Despite novel medical therapies, colectomy has a role in the management of patients with ulcerative colitis (UC) and inflammatory bowel disease unclassified (IBDU). This study aimed to determine the incidence of unplanned surgery and initiation of immunomodulatory or biologic therapy (IMBT) after colectomy in patients with UC or IBDU, and identify associated factors.
MethodsData of patients with preoperative diagnosis of UC or IBDU who underwent colectomy and were followed up at a single tertiary centre was retrospectively collected. The primary outcome was the risk of unplanned surgery and initiation of IMBT during follow-up after colectomy. Secondary outcomes were development of Crohn's disease-like (CDL) complications and failure of reconstructive techniques.
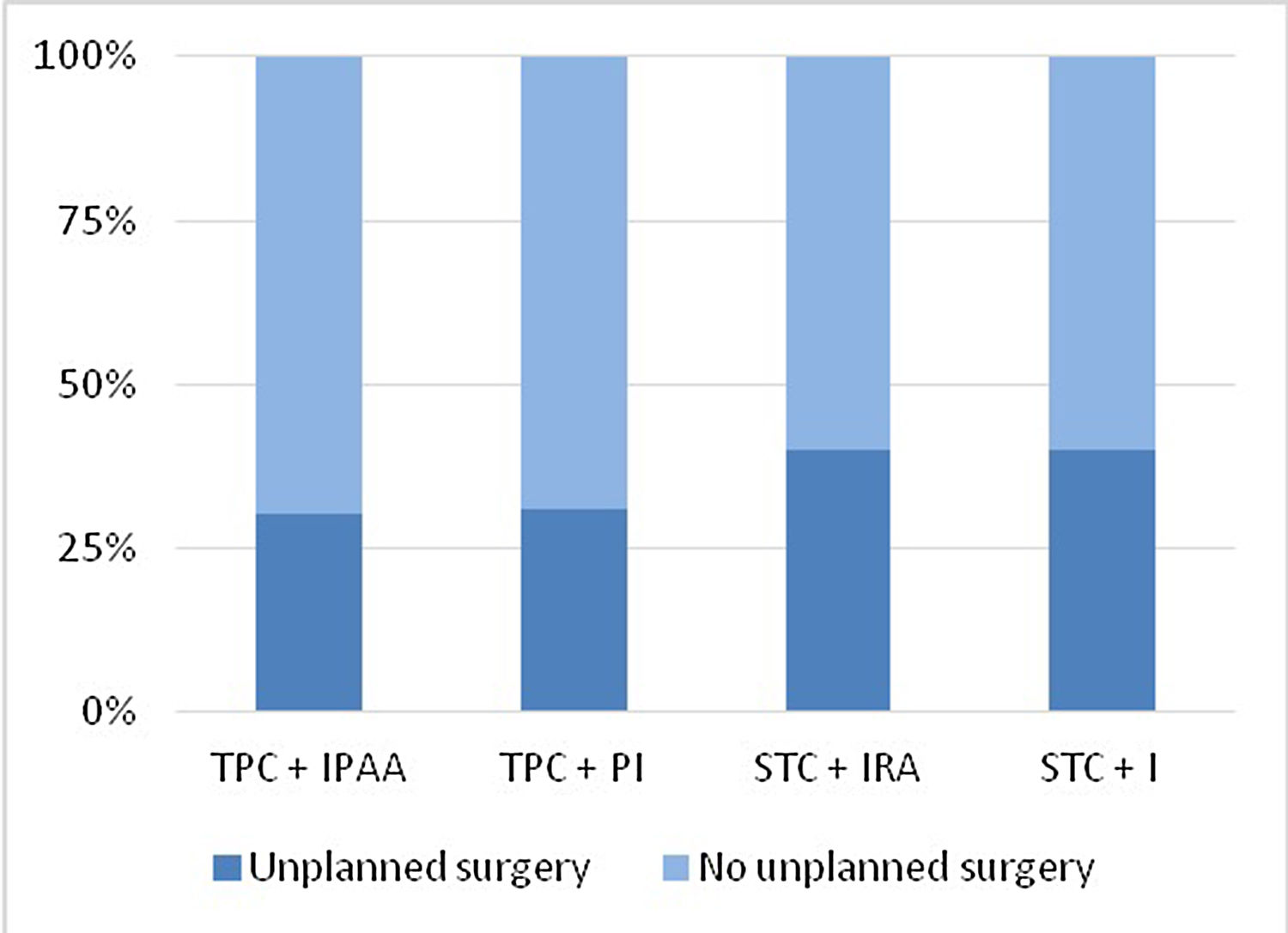
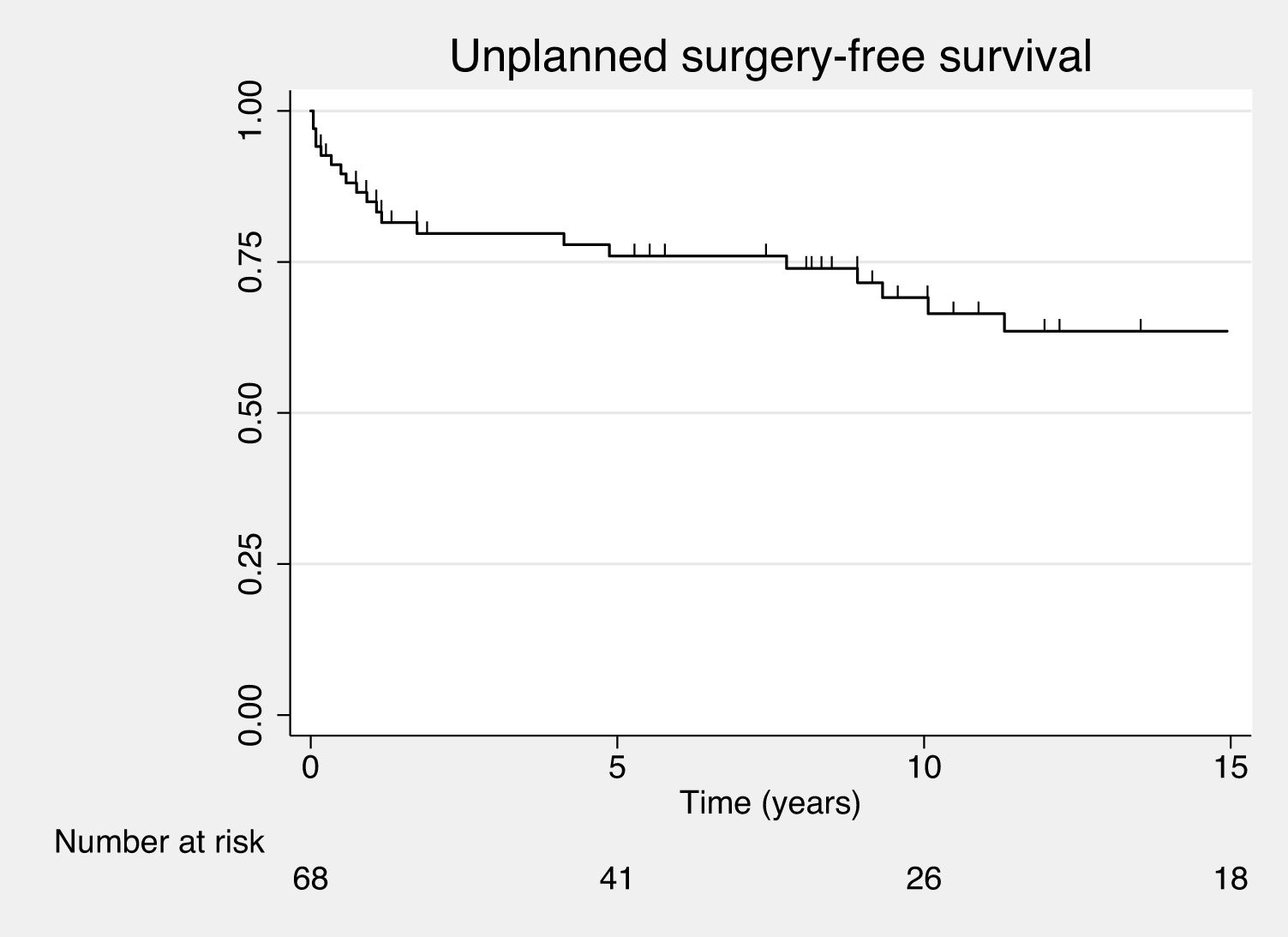
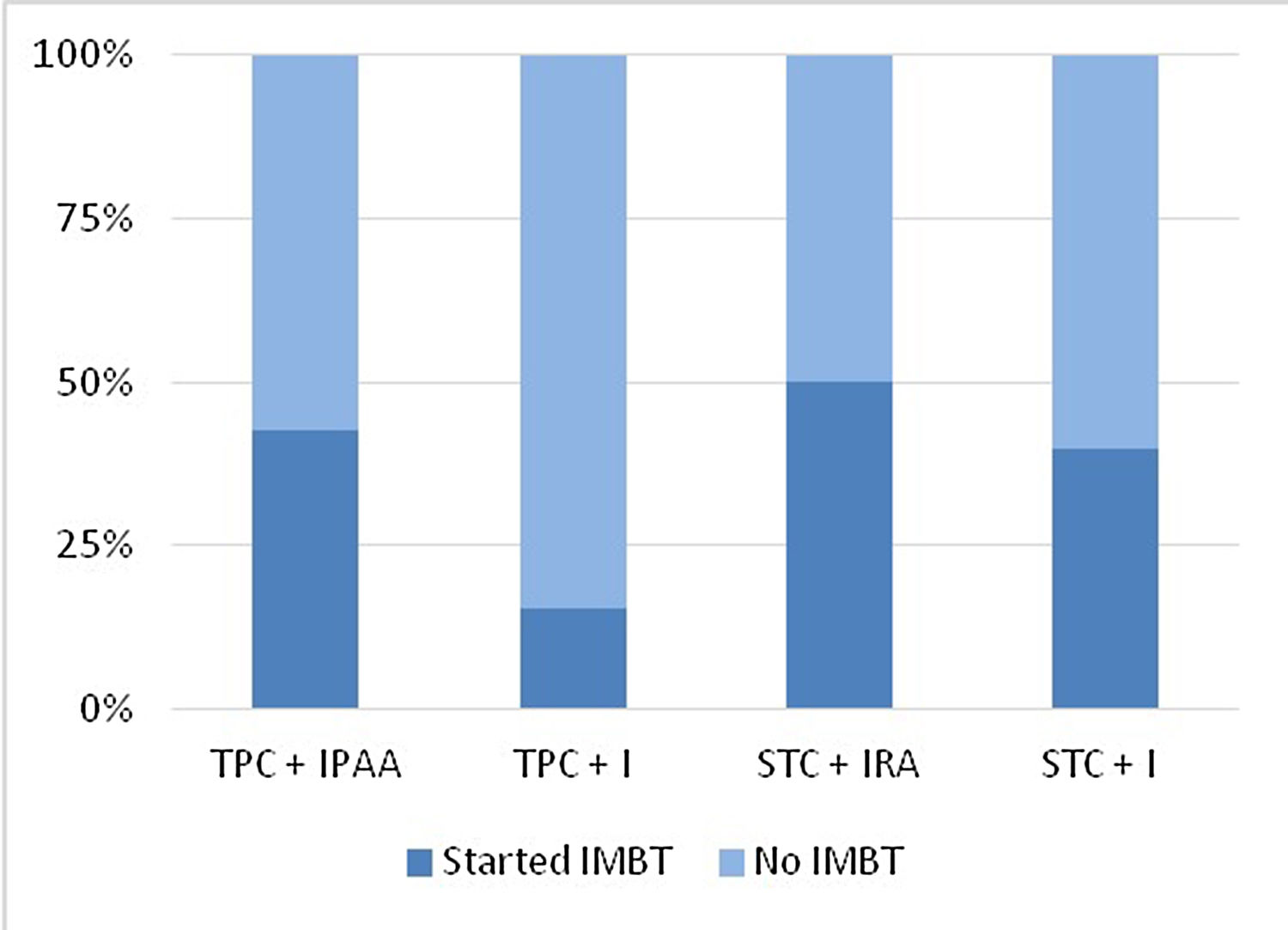
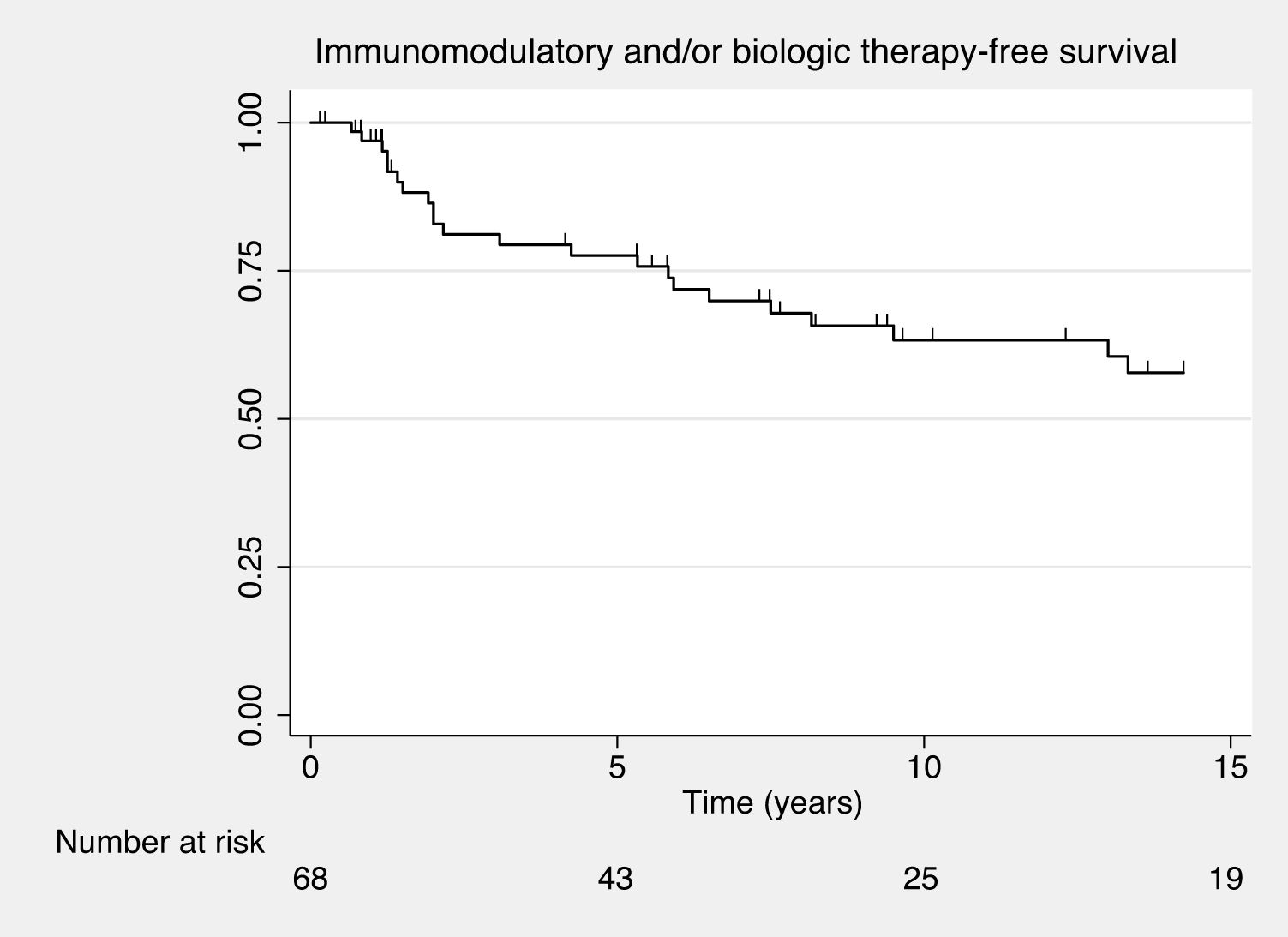
Results68 patients were included. After a median follow-up of 9.9 years, 32.4% of patients underwent unplanned surgery and IMBT was started in 38.2%. Unplanned surgery-free survival was 85% (95% confidence interval [CI] 73.8–91.6%) at 1 year, 76% (95% CI 63.2–84.9%) at 5 years and 69.1% (95% CI 55–79.6%) at 10 years. IMBT-free survival was 96.9% (95% CI 88.2–99.2%) at 1 year, 77.6% (95% CI 64.5–86.3%) at 5 years and 63.3% (95% CI 48.8–74.7%) at 10 years. 29.4% of patients met criteria for CDL complications. CDL complications were significantly associated to IMBT (hazard ratio 4.5, 95% CI 2–10.1).
ConclusionIn a retrospective study, we found a high incidence of unplanned surgery and IMBT therapy initiation after colectomy among patients with UC or IBDU. These results further question the historical concept of surgery as a “definitive” treatment.
La colectomía continúa teniendo un rol terapéutico en pacientes con colitis ulcerosa (CU) y enfermedad inflamatoria intestinal no clasificada (EII-noC). El objetivo de este estudio fue determinar la incidencia de cirugía no planificada e inicio de terapias inmunomoduladoras/biológicas (TIMB) tras colectomía en pacientes con CU o EII-noC, e identificar factores de riesgo.
MétodosSe analizaron retrospectivamente los datos de pacientes con CU o EII-noC y colectomía seguidos en un centro terciario. El objetivo primario fue evaluar el riesgo de reintervención e inicio de TIMB. Los objetivos secundarios fueron analizar la incidencia de Crohn “de novo” y el fracaso de las técnicas reconstructivas.
Resultados68 pacientes fueron incluidos. Tras una mediana de seguimiento de 9.9 años, el 32.4% de los pacientes fueron reintervenidos y el 38.2% inició TIMB. La supervivencia libre de reintervención fue 85% (intervalo confianza 95% [IC] 73.8-91.6%) al año, 76% (IC 95% 63.2-84.9%) a los 5 años y 69.1% (IC 95% 55-79.6%) a los 10 años. La supervivencia libre de TIMB fue 96.9% (IC 95% 88.2-99.2%) al año, 77.6% (IC 95% 64.5-86.3%) a los 5 años y 63.3% (IC 95% 48.8-74.7%) a los 10 años. 29.4% de los pacientes cumplieron criterios de Crohn “de novo”. Crohn “de novo” fue factor de riesgo para inicio de TIMB (Hazard ratio 4.5%, IC 95% 2-10.1).
ConclusiónEn una cohorte retrospectiva, encontramos una alta incidencia de cirugía e inicio de TIMB tras colectomía en CU o EII-noC. Estos resultados cuestionan el concepto clásico de colectomía como tratamiento definitivo.