Common mental disorders (CMDs) in mental health settings show high rates of comorbidities. While semi-structured interviews are the gold standard to establish a diagnosis, there are self-report instruments such as the Psychiatric Diagnostic Screening Questionnaire (PDSQ) that aids clinicians in improving the diagnostic process in a time-efficient manner.
MethodsNetwork analysis of the 13 domains of the PDSQ was applied to a sample of 374 first-contact outpatients to identify domains of psychopathology acting as hubs and bridges of interconnections within the CMDs.
ResultsA global network densely connected with positive connections among PDSQ domains was found. The global network has four main clusters: depression-anxiety, somatoform, psychosis and substance-related domains. This network allowed for the identification of main ‘nodes’ acting as hubs favoring interconnections between dimensions and main ‘bridges’ easing the connections between clusters.
ConclusionThe network structure of the PDSQ domains might provide a complementary explanation to the high rates of comorbidity among CMDs. Moreover, our results support the relevance of the self-administered PDSQ inventory to account for a deeper understanding of comorbidities among CMDs.
Distress and suffering are cornerstone manifestations of common mental disorders (CMDs) at the first contact with the mental health system. The CMDs are not associated with the highest median societal cost per patient worldwide, such as schizophrenia disorder, but these disorders are much more prevalent and thus would contribute substantially to the total national cost in a country.1
Patients often exhibit a wide range of psychopathological symptoms and non-psychopathological conditions with varying severity, ranging from normality to subthreshold and full-blown clinical disorders. Clinicians should not only account for the quantitative differences in illness severity but also categorize symptoms within formal taxonomic systems.2 This “categorical diagnostic” problem applies to major psychiatric disorders, but it is even more severe regarding CMDs, where diagnostic entities share common phenomenological features.3 CMDs are not mutually exclusive in current classifications and the experience of a particular CMD increased notably the onset of one another CMD.4 Both factors generate a particular type of comorbidity within CMDs different from those originally proposed for medical diseases.5-7
The use of semi-structured interviews by professionals with specific training is the gold standard for diagnosing psychiatric disorders. In addition, the information of the patient by means of self-report questionnaires might help psychiatrists improve the accuracy of diagnosis mostly by reducing possible missing diagnoses and, to a lower degree, by ameliorating the risk of an incorrect diagnosis.8
The Psychiatric Diagnostic Screening Questionnaire (PDSQ) is a self-report diagnostic instrument devised to facilitate the efficiency of conducting initial diagnostic evaluations in mental health settings.9 Extensive psychometric evaluations of the PDSQ rendered good to excellent psychometric properties.9-12 In addition, the PDSQ is a multi-dimensional instrument that provides a measure of the severity of overall psychopathology as well as the quantifiable measures of 13 subscales covering most psychopathological domains in CMDs.
Network analysis may offer a novel approach to examine unanswered questions related to both comorbidity at the symptom or dimension level.13 Network analysis allows for estimating and visualizing the direct and indirect connecting pathways between dimensions with overlapping content.14
AimsThis study aims to examine the interrelationships between dimensions of psychopathology in CMDs as assessed by the PDSQ self-report questionnaire at the first contact of outpatients in mental health settings. Specifically, we focus on the general network structure of the CMD dimensions and the direct and indirect associations between PDSQ domains to reveal potential hubs with higher connections to the others.
It is hypothesized that psychopathological dimensions of CMDs show a dense network of associations. Moreover, depressive and anxiety dimensions of the PDSQ are the most strongly interconnected psychopathological domains of first contacts in outpatient mental health centers.
Material and methodsParticipantsThis study aimed to collect a consecutive sample of first-contact patients in two adult outpatient centers of the Mental Health Network of Navarra. The patients were invited to participate in the study between June 2012 and March 2016. The sample comprised 374 patients. These patients were assessed with an exhaustive protocol including diagnostic, clinical, personality and stressful event questionnaires. For this research, we used diagnostic screening data. All patients were clinically stable at the time of the assessment. A full description of the sample was reported elsewhere (Arraras et al., submitted). The inclusion criteria were submission to a first appointment and collaboration with the study. The exclusion criteria included patients who were unable to answer a questionnaire due to sensory disabled conditions or impaired cognitive function.
AssessmentsThe diagnosis of patients was ascertained by research psychiatrists using all available information and including external information from a close relative. The Mini-International Neuropsychiatric Interview-Plus (MINI-Plus 5.0.0) was administered at the first interview.15 The Mini-Plus is a brief structured interview for the diagnosis of major axis I psychiatric disorders according to the DSM-IV diagnostic criteria.16,17
The Psychiatric Diagnostic Screening Questionnaire (PDSQ)9 was administered to patients in the time before the first appointment, and doubts about the questionnaire were solved by the professionals. The PDSQ is a self-report questionnaire designed to screen for the diagnosis of CMDs in outpatient mental health settings. It comprises 125 questions that allow for the quantification of 13 subscales for the most common mental health problems as follows: major depressive disorder (MDD), posttraumatic stress disorder (PTSD), bulimia (Bul), obsessive-compulsive disorder (OCD), panic disorder (PD), psychosis (Psy), agoraphobia (Ago), social phobia (Soc), alcohol abuse/dependence (Alc), drug abuse/dependence (Dru), generalized anxiety disorder (GAD), somatization disorder (Som), and hypochondriasis (Hyp). Questions are formulated covering three different time frames: the past two weeks, six months before the evaluation, and two questions about having ever experienced or witnessed a traumatic event.
Participants answered each item with a yes/no (1 and 0 score, respectively) response. The PDSQ subscales were calculated by summing the individual items that constitute each subscale as raw total scores, where a higher score indicates a higher number of symptoms. Moreover, the PSDQ provides cutoff scores for each subscale to calculate probable DSM-IV disorder for each individual and results in dichotomous variables indicating the presence or absence of the DSM diagnoses. The PDSQ was validated in Spanish.18
Statistical analysisDue to the extension of the PDSQ questionnaire, we explored possible missing responses by calculating the average percentage of PDSQ items completed in the PDSQ.
The network analysis approach (NA) allows us to examine complex patterns of pairwise interactions between psychopathological domains and to ascertain to what extent they are associated with each other.13,19
First, we examined the network structure of the 13 psychopathological domains of the PDSQ domain diagnoses. To estimate an interpretable network, graphical LASSO using the extended Bayesian information criterion (EBIC) was employed. We used the qgraph20 and EGAnet21 R packages. The exploratory graph analysis (EGA) not only displays the network structure with nodes and edges but also processes the walktrap algorithm, which estimates the number of latent communities underlying the multivariate data using undirected network models. Centrality indices (strength/degree, closeness and betweenness) were calculated to study the importance of each node to the network. To determine the accuracy and stability of the centrality indices, the correlation stability (CS) coefficients were obtained as a robustness measure.
Centrality indices provide information about how important a node is, but to allow for estimation of nodes that increase the risk of comorbidity to other domains, bridge centrality estimators are needed.22 The networktools R package was used to calculate bridge centrality statistics.23
Sensitivity analysisTo examine the robustness of our network analysis on the severity of psychopathological domains and to reduce the loss of information related to the specific analysis, we performed a confirmatory factor analysis (CFA) with maximum likelihood estimation to test whether the clusters of the resulting network were mirrored as the best fitting model in CFA. Implicitly, we intend to explore whether results from CFA might lead to different final interpretations or conclusions.24
CFA results reported several indices of model goodness of fit, such as the model chi-square test for nested models, the root mean square error of approximation (RMSEA), the comparative fit index (CFI), and the nonnormed fit index (NNFI). The model chi-square test compares the EGA 4-factor structure to models comprising 1, 2, 3 and 5 factors. Moreover, to evaluate and compare the goodness of fit between models with different numbers of factors, we considered the following indicators to have good fitness: RMSEA <0.06 and CFI and NFI > 0.95.25
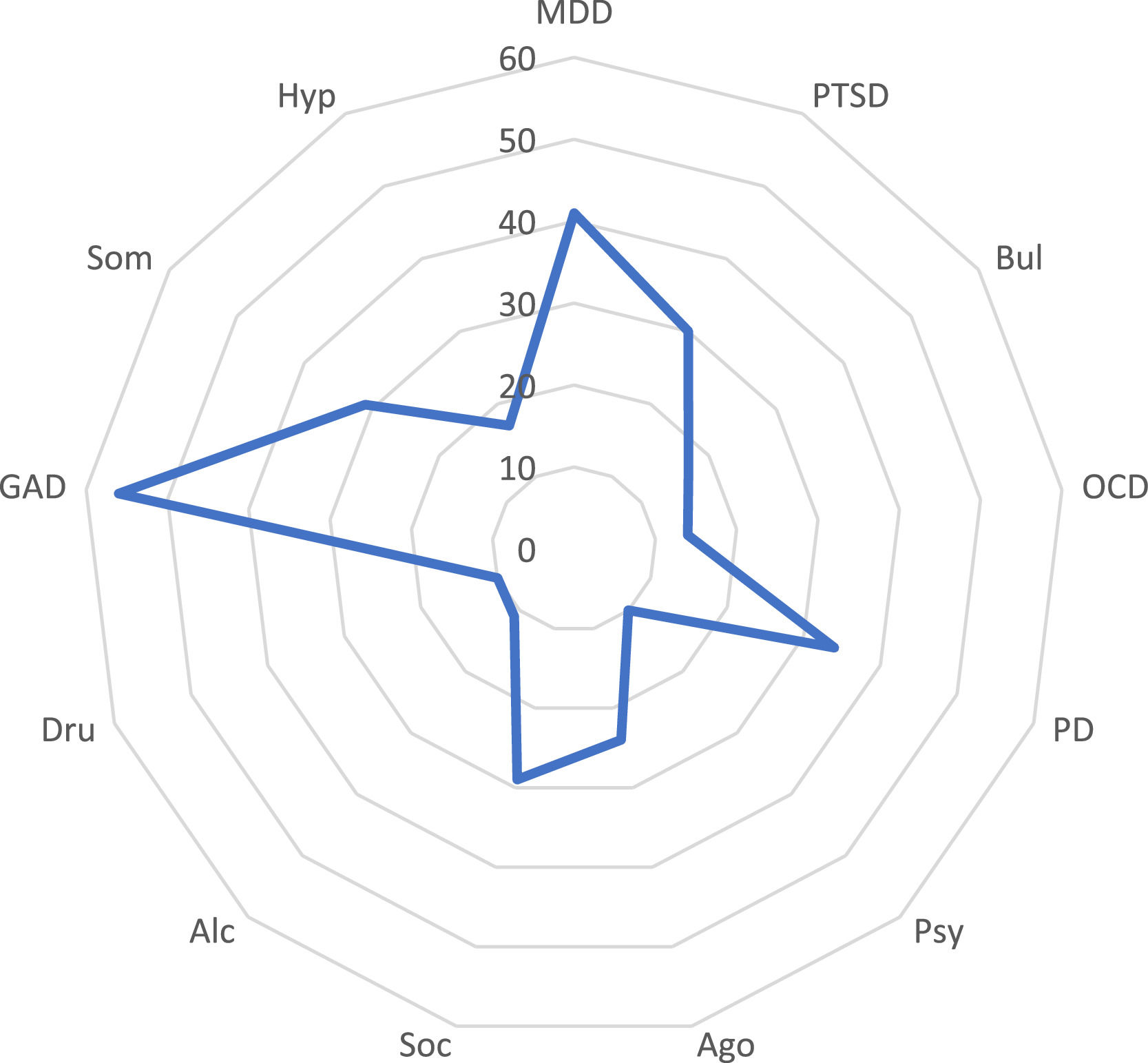
ResultsCharacteristic of the sampleOf the 374 subjects, 59.7% were women. The mean age of the sample was 40.2 years (S.D. = 13.9), and 10.7% of the sample had less than compulsory education. DSM-IV diagnoses as evaluated by the MINI-Plus interview and DSM diagnoses resulting for the application of the defined PDSQ cutoff scores are shown in Table 1. Patients showed a wide display of DSM-IV diagnoses, and the high rates of diagnoses were major depression (33.3%), generalized anxiety disorder (18.7%), panic disorder (18.1%), alcohol abuse (12.5%), drug abuse (10.1%) and somatization disorder (10.1%). Moreover, there were 154 patients (41.1%) with other DSM IV diagnoses that are not included in the MINI-PLUS interview, such as dysthymic disorder (6.1%), adjustment disorder (19.9%) and “other conditions that may be a focus of clinical attention” (5.8%). 8.8% patients received a diagnosis code in the MINI-PLUs as “suicidal risk” patients (8.8%) (Table 1). To account for the severity of symptomatology, PDSQ psychopathological domains are shown in Fig. 1 by averaging the total score in each domain by the number of items.
Demographic and diagnostic characteristics of the sample.
| Patients (n=374) | |||
|---|---|---|---|
| Age | 40.2±13.9 | ||
| Gender (M/F) % | 40.3/59.7 | ||
| Education (%) | |||
| Less than compulsory | 10.7 | ||
| Compulsory | 38.4 | ||
| Secondary | 36 | ||
| University | 14.9 | ||
| Socioecon. status (%) | |||
| Low | 41.1 | ||
| Medium low | 29.9 | ||
| Medium | 18.9 | ||
| High | 10.1 | ||
| Cohabitance (%) | |||
| Living alone | 11.2 | ||
| Living with family | 80.3 | ||
| Shared home | 7.7 | ||
| Residence | 0.8 | ||
| Country of birth (%) | |||
| Spain | 82.4 | ||
| Other | 17.6 | ||
| Diagnoses (%) | DSM-IV* | PDSQ | κ |
| Major depressive disorder | 33.3 | 53.3 | 0.44 |
| Post-traumatic stress disorder | 8.8 | 44.8 | 0.21 |
| Panic disorder | 18.1 | 35.2 | 0.26 |
| Agoraphobia | 9.3 | 37.1 | 0.23 |
| Social phobia | 13.3 | 50.1 | 0.23 |
| Obsessive-compulsive disorder | 5.6 | 47.7 | 0.12 |
| Somatization disorder | 10.1 | 46 | 0.18 |
| Generalized anxiety disorder | 18.7 | 42.1 | 0.22 |
| Bulimia | 1.3 | 10.9 | 0.20 |
| Hypochondriasis | 6.4 | 31.7 | 0.23 |
| Psychosis | 6.1 | 28.5 | 0.23 |
| Alcohol abuse | 12.5 | 23.5 | 0.46 |
| Drugs abuse | 10.1 | 22.9 | 0.51 |
| Other diagnoses⁎⁎ | 41.1 | – | |
Average total score in each PDSQ psychopathological domain.
MDD: Major depressive disorder. PTSD: Posttraumatic stress disorder. Bul: Bulimia. OCD: Obsessive compulsive disorder. PD: Panic disorder. Psy: Psychotic disorder. Ago: Agoraphobia. Soc: Social phobia. Alc: Alcohol abuse. Dru: Drug abuse. GAD: General anxiety disorder. Hyp: Hypochondriasis
The percentage of nonrespondent items was lower than 5%.
Internal consistency estimates (Cronbach's coefficient alpha) exceeded 0.80 for all but 3 subscales (obsessive-compulsive 0.73; psychosis 0.77; and somatization 0.76), with a mean value of 0.84.
To account for the degree of concordance of the PDSQ subscales with the diagnostic reference pattern in the MINI-Plus interview (DSM-IV criteria), Cohen's kappa coefficients were calculated. The degree of concordance with the DSM-IV diagnostic criteria of the 13 PDSQ subscales using the original cut points were lower than values considered good, ranging between κ = 0.12 and κ = 0.44.26
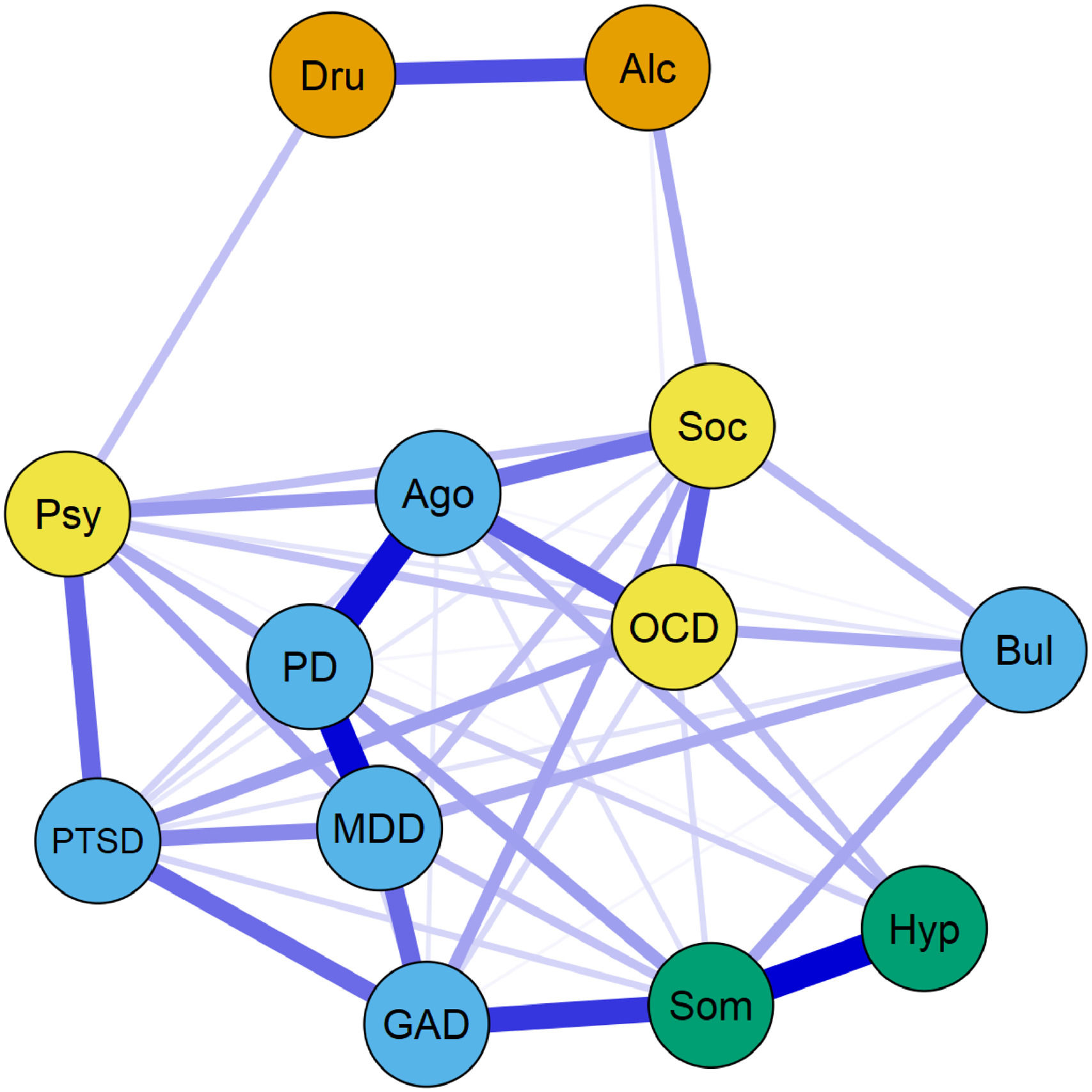
Network structure and analysis of the PDSQ diagnosesThe overall network density was 60.3% (47/78 possible interconnections), indicating that the CMD domains were highly connected, either directly or indirectly, via other symptoms in the network. Most PDSQ domains showed between 3 and 8 interconnections.
The generated network showed that 9 out of the 11 nodes were generally highly and positively interconnected suggesting that there may be a global factor of severity potentially affecting the network. The 2 nodes of substance abuse disorders showed strong interrelationships between themselves, though with weak associations regarding other CMDs (Fig. 2).
Network structure of the PDSQ psychopathological domains.
MDD: Major depressive disorder. PTSD: Posttraumatic stress disorder. Bul: Bulimia. OCD: Obsessive compulsive disorder. PD: Panic disorder. Psy: Psychotic disorder. Ago: Agoraphobia. Soc: Social phobia. Alc: Alcohol abuse. Dru: Drug abuse. GAD: General anxiety disorder. Hyp: Hypochondriasis. Som: Somatization disorder.
Four main and highly connected clusters were evidenced in the network analysis. The 4 main clusters and pertaining domains were: depression-anxiety (including MDD, GAD, PD, PTSD and Bul); somatoform (including Som and Hyp); psychosis-obsessive (including Psy, Soc, OCD); and substance-related (including Alc and Dru) clusters. The number of connections was greater between symptoms of the same cluster than across other clusters or other psychopathological domains.
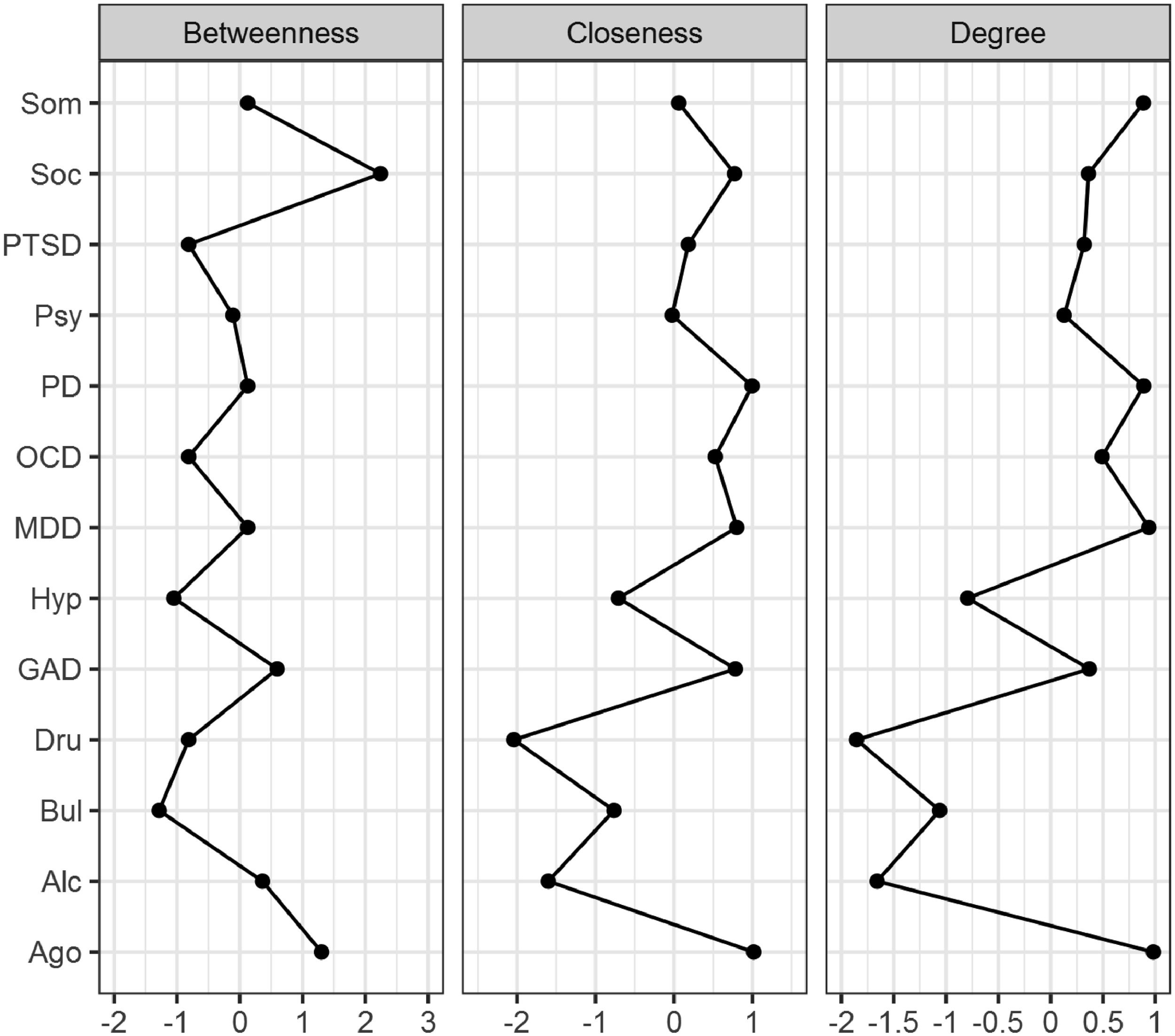
Four nodes, 3 of the depression-anxiety cluster (MDD, PD and Ago) and 1 of the Somatoform cluster (Som) showed the higher values of node strength. These 4 nodes seem to be the main hubs for intra and intercluster interconnections of dimensions because they have the highest local influence of other nodes within the network (Fig. 3). The Ago and Soc subscales showed the highest betweenness, suggesting that both nodes quantitatively showed the highest number of shortest paths between two other nodes that crossed the node, acting as mediators of traffic in different areas of the network. The Ago, GAD, MDD, PD, and Soc subscales obtained the highest closeness, indicating that they are the nodes that best indirectly connected to other nodes (Fig. 3).
Centrality indices of the PDSQ network.
MDD: Major depressive disorder. PTSD: Posttraumatic stress disorder. Bul: Bulimia. OCD: Obsessive compulsive disorder. PD: Panic disorder. Psy: Psychotic disorder. Ago: Agoraphobia. Soc: Social phobia. Alc: Alcohol abuse. Dru: Drug abuse. GAD: General anxiety disorder. Hyp: Hypochondriasis
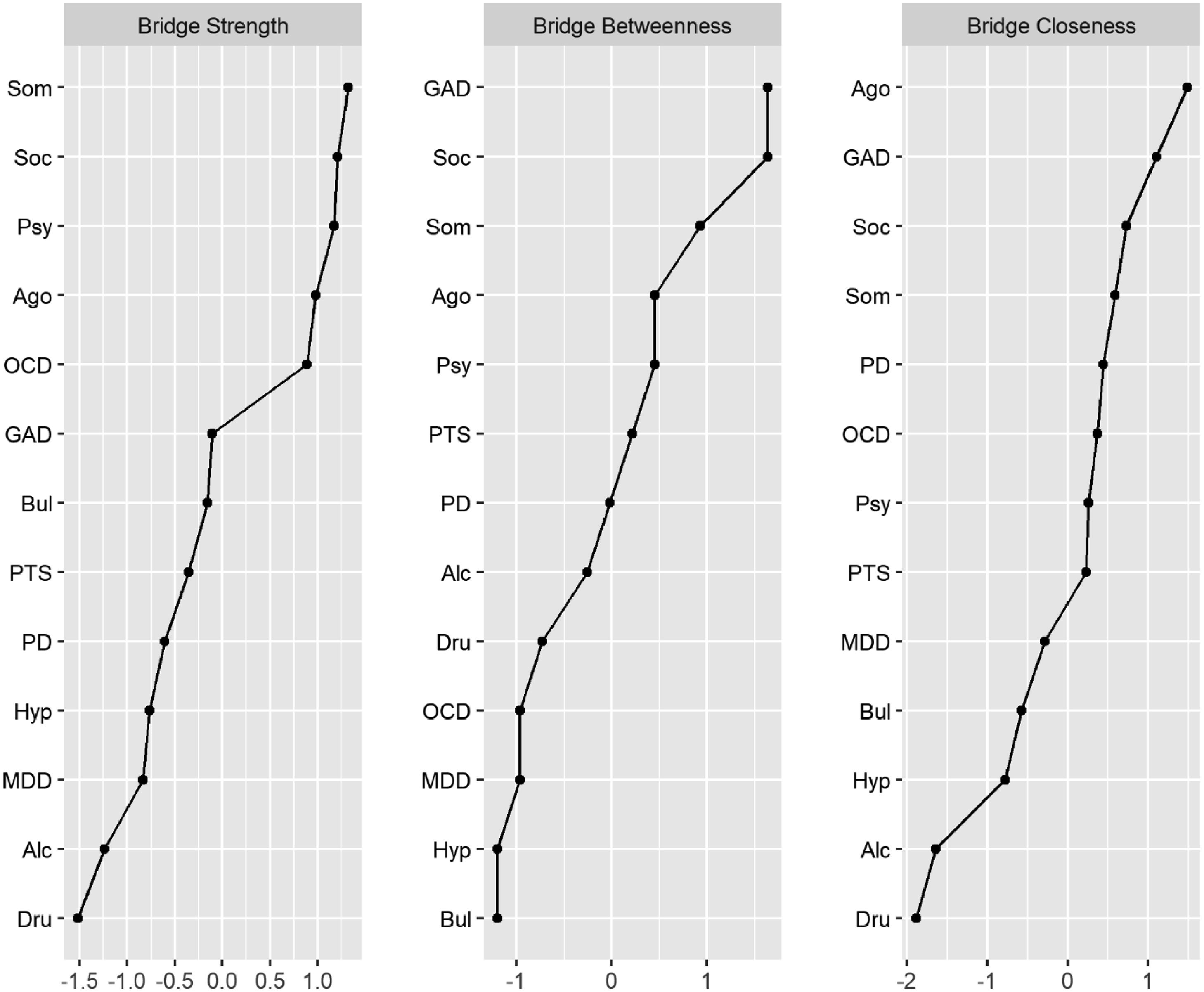
One node from somatoform cluster (Som), 3 from psychosis-obsessive cluster (Psy, Soc and OCD) and 1 from depressive-anxiety cluster showed the higher values in “bridge strength”. These results suggest that they are the main hubs for intercluster interconnections since “bridge strength” is a measure of a node's total connectivity with other clusters (Fig. 4).
Bridge centrality indices of the PDSQ network.
MDD: Major depressive disorder. PTSD: Posttraumatic stress disorder. Bul: Bulimia. OCD: Obsessive compulsive disorder. PD: Panic disorder. Psy: Psychotic disorder. Ago: Agoraphobia. Soc: Social phobia. Alc: Alcohol abuse. Dru: Drug abuse. GAD: General anxiety disorder. Hyp: Hypochondriasis. Som: Somatization disorder.
Stability was assessed by means of the correlation stability coefficient (CS coefficients). Higher scores denote that a greater number of observations can be dropped without significant changes in the magnitude of centrality estimates.27 Edge-weight estimates for strength and closeness were reliable and accurate since bootstrapped 95% CIs were quite narrow. Node strength had a CS coefficient of 0.59 and closeness of 0.44, suggesting that the network was sufficiently stable and that a greater number of observations could be dropped without significant changes in the magnitude of centrality estimates. However, CS for betweenness was lower, 0.05, not reaching the minimum threshold of 0.25, partly reducing the strong support of stability reached by the two other indices and inducing caution in the interpretation of the results (Suppl Figs. 1 & 2).
Sensitivity analysisThe CFA model comprising the EGA 4-factor network model demonstrated excellent goodness of fit (x2 = 63.86, df= 59, RMSEA = 0.015, CFI = 0.998, NNFI = 0.997). CFAs with a lower number of factors showed lower goodness-of-fit indices than the EGA 4-factor model, and a 5-factor model also achieved slightly worse goodness of fit (Supplementary Table 1).
DiscussionMain findingsThis study presented the complex network structure of psychopathological domains in first-contact outpatient mental health settings, as ascertained by means of the PDSQ self-report questionnaire. To the best of our knowledge, this is the first report to investigate psychopathological domains of CMDs using network analysis.
We found that self-reported psychopathological domains of CMDs provided a global network densely connected with positive connections among PDSQ domains and without any negative interconnection. The global network of CMDs displayed four main psychopathological clusters: the first comprising depression (MDD), anxiety (GAD, PD and Ago), PTSD and Bul dimensions; the second including somatization (Som) and hypochondriasis (Hyp) dimensions; the third made up psychosis (Psy), social phobia (Soc) and obsessive dimensions (OCD) dimensions; and the fourth comprising alcohol (Alc) and substance abuse (Dru) dimensions. This EGA network structure achieved high goodness of fit in the sensitivity analysis based on CFA models (EGA 4D model in Supplementary Table 1).
In agreement with our hypothesis, some of the nodes related to depression and anxiety, such as PD, MDD and Ago exhibited high degree, suggesting their relevance for intra- and intercluster connections (Fig. 3). Unexpectedly, Som node showed also a strong degree. Thus, these 4 nodes seem to be the main hubs since they ease the interconnections among psychopathological dimensions. And high scores in any of them might potentiate the increase of severity in the remaining nodes and consequently the degree of network comorbidity. Moreover, the examination of bridge strength between clusters revealed that Som is a main hub for depression and anxiety dimensions (cluster 2) and that the 3 domains of the third cluster (Soc, Psy and OCD) showed the highest interconnections with psychopathological domains of the other three clusters (Fig. 4). Likewise, Ago plays also a relevant role for the interconnections with the three other clusters. In sum, these 4 bridge hubs allowed for increasing extracluster severity and might account for the high rates of comorbidity among psychopathological domains of CMDs.
The substance abuse cluster remained relatively isolated within the CMDs network, showing weak connections toward social phobia and bulimia in the case of alcohol abuse and only toward psychosis in the case of the drug abuse domain.
Both the “key strength” nodes and the “key bridge strength” PDSQ nodes highlight their value as “core” domains and main hubs of CMDs for interconnecting nodes and clusters of PDSQ dimensions. Thus, comorbidity patterns could be better explained by the preferential connections established between these “core” dimensions and the rest of the psychopathological domains,28 and they may play a role in the development and maintenance of comorbid mental disorders.22
These properties of nodes and clusters of the PDSQ network are in agreement with robust findings on comorbidity of CMDs.4 Strong evidence from large epidemiological studies found that comorbidities among CMDs are much higher than would be expected by chance.29,30 Moreover, two consistent findings in the literature are that the presence of one of the CMDs is a risk factor for developing the other31 and that comorbidity within CMDs is associated with a higher illness severity, chronicity, and impairments in everyday life.32
New dimensional approaches have led researchers to search for common underlying spectra of CMDs, mainly based on factor analysis, to find more parsimonious means of addressing comorbidities than categorical diagnosis.33-36 Achenbach, Edelbrock37 achieved a cornerstone achievement in research by applying a quantitative approach to the classification of childhood psychopathologies. Indeed, Achenbach's group proposed a new way to characterize childhood disorders into two dimensions, namely, “internalizing” (including anxious and depression symptoms) and “externalizing” (including aggressive, delinquent, and hyperactive-impulsive symptoms).37,38
This quantitative endeavor to reformulate psychopathology and nosology achieved renewed interest in 2015 when the Hierarchical Taxonomy of Psychopathology (HiTOP) was established. The HiTOP system provides a comprehensive psychopathological system that conceptualizes psychopathology as a set of dimensions organized into increasingly broad, transdiagnostic spectra based upon bi-factor modelling.39,40 However, the network analysis approach allows to explore whether psychopathological dimensions of CMDs might be accomplished in a dynamic network of interconnections regardless of whether they are significantly correlated.
Our CMDs network is in agreement with the HiTOP model since depression and anxiety cluster of CMDs (internalizing dimension) are clearly detached from alcohol and drug abuse clusters (externalizing dimension). Though our sample was not large enough to differentiate all subfactors within the internalizing dimension, the nodes of our depression and anxiety cluster are main domains of distress and fear subfactors of the HiTOP hierarchy.41 Moreover, as our sample was made up of first-contact appointments with mental health centers, the prevalence of full-blown psychosis was very low, precluding the identification of a ‘thought’ dimension.
The analysis of the CMD network might allow for inferences on the severity of clinical domains, might have implications for prognosis and might help in formulating hypothesis regarding the underlying connections between and among domains. For instance, intra-cluster connections within the first cluster is in agreement with the high possibility of co-occurrence of MDD and PD, GAD and PTSD, and it could explain the increase the severity of GAD domain in a MMD patient after recrudescence of their symptomatology. This is in alignment with the introduction of the anxious distress specifier for Depressive disorders in DSM-5.42
Extra-cluster bridging may provide explanations for prognosis. For instance, patients the exacerbation of somatoform symptomatology (Som node) may pave the way to an increase of depressive symptomatology (MDD domain), which will led to a more severe course.43
Finally, the network analysis might allow for inferential hypothesis regarding common causes within clusters domains. For instance, the strong interconnections between major depression and generalized anxiety disorder are in agreement with results from studies reporting a common liability influenced by the same genetic factors.44,45
Use of the PDSQ in clinical practiceThe PDSQ is a reliable and valid measure of multiple DSM-IV disorders.46 The use of self-report questionnaires in clinical practice might be hampered by drawbacks derived from patient's sources, such as personal bias, lack of insight, the tendency to give socially acceptable answers or to respond in the same way to all questions. There are also potential biases from the questionnaire itself, such as misunderstanding of statements, or ceiling- or floor-effect scorings. However, self-report questionnaires not only are less-time consuming for practitioners but also they might provide complementary and valious information not gathered in clinical interview and they are non-expensive and relatively easy to obtain.47,48
LimitationsOur study has a cross-sectional design that precluded any basis to establish causal relationships or dynamic interactions between psychopathological domains. However, the strong dependencies between PDSQ diagnoses might suggest that psychopathological domains of CMD diagnoses are not only highly interrelated but also that such relationships may operate in a causal way.49,50 Further longitudinal studies are warranted to examine whether the activation of a specific psychopathological domain will lead to the stimulation of its neighboring domains and to calculate the specific strength of activation for each connection.
The results from this study are sample and setting dependent, and generalization to other mental health settings should be taken cautiously. However, the prevalence of DSM-IV disorders based on the PDSQ cutoff points was within the range of those in the literature for outpatients. Moreover, the low agreement between MINI and PDSQ diagnoses introduced an extra “noise” in the reliability of diagnostic process of psychiatric disorders derived from the use of two different sources of information (clinician's and patient's ratings).26
It is also important to note that the PDSQ provides assessment for a wide range of CMDs but not all possible psychiatric disorders.10 In addition, the PDSQ subscales were validated against the DSM-IV but not regarding the DSM-5 though, many of the basic criteria have remained largely unchanged.
Node strength and closeness were sufficiently stable, demonstrating the stability of our network.27 However, the low betweenness centrality might suggest that although all PDSQ nodes are well interconnected with each other, they use lower shortest paths of interconnections between psychopathological domains by establishing the connection through distant psychopathological domains in the network.
Some PDSQ items are very similar, and they scored for more than one subscale. These similarities and score overlapping might have affected the resulting network by producing an inflation of the estimates of edge weights and centrality.
ConclusionsIn summary, the resulting network provides an alternative and complementary explanation to the high overlapping of symptoms and dimensions and to the comorbidity problem in CMDs.51,52 Moreover, our results added complementary evidence to the utility of the PDSQ as a self-report questionnaire, not only aiming at screening but also to quantitative assessment of psychopathological domains of CMDs in practice.
FundingThis work was supported by the Government of Navarra (grant 17/31 and 18/41) and the Carlos III Health Institute (FEDER Funds) from the Spanish Ministry of Economy and Competitivity (16/02148 and 19/1698).
Data availability statementThe data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Author contributionsM.C. designed and conceptualized the study, prepared the data, contributed to the implementation of PDSQ and drafted the manuscript. J.A. implemented the PDSQ and revised the manuscript. G.G. prepared and analyzed the data and revised the manuscript. V.P. designed and conceptualized the study, secured funding and revised the manuscript.
Ethical considerationsThis study was approved by the ethics committee of the Regional Health Service of Navarra and written informed consent was obtained from all study participants or their legal representatives.
We thank all participants of the study and their families.