Obesity is a pandemic affecting the western world, with very high associated morbidity and mortality rates. The intragastric balloon is a device used in the temporary treatment of morbid obesity as a bridge to its definitive treatment. It is placed by endoscopy and remains free inside the stomach.1 Together with changes in dietary habits, this treatment achieves good results for weight loss. However, this therapy is not risk-free and can have complications, some of which are potentially serious. Consequently, even though the rate of complications is low, patients, particularly those at high risk, should be closely monitored so that severe complications can be detected early.1,2 We describe the case of a patient with previous gastric surgery who presented with a gastric perforation following the placement of an intragastric balloon.
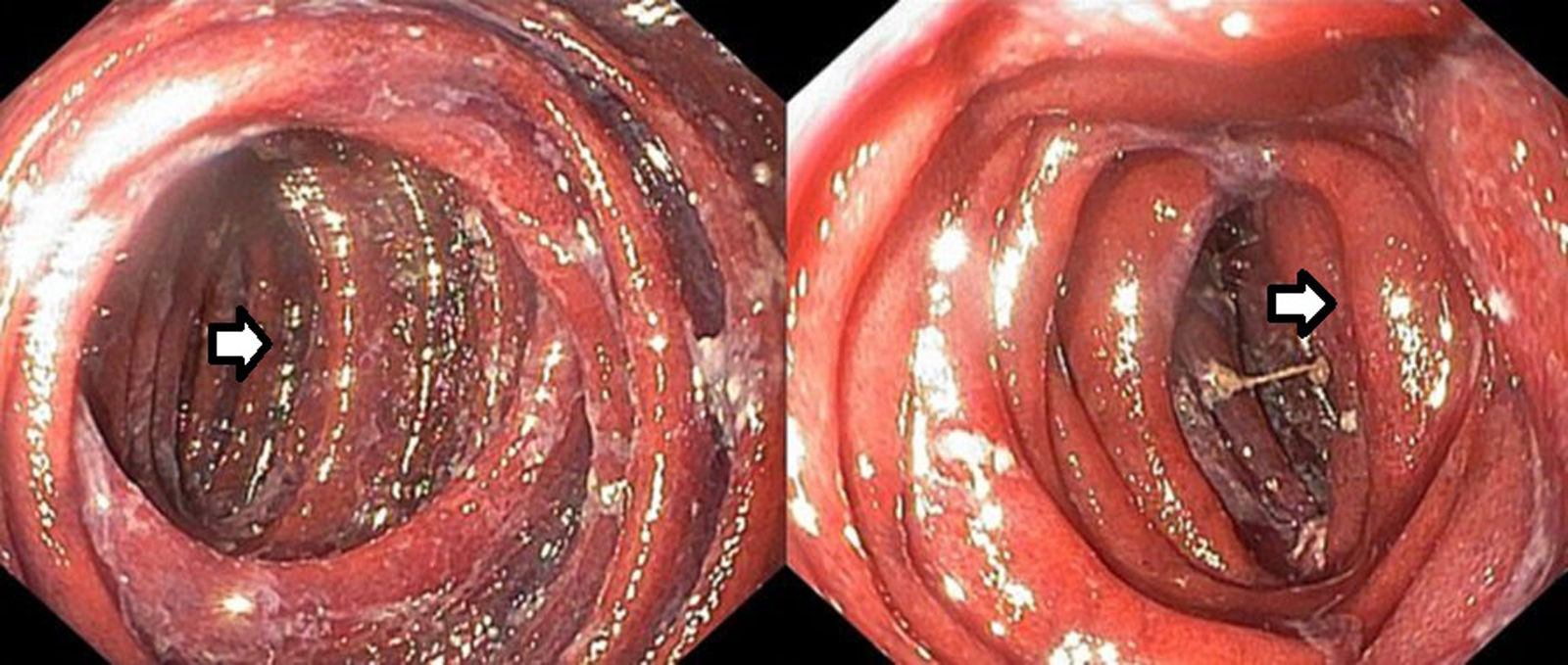
A 67-year-old morbidly obese man (body mass index 45) underwent surgery for a hiatal hernia (Nissen fundoplication) 15 years ago. Fifteen days after the insertion of an intragastric balloon (Apollo or Medsil Orbera balloon filled with 600ml physiological saline solution and methylene blue), he came to the Emergency Department of our hospital with signs and symptoms of onset 48h previously of severe pain in the upper abdomen, oral intolerance with nausea and vomiting and a poor general state of health. The physical examination revealed hypotension (80/50mmHg), tachycardia (124bpm) and board-like abdominal rigidity. Notable in the laboratory test results were leukocytosis of 19,170 with left shift (87% neutrophils) and prothrombin activity of 76%. An X-ray of the abdomen showed significant gastric dilatation and pneumoperitoneum (Fig. 1a and b). A computed tomography (CT scan) of the abdomen confirmed the findings (Fig. 1c). An emergency midline laparotomy was performed after previously revealing extensive necrosis of the lesser curvature of the stomach and subcardial perforation. A gastrectomy involving the affected zone was performed after extraction of the gastric balloon, which was found impacted at the pylorus (Fig. 1d). The patient's postoperative progress was poor, and he presented with signs and symptoms of sepsis which required antibiotic treatment and vasoactive agents, respiratory distress and an infection of the wound. The patient gradually improved, and on day 20 post-surgery showed signs and symptoms of evisceration which required another operation. During surgery, it was discovered that the gastric remnant showed an area of subcardial ischaemia. After releasing the stomach, the poor quality of the gastric remnant was observed, and as a result a total gastrectomy and Roux-en-Y oesophagojejunostomy were performed. The patient made good progress following the second surgery, on day 15 presenting with a residual abscess which was treated by image-guided drainage. He was discharged 50 days after admission. Currently, at 3 years post-surgery, he has a good quality of life and is followed up by the Nutrition Unit for monitoring of his nutritional status post-gastrectomy.
(a and b) Plain X-ray of the abdomen, anteroposterior view (a) and in decubitus with horizontal beam (b): the massive gastric dilatation is observed (arrow); (c) computed tomography (CT scan): note balloon in antral region (arrow) and massive gastric dilatation with perforation in the posterior wall (double arrow); (d) extraction of the intragastric balloon.
Endoscopic therapy can be an effective alternative to pharmacological treatment for class I and II obesity, since it is effective in the short term, reducing body weight and improving the comorbidities associated with obesity.2–4 It is based on the gastric space-occupying effects which increase feelings of fullness. The process is well-tolerated, and most of the complications are mild and well tolerated, particularly nausea and vomiting which occur in 20–25% of cases, and abdominal pain, which occurs in 15–20%.5 However, cases of mortality (0.05%) and severe complications, such as gastric perforations (0.1%), have been described.3
At present, previous gastric surgery is considered a contraindication for intragastric balloon placement, although absolute contraindication is reserved strictly for partial gastrectomy cases. However, in patients with previous abdominal surgery, monitoring must be strict to avoid severe complications. Therefore, as is seen in our case, gastric surgery, and particularly anti-reflux surgery, are significant risk factors since they make evaluating the stomach difficult, because of the same anti-reflux mechanism, in case of impaction of the balloon at the pylorus. In these cases, if the obstruction is not diagnosed early, and in view of the fact that vomiting is not possible, progressive gastric dilatation occurs, which can result in gastric necrosis and perforation. In our case, the patient was not warned of the risk and did not consult a doctor in spite of the discomfort, finally coming to the Emergency Department in a state of septic shock. It should be noted that abdominal pain, nausea and vomiting are common adverse effects in the first few days following balloon placement but are uncommon after 15 days.
In cases of gastric perforation, the treatment should be as conservative as possible given that this is a benign disease. Currently, in cases diagnosed early, laparoscopy can be performed and the orifice closed, obtaining good results.1 However, dramatic cases such as the one presented here, which involve subcardial gastric necrosis, can even require a total gastrectomy. Endoscopic treatment would have had to be ruled out for the patient described in this article because of his surgical history and body mass index, which, at 45kg/m2 (morbid obesity) means that immediate surgery would be advised.
In conclusion, we can confirm that intragastric balloon placement is not free from complications, and accordingly, it is essential that patients be monitored closely and that they are warned of the risks and the importance of attending for follow-up examinations in case of the onset of clinical signs and symptoms suggestive of complications. This is particularly the case in patients who have previously undergone anti-reflux surgery.
Please cite this article as: Ríos A, Febrero B, Rodríguez JM. Perforación gástrica por balón intragástrico en paciente con funduplicatura de Nissen. Gastroenterol Hepatol. 2018;41:251–253.