Pyoderma gangrenosum (PG) is a neutrophilic inflammatory disease of unknown aetiology. Neutrophilic inflammatory infiltrate, its association with immune-mediated disease and its response to immunomodulatory drugs raise suspicion of an immune abnormality. Furthermore, exacerbation or onset of new lesions with minor trauma (pathergy phenomenon) has been reported in 16.3% of cases.1
It is associated with systemic diseases in 86% of patients, with inflammatory bowel disease being the most common (17.6%) and association with solid neoplasms the rarest (7.4%).1
Peristomal PG (PPG), a rare variant, is more common in women (20–50 years of age)2 and rarely associated with colorectal carcinoma,3,4 as in the case reported.
A 56-year-old woman with a rectosigmoid neoplasm and peritoneal and liver metastases was being treated with chemotherapy (CTX) with folfox and bevacizumab. Due to a bowel obstruction, she underwent surgery in which a loop colostomy with a supporting rod was performed in the left hypochondrium, with no tumour resection.
Eight days after the operation, after the stoma rod was removed, painful ulcerative lesions were detected in the decubitus area. Postoperative CTX was started, the ulcers progressed and biopsy and culture found neutrophilic inflammatory infiltrate and Escherichia coli. The patient was diagnosed with PPG 45 days after the operation.
The PPG was treated with clobetasol propionate (0.5mg/g) every 24h for 30 days, then tacrolimus 0.1% every 24h for 45 days, and finally triamcinolone acetonide 40mg/mL by intralesional infiltration every 15 days plus oral prednisone 30mg every 24h for 60 days.
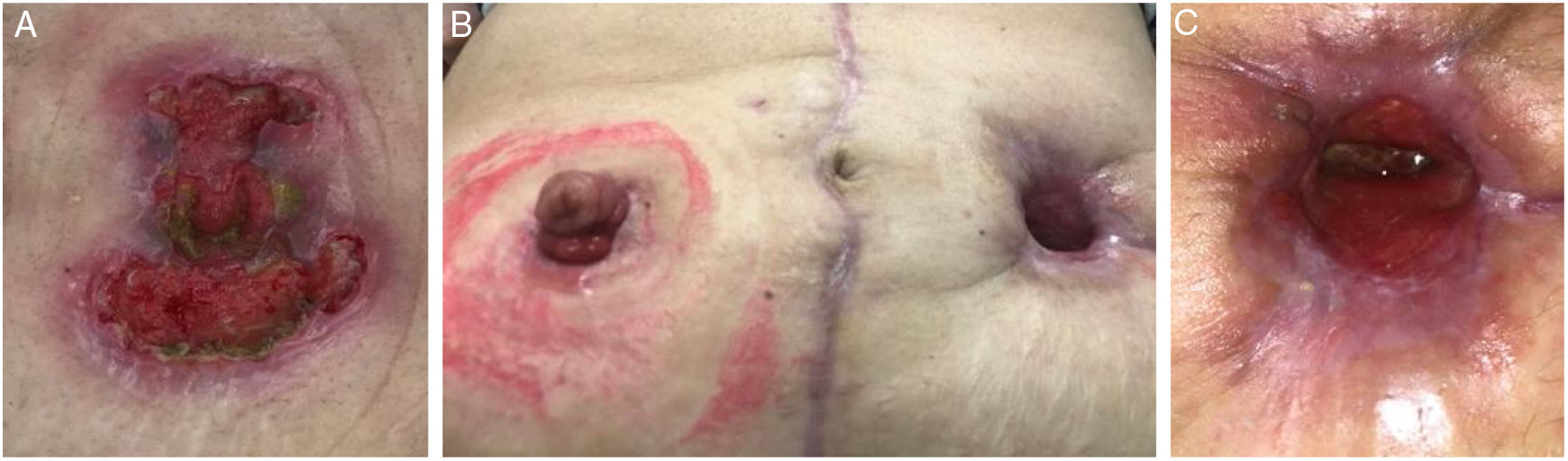
After six months of postoperative CTX, 50% regression of the primary tumour and complete response of the liver metastases were detected. Due PPG progression (Fig. 1A) and the patient's poor quality of life due to pain and difficulty in peristomal care, she underwent surgery to relocate the stoma. Local conditions allowed removal of the greater omentum with a residual implant and removal of the primary tumour (anterior resection with rectal anastomosis and protective ileostomy in the patient's right iliac fossa).
(A) Peristomal ulcers with anfractuous, raised and violaceous edges.
(B) Excision of the left colostomy and relocation of a right ileostomy 6 months after the first operation following neoadjuvant CTX and systemic treatment with corticosteroids. PPG did not develop in the new ileostomy, and the patient's pyoderma healed after tumour excision and CTX discontinuation.
(C) Detail of healing by secondary intention of the wound in the PPG area, which finally healed 3 months after the second operation.
The PPG healed by secondary intention after two months with neither CTX nor corticosteroid therapy and without PPG developing in the new ileostomy (Fig. 1B and C).
Five months after the second surgical procedure, a single focus of right peritoneal and retroperitoneal para-aortic uptake was detected on positron emission tomography/computed tomography (PET/CT), whereupon chemotherapy (FOLFIRI plus bevacizumab) was started again. At present (eight months after surgery), the patient shows no macroscopic disease on PET/CT.
Time to onset of PPG after a stoma operation varies (from 1 month to 26 years)2,3 and involves development of painful ulcers with raised, violaceous edges. The patient's ulcer appeared in the area of the supporting rod for the stoma; hence, it may have been associated with a pathergy phenomenon.1 Her severe pain required the addition of analgesics and local anaesthetics to her treatment.
PPG is diagnosed clinically and by ruling out diseases such as skin infection, abscess, contact dermatitis, peristomal irritation and the spread of an inflammatory bowel disease to the peristomal skin. Cultures do not detect pathogenic organisms, except the usual flora, and biopsy generally reports non-specific inflammation with neutrophilic dermal infiltration, ruling out other causes such as malignancy and vasculitis,2 as in the case reported.
Treatment requires topical, systemic or combined therapies, and the prognosis improves when the associated disease is treated.2,5
Topical corticosteroids through intralesional injections and occlusive dressings are the most common treatments, but topical tacrolimus has been found to yield a greater benefit.5 However, the patient did not respond and required systemic treatment. The most common systemic treatments are glucocorticoids and cyclosporine. They have similar effectiveness; the choice will depend on the patient's comorbidities and risk factors. Other immunosuppressants such as azathioprine, mycophenolate mofetil, dapsone, doxycycline, methotrexate, gamma globulins and thalidomide have been used with variable efficacy.5
The PPG in the case reported continued to progress despite systemic treatment with corticosteroids and CTX immunosuppressants (folfox plus bevacizumab).
Infliximab has been the most commonly used biologic therapy.5 In the case reported, as the patient's PPG was associated with a colorectal neoplasm being treated with CTX, systemic treatment with corticosteroids was resorted to and biologic therapy was not used due to the possibility of neoplastic progression.
Relocation of the stoma causes recurrence in the new location in most patients. However, in patients with associated systemic treatment, there is less recurrence. When the stoma is closed and not relocated, the PPG generally resolves.2,4
The case reported healed after surgery with no recurrence of PPG in the new ileostomy, possibly due to the association of preoperative systemic treatment and definitive surgery with removal of the primary tumour and the metastases.
PPG associated with colorectal carcinoma and chemotherapy is a rare complication with no clearly defined treatment regimen. Treatment includes local and systemic regimens. However, when there is no response, excision of the associated colorectal carcinoma can contribute to PPG resolution. Prospective, randomised studies are needed to compare local, systemic and surgical treatments.
Please cite this article as: Villalba Ferrer F, Julve Herraiz L, Valderas Cortés G, Cifre Martínez C, Cerveró GE, Villalba Segarra A, et al. Carcinoma colorrectal, quimioterapia y pioderma gangrenoso periestomal. Una asociación infrecuente. Gastroenterol Hepatol. 2020;43:518–519.