and sometimes have difficulty falling asleep. This can cause fatigue, difficulty participating in physical therapy and anxiety. It is important that healthcare professionals make an effort to group activities and minimise interruptions to facilitate the patient's sleep and rest.26
Psychological aspectsPatients often experience a wide range of feelings associated with their health status, from concern about the transplant, denial, fear, depression or anger, to acceptance. Some also become dependent on the TAH and worry about changes in body image, constant sounds, and/or alarms, and the risk of associated complications.26 Others are able to carry out activities of daily living without fatigue, achieving an improvement in their quality of life, which gives them hope.34
A good relationship with professionals, contact with family and loved ones, listening to music or other pleasurable activities are strategies that can help patients to cope better with the process.26,34
Emotional support of the family should not be forgotten, as they often experience stress, social deprivation, and go through complicated psychological processes.22,26,34
Therefore, a multidisciplinary team must be involved that covers all the needs and concerns of the patient and family.26
Educating the patient and family in self-careEducation in the following aspects is essential: sternotomy and cannulae orifice care, driver management, emergency situations, and adherence to treatment and exercise.14,20–22,25,31,32
It is also important for the patient to regularly monitor temperature, weight, blood pressure, and know how and when to contact the physician in charge.16,22
The educational process starts the moment the patient leaves the intensive care unit. Before discharge, patients and relatives should be trained in the daily management and care of the device.14,20,22,25
There is a large gap regarding the educational process and its evaluation. However studies by Demondion et al.22 and Friedline et al.25 emphasise the combination of theoretical and practical sessions using simulation. They also highlight that the patient and family should take a written and practical test, to demonstrate confidence in managing the device.
In this sense, Presti and Crenshaw state that the existence of a nurse trained in mechanical support or an advanced practice nurse is essential in the education and follow-up of these patients and their families, to reduce complications and hospital readmissions.21
Home follow-upThe choice of hospital discharge time and the ability to cope with the complexity of the device are essential to prevent complications. In fact, in dependent patients without help at home, this process is not possible.22
Requirements for discharge include haemodynamic stability, absence of intravenous medication and being connected to the Freedom driver, and not requiring frequent readjustments.20,22,25
Once the patient has become an outpatient, it is recommended that a specialist nurse is in charge of follow-up. The patient will also be consulted periodically for monitoring and assessment for possible complications.22
The hospital readmissions described are due to infectious complications, the need for transfusions, device-related problems, hypertension, and neurological impairment.22,26 Some of these complications require urgent transplantation.22
DiscussionThis review was conducted to respond to the need to provide standardised care for patients undergoing TAH implantation in our hospital. Because of the absence of specific nursing studies, we decided to conduct a scoping review with the aim of providing an overview of postoperative management and nursing care after TAH implantation as a bridge to transplantation, to gain more in-depth knowledge of the device, its management, possible complications, and related care.
The evidence highlights as key aspects the management and monitoring of the TAH, care to prevent infection, maintenance of renal function, adequate nutrition, haematological status, early mobilisation, sleep-rest preservation, attention to the psychological dimension, and education of the patient and family.
We found discrepancies were found in relation to anticoagulation, device driveline dressings, or early mobilisation and rehabilitation. These aspects highlight the importance of further studies to determine guidelines for the care of patients with a TAH and their families.
Furthermore, the quality of evidence ranged from low (12 publications)7,14–19,21,24,27–29 to very low (10 publications).2,20,22–26,30–33 None of the studies were rated with a moderate or high level of evidence, as the findings come from retrospective studies, description of experiences and/or clinical cases, and literature reviews without a systematic methodology. Nevertheless, they are the best available evidence to determine what nursing care should be provided to patients with a TAH and their families, therefore, we consider that these findings can help towards improving care in practice. Therefore, we recommend that intervention-type studies be conducted to obtain results that help to reduce variability in practice.
Considering the specificity and complexity of the care of the TAH patient, the importance of a multidisciplinary approach and the development of evidence-based strategies to help these patients and their families cope with physical and psychosocial problems is highlighted.14,20,22,25,26,29 The multidisciplinary approach is widely supported in the literature because it improves patient outcomes.34
In this regard, the involvement of the nurse is evident as they are responsible for monitoring, device management, the detection and management of complications, and for providing emotional support and education to the patient and family.20 In fact, in a study by Savage et al.,34 patients reported that the support of the nurses who had been part of their experience had made them feel more confident and capable in coping with the TAH implantation.34 Therefore, having adequate education and training helps the nurse to provide specialist care and become a vital element in the process.
This review has some limitations, such as the inclusion of studies only in English and Spanish. In addition, the paucity of evidence related to nursing care made it necessary to consider all types of studies that have implications for nurses.
ConclusionsIn this scoping review, we observed multiple divergences in patient care, such as anticoagulation-antiaggregation therapy, open chest management, daily cannula care, and physical mobilisation exercises. Further interventional research is therefore needed to fill this gap and to identify the most appropriate care for patients with a TAH and their families.
The complexity of TAH implantation, and the multiple related complications that may arise during the postoperative process, necessitate standardised and multidisciplinary management of patients who have undergone TAH implantation. It is also crucial to train the entire healthcare team, in which nurses acquire autonomy and involvement in decision-making and develop competencies to address the physiological and psychosocial needs of the patient and family.
There is a gap in both the national and international literature on the nursing care of patients with TAH. However, the results of this scoping review can be used as a basis for future studies related to the nursing care of patients undergoing TAH implantation as a bridge to transplantation. Thus, the absence of standardised protocols raises the need for future studies to measure the effectiveness of care in patients with a TAH, which may contribute to quality multidisciplinary care and facilitate the identification of interventions for each patient, family, and setting.
Conflict of interestsThe authors have no conflict of interests to declare.