We present the case of a 74-year-old female patient with a prior history of atrial fibrillation and chronic pancreatitis who attended A&E due to a two-month history of recurrent syncope. She exhibited jaundice and mild diffuse abdominal pain. The examination revealed sinus tachycardia and melaena upon digital rectal examination. The blood tests revealed moderate microcytic anaemia (9.2g/dl).
An emergency gastroscopy was performed, which showed a Forrest III gastric ulcer with inflammatory edges. The follow-up blood tests showed complete cholestasis (GGT=1,303U/l, AP 725U/l, TBIL=6.65mg/dl), with elevated cytolytic enzymes (GOT=190U/l, GPT 137U/l). Amylase and lipase were normal, as were all other values, except the complete blood count that continued to show anaemia (Hb=9.3g/dl), so intravenous iron therapy was started. The diffuse abdominal pain, although mild (3/10 on the VAS), persisted despite medical treatment.
Given the clinical suspicion of choledocholithiasis, an abdominal ultrasound was performed that revealed dilation of the extrahepatic and intrahepatic bile duct with a common bile duct of 14mm and doubtful choledocholithiasis. An ERCP was performed, which confirmed dilation of the bile duct without any filling defects and without trawling any gallstones with a balloon. A protruding papilla was also observed with macroscopically normal mucosa, from which biopsies were taken.
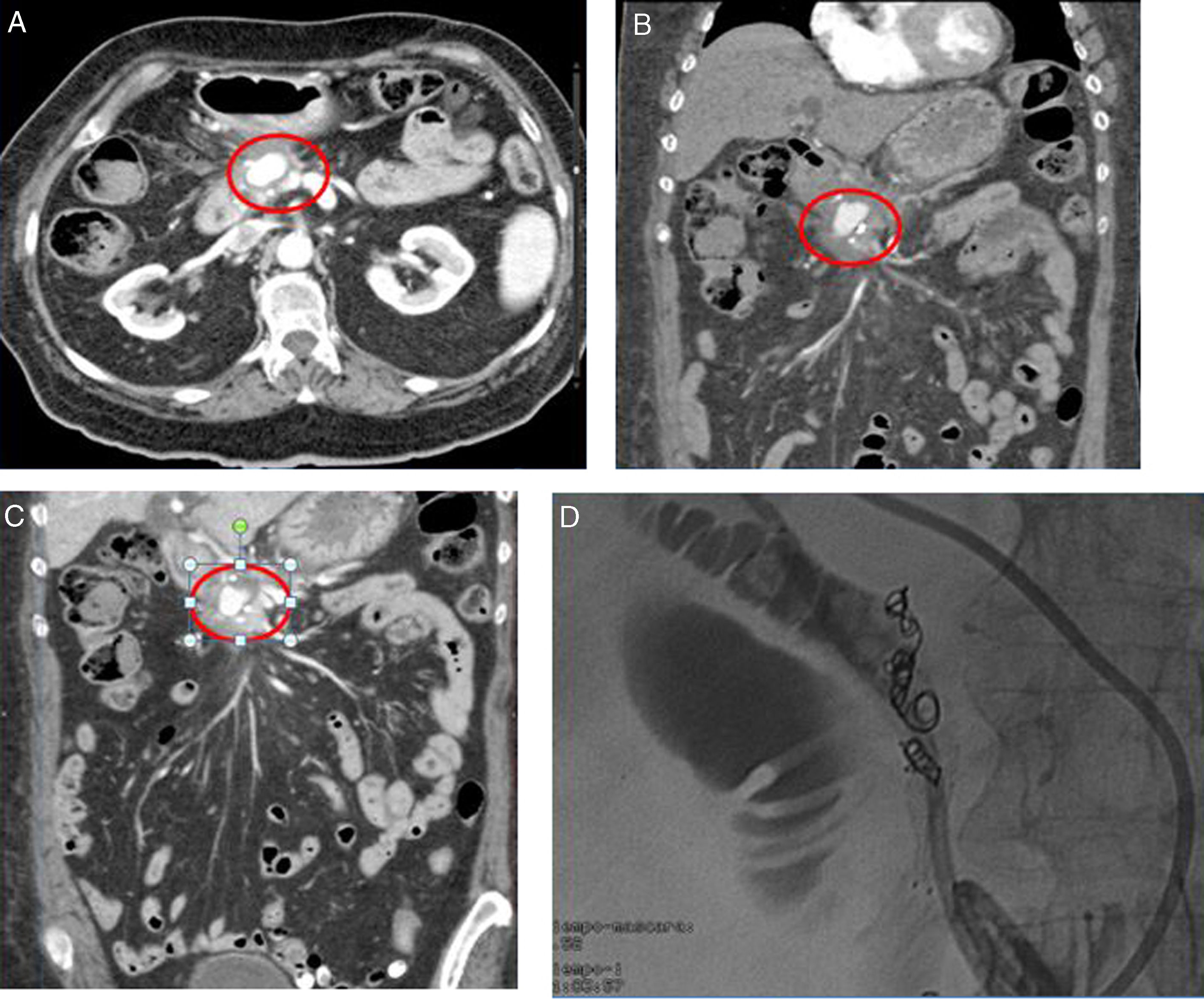
Given the suspicion of ampullary neoplasm, an abdominal contrast CT scan was conducted that confirmed a diagnosis of a periampullary pseudoaneurysm of the superior pancreaticoduodenal artery measuring 2.4cm in diameter, which compressed the distal bile duct and caused an impression on the ampullary region (Fig. 1).
Finally, the biopsies obtained confirmed nonspecific reactive inflammation and ruled out malignancy.
With the final diagnosis of pseudoaneurysm of the gastroduodenal artery with compression of the bile duct in the ampullary region, it was treated with coil embolisation combined with drainage placed by percutaneous cholangiography to alleviate the distension of the bile duct until the pseudoaneurysm had shrunk, with its removal scheduled for discharge (Fig. 1).
The patient's blood test results gradually improved, with peak bilirubin values of 10.5mg/dl returning to normal. Haemoglobin levels also improved to 12.7g/dl.
Although vascular complications secondary to chronic pancreatitis are very rare, their true incidence and prevalence are difficult to estimate and may be as high as 10%.1 The incidence of bleeding following pseudoaneurysm rupture in chronic pancreatitis is estimated to be 3.2%. The arteries most commonly affected are the splenic artery and the left gastric artery, followed by the gastroduodenal artery, the superior mesenteric artery and the hepatic arteries themselves.2 Pancreatic pseudoaneurysm is primarily associated with pancreatitis whose course involves the formation of pseudocysts. It has also been associated with hepatobiliary surgery.
The rupture of a pancreatic pseudoaneurysm is the most common cause of bleeding in acute and chronic pancreatitis, accounting for up to 61% of all cases.
Several aetiopathogenic theories to explain pseudoaneurysms secondary to chronic pancreatitis have been postulated, which include the activation of intrapancreatic enzymes and ischaemic processes leading to separation of the internal elastic lamina.3
Obstructive jaundice caused by the extrinsic compression of the bile duct is another form of presentation of pseudoaneurysms. However, this presentation is extremely rare. In the literature review we performed, we were only able to find isolated case reports.
Diagnosis should be confirmed by angiography or contrast CT scan to show arterial dilation and its association with neighbouring structures, in this case the bile duct.4
The recommended treatment is embolisation performed by an interventional radiologist. This may involve the use of coils or the placement of a stent, which isolates the pseudoaneurysm from the vessel lumen to reduce the pressure exerted on it. Studies that have assessed the efficacy of treatment with coils have found a high rate of resolution and an acceptable rate of complications, making it a less aggressive alternative to surgery.5
Please cite this article as: Casas Deza D, Gotor Delso J, Gascón Ruiz M, Bernal Monterde V, Jimeno Ayllón C, Gracia Ruiz M, et al. Obstrucción biliar secundaria a seudoaneurisma de la arteria gastroduodenal. Una inusual forma de presentación. Gastroenterol Hepatol. 2019;42:384–386.