Gastric polyps are usually asymptomatic lesions incidentally discovered during endoscopy.
ObjectiveTo study the frequency of different types of gastric polyps in our population and their possible association with other factors.
Patients and methodsRetrospective study of gastroscopies performed in a tertiary hospital over a ten-year period. Demographics, medical history, indication for gastroscopy and morphological and histological characteristics of polyps were collected.
ResultsGastric polyps were found in 827 out of 41253 (2%) reviewed gastroscopies, corresponding to 709 patients. Mean age was 65.6 years, and 62% were female. 53.9% of patients had multiple polyps. The most common location was the fundus and 83.3% were smaller than 1cm. Histopathology was obtained in 607 patients: hyperplastic polyps were the most common (42.8%), followed by fundic gland polyps (37.7%). Factors independently associated with hyperplastic polyps were age and single polyp, size ≥6mm and location other than fundus. In contrast, fundic gland polyps were associated with reflux and multiple polyps, size <6mm and located in fundus. Adenomas were independently associated with single polyp.
ConclusionsFundic gland and hyperplastic polyps are the most common in our population and have characteristic features that can guide histological diagnosis. With single polyps it is advisable to take biopsies to rule out adenoma.
Los pólipos gástricos son lesiones habitualmente asintomáticas y constituyen un hallazgo durante la realización de una endoscopia.
ObjetivoEstudiar la frecuencia de los diferentes tipos de pólipos gástricos en nuestro medio y su posible asociación con otros factores.
Pacientes y métodosEstudio retrospectivo de las gastroscopias realizadas durante 10 años en un hospital de tercer nivel. Se recogieron datos demográficos, antecedentes patológicos, indicación de la gastroscopia y características morfológicas e histológicas de los pólipos.
ResultadosSe incluyeron 41.253 gastroscopias, identificándose 827 (2%) con pólipos gástricos correspondientes a 709 pacientes. La edad media fue 65,6 años y un 62% fueron mujeres. El 53,9% tenían múltiples pólipos. La localización más frecuente fue fundus y la mayoría fueron menores de 1cm (83,3%). Se obtuvo muestra para anatomía patológica en 607 pacientes, siendo los más frecuentes los pólipos hiperplásicos (42,8%), seguidos de los pólipos de glándula fúndica (37,7%).
Los factores que se asociaron de forma independiente a los pólipos hiperplásicos fueron la edad y el ser pólipo único, de tamaño ≥6mm y localización no fúndica. Contrariamente, los de glándula fúndica se asociaron a la indicación por reflujo y el ser múltiples, <6mm y localizados en fundus. Los pólipos adenomatosos se asociaron a ser un pólipo único.
ConclusionesLos pólipos de glándula fúndica e hiperplásicos son los más frecuentes en nuestro medio, y tienen rasgos contrarios que pueden orientar al diagnóstico histológico. En el caso de pólipos únicos es recomendable la toma de biopsias para descartar el diagnóstico de adenoma.
Gastric polyps are usually asymptomatic lesions that tend to be diagnosed during an upper gastrointestinal tract endoscopy. Their prevalence is variable, from 0.3 to 6% in different studies,1,2 and they have been associated with various factors, such as H. pylori infection, proton-pump inhibitor (PPI) use and chronic atrophic gastritis.3,4
The classification of gastric polyps is based on their histological characteristics. The most prevalent are epithelial polyps, and the most common among them are hyperplastic and fundic gland polyps, with adenomatous polyps being much less common, representing only 1–12%.1,2,5,6 However, this distribution varies widely based on the population studied.
Gastric polyps, like those in other locations, can become malignant. The risk of malignant transformation depends on the histological type: hyperplastic polyps have a low risk of malignant transformation (2%),7 while adenomas have a higher risk (up to 30%).8–10 The importance of the histological exam stems from the fact that the macroscopic appearance and pathological anatomy study results do not always match.11,12 Biopsies may also not be representative of the entire polyp.13,14 Therefore, the existence of factors associated with the different histological types of gastric polyps can be useful when making clinical decisions.
The objective of our work was to study the frequency of the different types of gastric polyps in our area and to identify the factors associated with the most common histological types.
Patients and methodsA retrospective study in which all gastroscopies (scheduled and emergency) performed at a tertiary-level hospital (Hospital Clínic de Barcelona [Hospital Clínic of Barcelona]) from January 2002 to September 2012 were reviewed. Gastroscopies were identified manually based on the reports stored in the endoscopy unit file. Follow-up gastroscopies performed on the same patient were not excluded. Endoscopic reports were prepared with the Endobase system (Olympus, Germany).
All data regarding patients and the characteristics of the polyps were obtained from the electronic medical record and the endoscopy reports, respectively. Demographic data were collected (sex, age), relevant pathological history (cirrhosis, colon polyps, colorectal cancer or hereditary polyposis syndrome) as well as data related to the endoscopy (indication included in the report, number and size of the polyps, location and histological type, and the presence of chronic gastritis or H. pylori infection using the urease test). Taking of proton-pump inhibitors (PPIs) could not be collected. In patients with gastric polyps who had an endoscopic follow-up, only the data from the initial endoscopy were considered.
The size of the polyp was calculated by comparing it with the size of the open biopsy forceps or by measuring the polyp after removal and recovery for an anatomical pathology study. In the case of multiple polyps, the largest was considered.
Statistical analysisIn the descriptive analysis, the continuous variables that followed a normal distribution were presented in the form of the mean±standard deviation and range, while those that did not follow a normal distribution were presented in the form of the median and the interquartile range. For comparisons, Student's t-test was used for quantitative variables that followed a normal distribution, the Mann–Whitney U test for those that did not follow a normal distribution and chi-squared for qualitative variables. A univariate analysis was conducted to identify the possible factors associated with the different types of polyps. Then a multivariate analysis was carried out with variables that achieved statistical significance and those deemed clinically relevant. The level of statistical significance was established with a p of less than 0.05. All calculations were done using the SPSS programme for Windows, version 19.0.
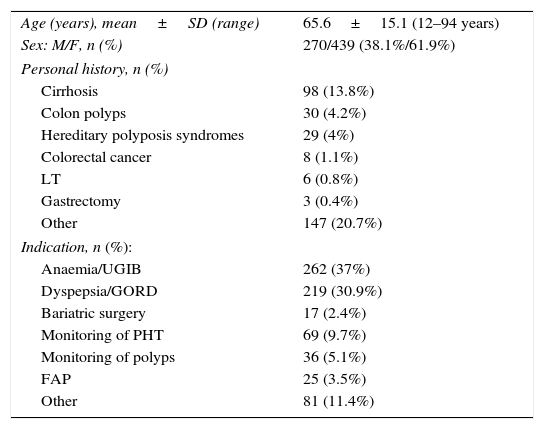
ResultsBetween January 2002 and September 2012, 41,253 gastroscopies were performed, detecting 827 (2%) with gastric polyps corresponding to 709 patients. Table 1 shows the characteristics of patients with gastric polyps. The mean age was 65 years and the majority were female (62%). Some 24% of patients had relevant pathological gastrointestinal history, including colon polyps (4.2%) and hereditary syndromes (4%). The most common indications for the UGIE were dyspepsia or gastro-oesophageal reflux disease (GORD) (30.9%) and anaemia or upper gastrointestinal bleeding (UGIB) (37%). 20.7% of patients were asymptomatic. Regarding the characteristics of the polyps, more than half of the patients had multiple polyps and the most common location was in the fundus (36.7%), either alone or associated with other locations. Regarding the size of the polyps, the majority were less than 10mm (83.3%), with a median of 5mm (interquartile range 3–8mm) (Table 2).
Characteristics of the 709 patients with gastric polyps.
| Age (years), mean±SD (range) | 65.6±15.1 (12–94 years) |
| Sex: M/F, n (%) | 270/439 (38.1%/61.9%) |
| Personal history, n (%) | |
| Cirrhosis | 98 (13.8%) |
| Colon polyps | 30 (4.2%) |
| Hereditary polyposis syndromes | 29 (4%) |
| Colorectal cancer | 8 (1.1%) |
| LT | 6 (0.8%) |
| Gastrectomy | 3 (0.4%) |
| Other | 147 (20.7%) |
| Indication, n (%): | |
| Anaemia/UGIB | 262 (37%) |
| Dyspepsia/GORD | 219 (30.9%) |
| Bariatric surgery | 17 (2.4%) |
| Monitoring of PHT | 69 (9.7%) |
| Monitoring of polyps | 36 (5.1%) |
| FAP | 25 (3.5%) |
| Other | 81 (11.4%) |
FAP: familial adenomatous polyposis; GORD: gastro-oesophageal reflux disease; LT: liver transplant; PHT: portal hypertension; UGIB: upper gastrointestinal bleeding.
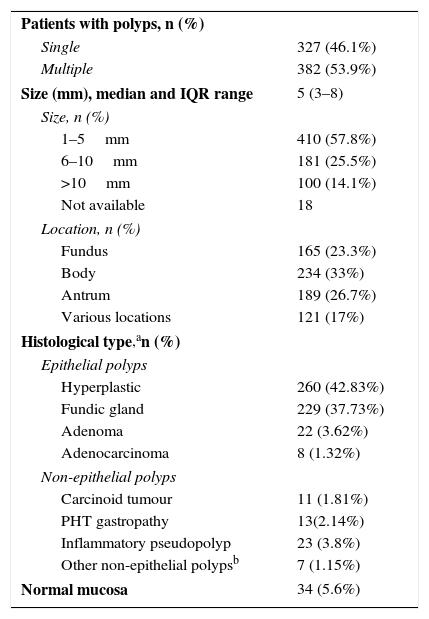
Morphological and histological characteristics of the polyps.
| Patients with polyps, n (%) | |
| Single | 327 (46.1%) |
| Multiple | 382 (53.9%) |
| Size (mm), median and IQR range | 5 (3–8) |
| Size, n (%) | |
| 1–5mm | 410 (57.8%) |
| 6–10mm | 181 (25.5%) |
| >10mm | 100 (14.1%) |
| Not available | 18 |
| Location, n (%) | |
| Fundus | 165 (23.3%) |
| Body | 234 (33%) |
| Antrum | 189 (26.7%) |
| Various locations | 121 (17%) |
| Histological type,an (%) | |
| Epithelial polyps | |
| Hyperplastic | 260 (42.83%) |
| Fundic gland | 229 (37.73%) |
| Adenoma | 22 (3.62%) |
| Adenocarcinoma | 8 (1.32%) |
| Non-epithelial polyps | |
| Carcinoid tumour | 11 (1.81%) |
| PHT gastropathy | 13(2.14%) |
| Inflammatory pseudopolyp | 23 (3.8%) |
| Other non-epithelial polypsb | 7 (1.15%) |
| Normal mucosa | 34 (5.6%) |
PHT: portal hypertension.
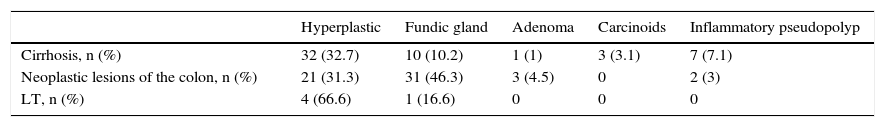
Samples were obtained for pathological anatomy in 607 patients (85.6%). The histological study showed epithelial polyps in 512 patients (84.3%), with hyperplastic polyps being the most common (n=260; 42.8%), followed by fundic gland polyps (n=229; 37.7%) (Table 2). In 8 cases the diagnosis was adenocarcinoma, 7 (24%) in adenomatous polyps and one in a hyperplastic polyp (0.4%). Table 3 describes the frequency of the different types of polyps in patients with a history of gastrointestinal diseases. In 34 patients (5.6%) with endoscopically-identified polyps, the biopsies described normal mucosa. All lesions with normal mucosa were small (less than 1cm) and most were smaller than 5mm (71%).
Types of gastric polyps in patients with a more relevant history of gastrointestinal disease.
| Hyperplastic | Fundic gland | Adenoma | Carcinoids | Inflammatory pseudopolyp | |
|---|---|---|---|---|---|
| Cirrhosis, n (%) | 32 (32.7) | 10 (10.2) | 1 (1) | 3 (3.1) | 7 (7.1) |
| Neoplastic lesions of the colon, n (%) | 21 (31.3) | 31 (46.3) | 3 (4.5) | 0 | 2 (3) |
| LT, n (%) | 4 (66.6) | 1 (16.6) | 0 | 0 | 0 |
LT: liver transplant.
An H. pylori study was carried out with the urease test in 144 patients (20.3%). It was positive in 40 (27.8%). H. pylori was positive in 18 of the 54 (33.3%) hyperplastic polyps and in 8 of the 44 (18.2%) fundic gland polyps. Samples were also taken of the body and antral mucosa to test for chronic gastritis in 137 patients (19.4%), showing chronic gastritis in 94 (68.6%), of which 36 had hyperplastic polyps and 29 had fundic gland polyps.
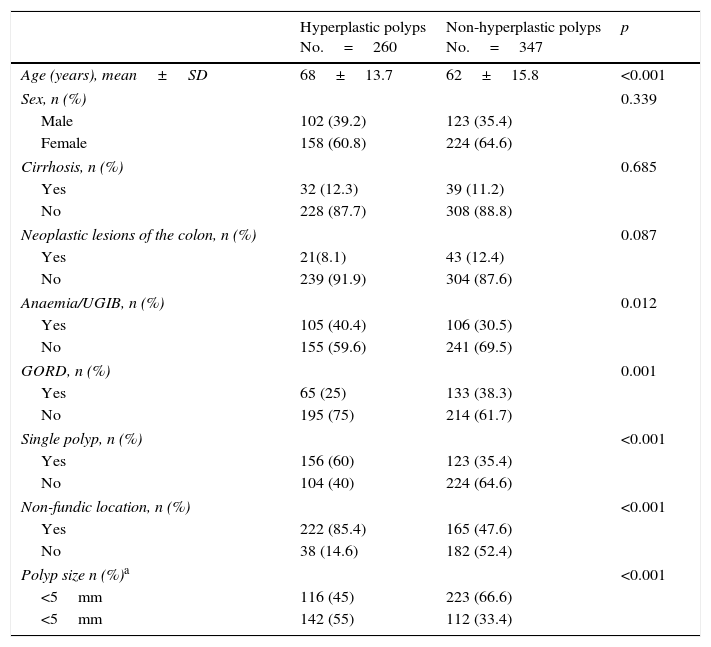
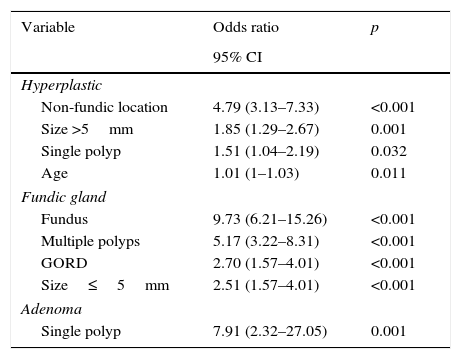
The factors independently associated with hyperplastic polyps were age and being a single polyp, sized ≥6mm and having a non-fundic location. For fundic gland polyps, the associated variables were indication of GORD and various characteristics of the polyp itself, the opposite of those associated with hyperplastic polyps (being multiple polyps, <6mm and located in the fundus). Adenomatous polyps were independently associated with being a single polyp (Tables 4–7).
Univariate analysis of the possible factors associated with hyperplastic polyps (n=607 polyps with confirmed histology).
| Hyperplastic polyps No.=260 | Non-hyperplastic polyps No.=347 | p | |
|---|---|---|---|
| Age (years), mean±SD | 68±13.7 | 62±15.8 | <0.001 |
| Sex, n (%) | 0.339 | ||
| Male | 102 (39.2) | 123 (35.4) | |
| Female | 158 (60.8) | 224 (64.6) | |
| Cirrhosis, n (%) | 0.685 | ||
| Yes | 32 (12.3) | 39 (11.2) | |
| No | 228 (87.7) | 308 (88.8) | |
| Neoplastic lesions of the colon, n (%) | 0.087 | ||
| Yes | 21(8.1) | 43 (12.4) | |
| No | 239 (91.9) | 304 (87.6) | |
| Anaemia/UGIB, n (%) | 0.012 | ||
| Yes | 105 (40.4) | 106 (30.5) | |
| No | 155 (59.6) | 241 (69.5) | |
| GORD, n (%) | 0.001 | ||
| Yes | 65 (25) | 133 (38.3) | |
| No | 195 (75) | 214 (61.7) | |
| Single polyp, n (%) | <0.001 | ||
| Yes | 156 (60) | 123 (35.4) | |
| No | 104 (40) | 224 (64.6) | |
| Non-fundic location, n (%) | <0.001 | ||
| Yes | 222 (85.4) | 165 (47.6) | |
| No | 38 (14.6) | 182 (52.4) | |
| Polyp size n (%)a | <0.001 | ||
| <5mm | 116 (45) | 223 (66.6) | |
| <5mm | 142 (55) | 112 (33.4) | |
GORD: gastro-oesophageal reflux disease; UGIB: upper gastrointestinal bleeding.
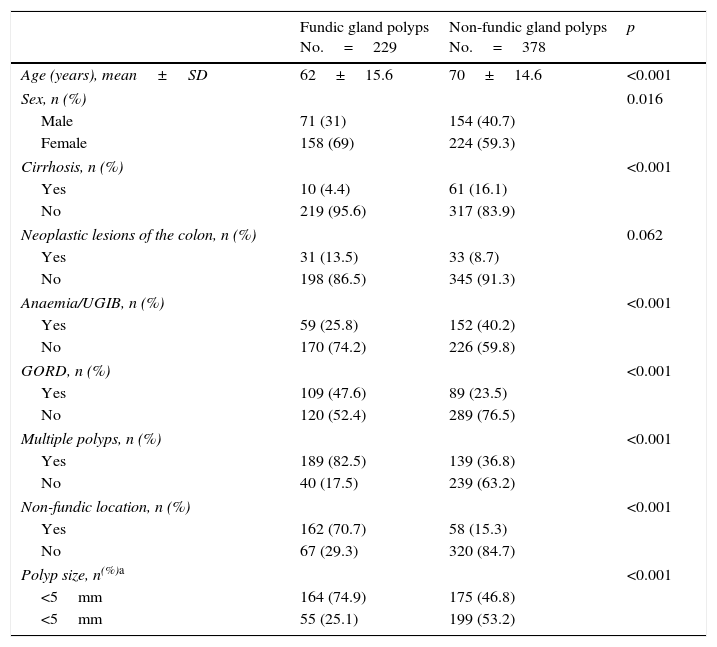
Univariate analysis of the possible factors associated with fundic gland polyps (n=607 polyps with confirmed histology).
| Fundic gland polyps No.=229 | Non-fundic gland polyps No.=378 | p | |
|---|---|---|---|
| Age (years), mean±SD | 62±15.6 | 70±14.6 | <0.001 |
| Sex, n (%) | 0.016 | ||
| Male | 71 (31) | 154 (40.7) | |
| Female | 158 (69) | 224 (59.3) | |
| Cirrhosis, n (%) | <0.001 | ||
| Yes | 10 (4.4) | 61 (16.1) | |
| No | 219 (95.6) | 317 (83.9) | |
| Neoplastic lesions of the colon, n (%) | 0.062 | ||
| Yes | 31 (13.5) | 33 (8.7) | |
| No | 198 (86.5) | 345 (91.3) | |
| Anaemia/UGIB, n (%) | <0.001 | ||
| Yes | 59 (25.8) | 152 (40.2) | |
| No | 170 (74.2) | 226 (59.8) | |
| GORD, n (%) | <0.001 | ||
| Yes | 109 (47.6) | 89 (23.5) | |
| No | 120 (52.4) | 289 (76.5) | |
| Multiple polyps, n (%) | <0.001 | ||
| Yes | 189 (82.5) | 139 (36.8) | |
| No | 40 (17.5) | 239 (63.2) | |
| Non-fundic location, n (%) | <0.001 | ||
| Yes | 162 (70.7) | 58 (15.3) | |
| No | 67 (29.3) | 320 (84.7) | |
| Polyp size, n(%)a | <0.001 | ||
| <5mm | 164 (74.9) | 175 (46.8) | |
| <5mm | 55 (25.1) | 199 (53.2) | |
GORD: gastro-oesophageal reflux disease; UGIB: upper gastrointestinal bleeding.
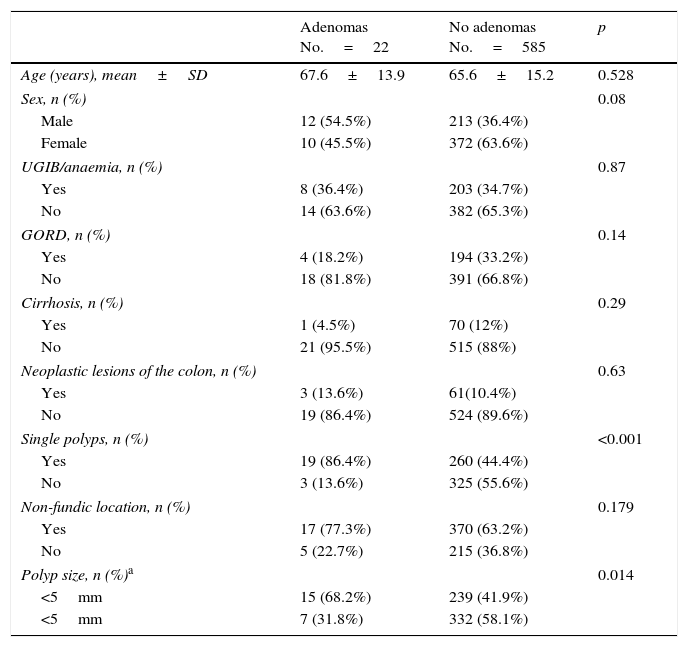
Univariate analysis of the possible factors associated with gastric adenomas (n=607 polyps with confirmed histology).
| Adenomas No.=22 | No adenomas No.=585 | p | |
|---|---|---|---|
| Age (years), mean±SD | 67.6±13.9 | 65.6±15.2 | 0.528 |
| Sex, n (%) | 0.08 | ||
| Male | 12 (54.5%) | 213 (36.4%) | |
| Female | 10 (45.5%) | 372 (63.6%) | |
| UGIB/anaemia, n (%) | 0.87 | ||
| Yes | 8 (36.4%) | 203 (34.7%) | |
| No | 14 (63.6%) | 382 (65.3%) | |
| GORD, n (%) | 0.14 | ||
| Yes | 4 (18.2%) | 194 (33.2%) | |
| No | 18 (81.8%) | 391 (66.8%) | |
| Cirrhosis, n (%) | 0.29 | ||
| Yes | 1 (4.5%) | 70 (12%) | |
| No | 21 (95.5%) | 515 (88%) | |
| Neoplastic lesions of the colon, n (%) | 0.63 | ||
| Yes | 3 (13.6%) | 61(10.4%) | |
| No | 19 (86.4%) | 524 (89.6%) | |
| Single polyps, n (%) | <0.001 | ||
| Yes | 19 (86.4%) | 260 (44.4%) | |
| No | 3 (13.6%) | 325 (55.6%) | |
| Non-fundic location, n (%) | 0.179 | ||
| Yes | 17 (77.3%) | 370 (63.2%) | |
| No | 5 (22.7%) | 215 (36.8%) | |
| Polyp size, n (%)a | 0.014 | ||
| <5mm | 15 (68.2%) | 239 (41.9%) | |
| <5mm | 7 (31.8%) | 332 (58.1%) | |
GORD: gastro-oesophageal reflux disease; UGIB: upper gastrointestinal bleeding.
Risk value for the significant variables in the multivariate analysis.
| Variable | Odds ratio | p |
|---|---|---|
| 95% CI | ||
| Hyperplastic | ||
| Non-fundic location | 4.79 (3.13–7.33) | <0.001 |
| Size >5mm | 1.85 (1.29–2.67) | 0.001 |
| Single polyp | 1.51 (1.04–2.19) | 0.032 |
| Age | 1.01 (1–1.03) | 0.011 |
| Fundic gland | ||
| Fundus | 9.73 (6.21–15.26) | <0.001 |
| Multiple polyps | 5.17 (3.22–8.31) | <0.001 |
| GORD | 2.70 (1.57–4.01) | <0.001 |
| Size≤5mm | 2.51 (1.57–4.01) | <0.001 |
| Adenoma | ||
| Single polyp | 7.91 (2.32–27.05) | 0.001 |
GORD: gastro-oesophageal reflux disease.
This is the first study that evaluates the frequency and histological type of gastric polyps in a provincial hospital in Barcelona, and it includes the greatest number of gastroscopies of all those conducted in Spain. In the literature, a great variability was observed in the prevalence of gastric polyps, with a polyp detection rate ranging from 0.6% to 6.35% in Brazil and the United States, respectively.1,2 Our detection rate (2%) would be located between what was reported in two other studies conducted in Spain: 0.3% in a hospital in Orense6 and 4.2% in a hospital in Madrid.5
Epithelial polyps are the most common in all published studies, meaning that hyperplastic and fundic gland polyps together make up 60–90%1,2,5 followed by adenomas, which are much less common (0.7–12%),1,2 with these rates being similar to those observed in our population (80% and 3.6%, respectively). However, there is more variability in the proportion of hyperplastic and fundic gland polyps. In the majority of series with adult patients, hyperplastic polyps are the most common (44–70%),1,15–17 but in Camarck's American series,2 fundic gland polyps represented 77%, with the prevalence much higher than that which is published in the literature. Although in three Spanish series (including ours) hyperplastic polyps were the most common, they did not exceed 50% of the total.5,6 It has been suggested that the differences in prevalence of these polyp subtypes could be related to factors such as H. pylori or taking PPIs.3,4,18–21 It is notable that in the other two Spanish series, the percentage of fundic gland polyps was much lower than in ours (7.4% in one and it was not mentioned in the other), despite recording chronic PPI use in 46.5% of patients.5 In our study we do not have this information, since it could not be obtained with sufficient reliability due to this being a retrospective study, but the high prevalence of fundic gland polyps in our series could result from high PPI use in our population.
In the majority of patients in our series, the polyps were detected casually during a gastroscopy performed to study gastrointestinal symptoms not attributable to polyps (for example, reflux) or asymptomatic patients examined for other reasons (for example, pre-bariatric surgery assessment), results that are similar to other publications.2,17 However, it should be kept in mind that, although the majority of gastric polyps do not cause symptoms, they can be the cause of bleeding, abdominal pain and even obstruction.22,23 In the literature, an association has been described between anaemia or UGIB and hyperplastic polyps, while the symptoms of GORD are associated with fundic gland polyps,23 although in our study only the latter was found.
The literature reports that, in between 16 and 37.5% of cases, despite the endoscopic appearance of a polyp, the histological study shows normal mucosa2,6 and this percentage increases in smaller lesions. In our study the percentage of biopsies with normal mucosa was significantly lower (5.6%), with the majority of lesions being smaller than 5mm. However, it should be pointed out that there is not always concordance between macroscopic appearance and pathological anatomy.11,12 Therefore, identification of characteristic features of each type of polyp may be helpful when making clinical decisions, but this does not avoid the recommendation to obtain biopsies. This would be especially relevant in cases of single polyps, since they are associated with the diagnosis of adenoma, and this type of polyp is the type with the highest risk of malignant transformation. In our study, 7 of the 8 adenocarcinomas diagnosed developed in an adenomatous polyp.
In patients with gastric polyps, the current guidelines recommend evaluating the state of H. pylori infection and obtaining biopsies of the surrounding gastric mucosa to rule out the coexistence of chronic gastritis.24,25 In our case, both determinations were carried out in just 20% of patients, which indicates low knowledge of and/or compliance with the recommendations. Eradication of H. pylori is the first link in treatment for hyperplastic polyps, since a disappearance of up to 80% of polyps has been shown.26–28 Also, due to the association of hyperplastic polyps with chronic gastritis, when a neoplasm appears it rarely does so on the polyp itself, rather on the atrophic mucosa. It is therefore crucial to investigate its existence to establish adequate follow-up. In general, gastric polyps of the non-adenomatous type have a low risk of malignant transformation, therefore endoscopic resection is not necessary,25 although some guidelines recommend polypectomy of hyperplastic polyps greater than 0.5cm.29,30
Despite the fact that this is one of the studies with the greatest number of patients, the biggest limitation is the retrospective design, the fact that it was conducted at a single site, and that it did not take into account whether more than one endoscopy had been performed in each patient. Therefore, our polyp detection rate is over the total number of endoscopies performed, which underestimates the real frequency of gastric polyps in our series. The participation of different endoscopists and pathologists could be considered another limitation due to the inter-observer variability, although this would not be more than a reflection of the reality of daily clinical practice and would increase the external validity of the study. For example, the decision to biopsy the polyps or not depended on the endoscopist, which would explain why they were not biopsied in some cases. Also, due to the extensive period of study, it is reasonable to expect that changes in the technique and quality of the examinations have occurred. Finally, the factors evaluated did not include taking of PPIs, and the H. pylori infection tests were not carried out in all patients included.
In conclusion, fundic gland and hyperplastic polyps are the most common gastric polyps in our area and they have opposing characteristic features that can orient the histological diagnosis. Nevertheless, in the case of single polyps, biopsies are recommended to rule out a diagnosis of adenoma. Finally, good knowledge of clinical practice guidelines is essential for the correct management of these lesions.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Argüello Viúdez L, Córdova H, Uchima H, Sánchez-Montes C, Ginès À, Araujo I, et al. Pólipos gástricos: análisis retrospectivo de 41.253 endoscopias digestivas altas. Gastroenterol Hepatol. 2017;40:507–514.