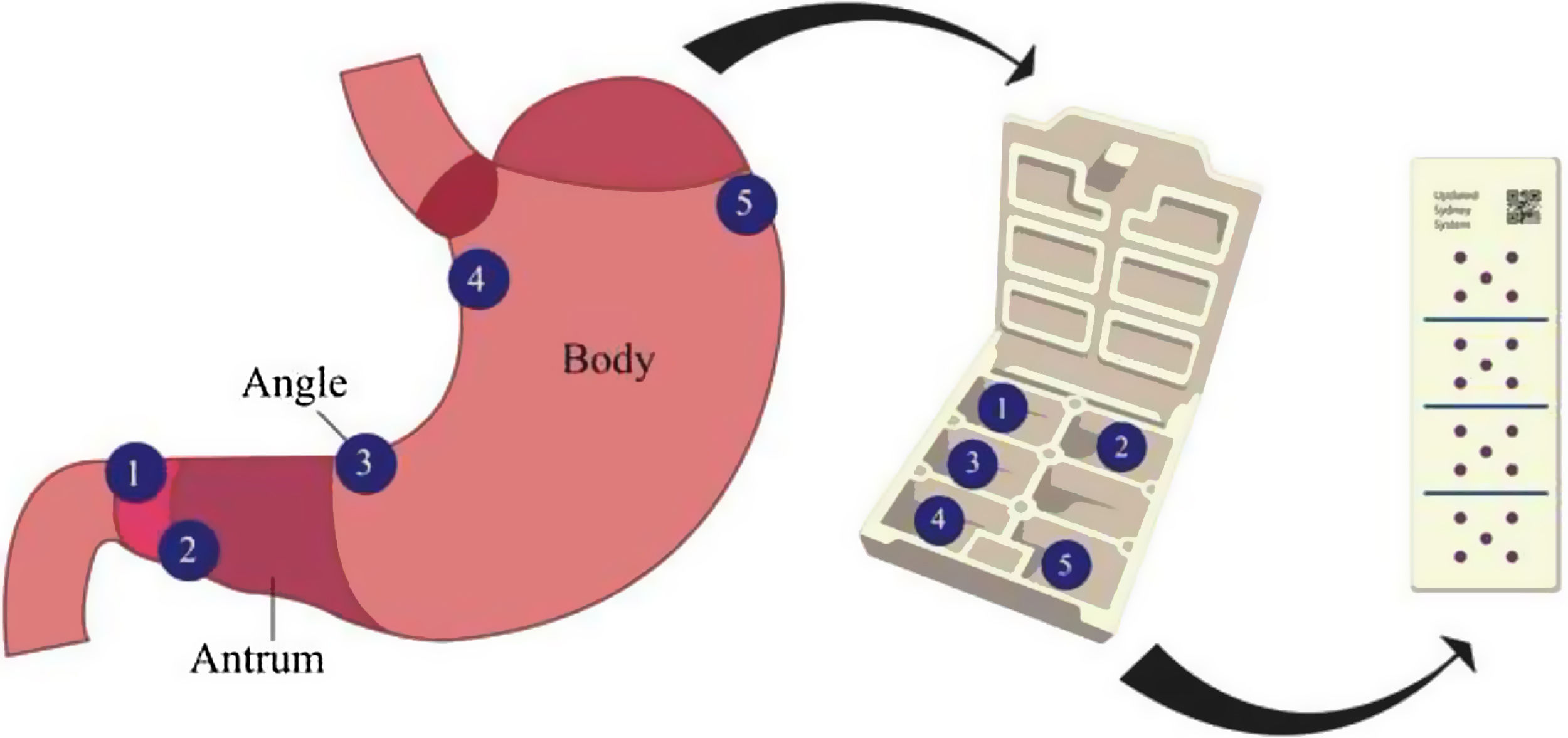
The updated Sydney system biopsy protocol (USSBP) standardizes the sampling of gastric biopsies for the detection of preneoplastic conditions (e.g., gastric intestinal metaplasia [GIM]), but the real-world diagnostic yield is not well-described.
AimTo determine whether regular application of USSBP is associated with higher detection of chronic atrophic gastritis (CAG), GIM and autoimmune gastritis (AIG).
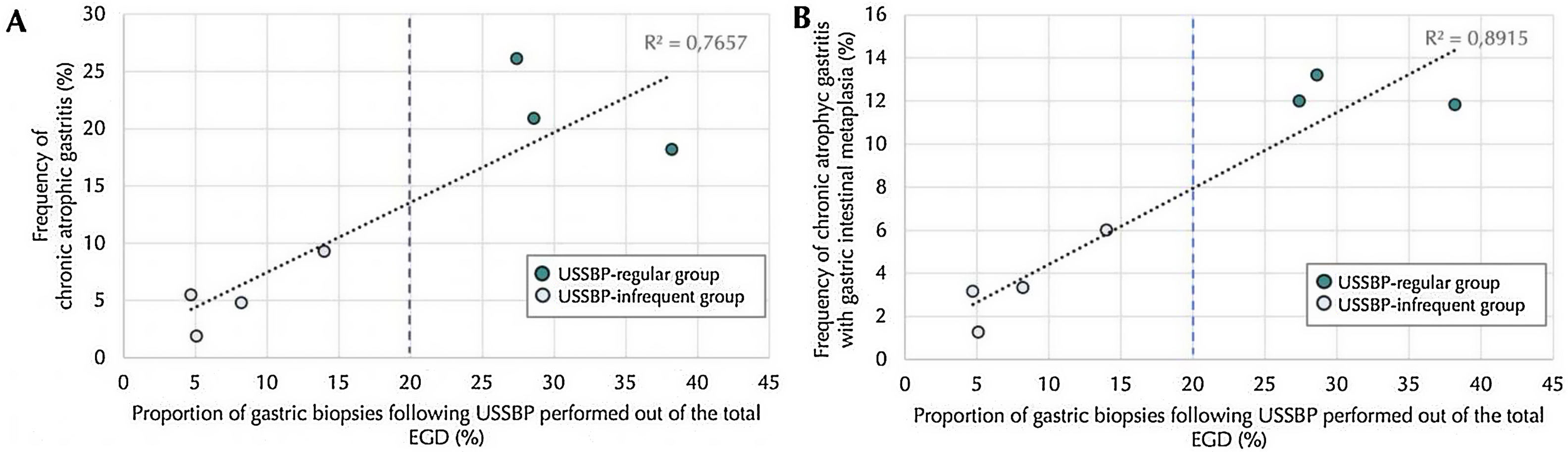
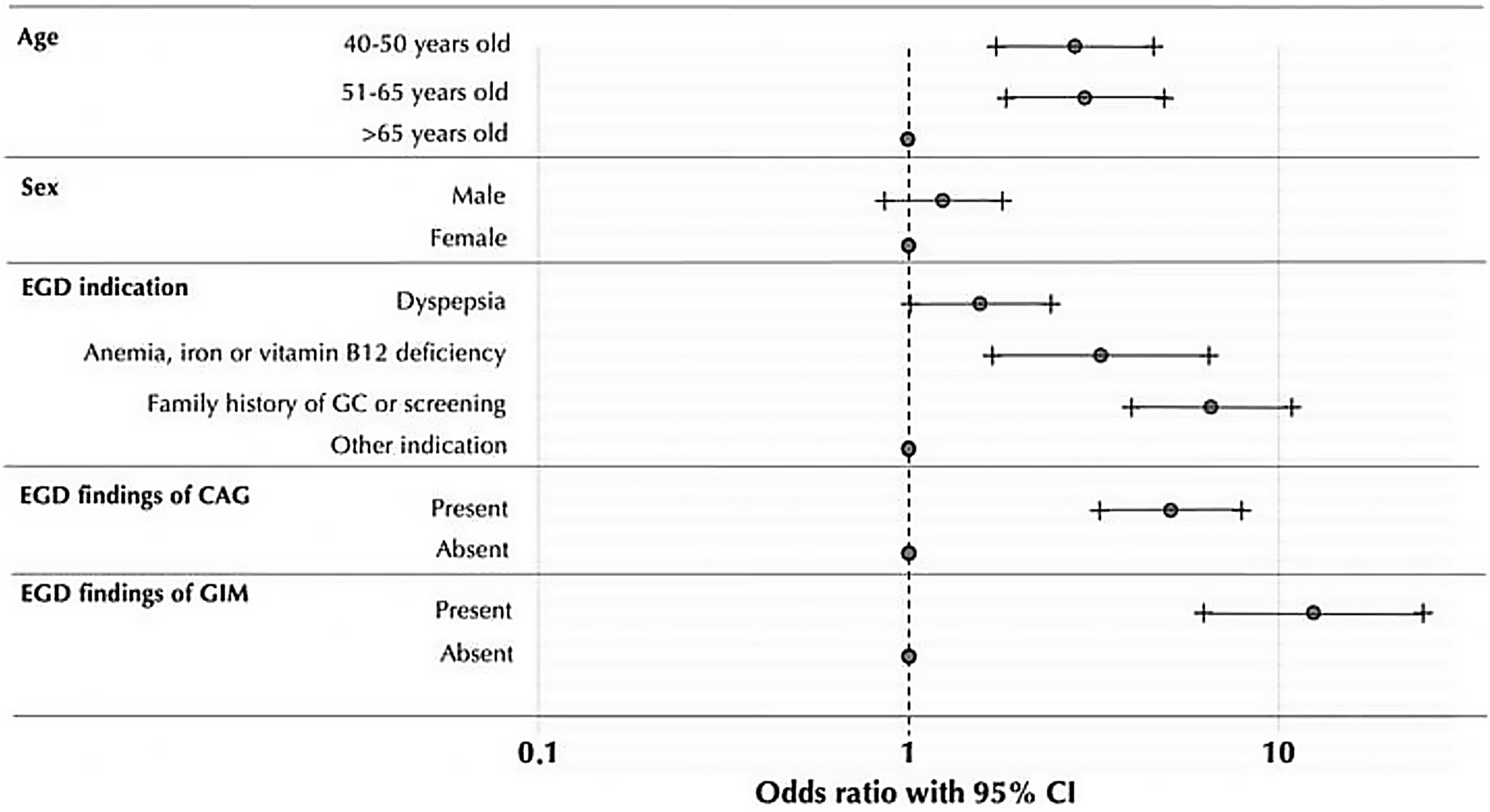
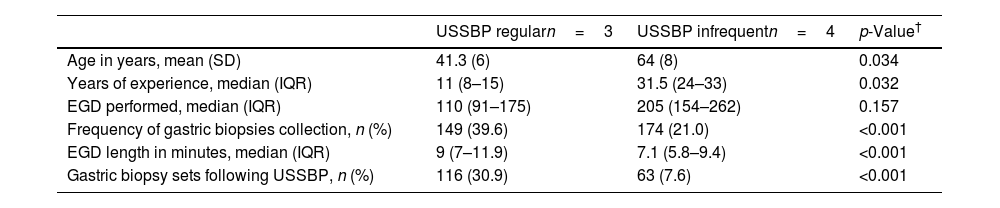
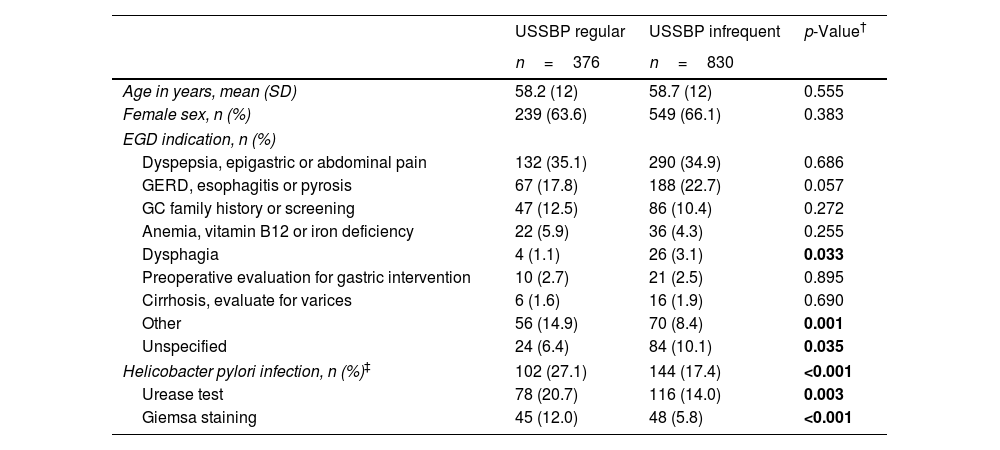
MethodsWe performed a real-world retrospective study at an academic urban tertiary hospital in Chile. We manually reviewed medical records from consecutive patients undergoing esophagogastroduodenoscopy (EGD) from January to December 2017. Seven endoscopists who performed EGDs were categorized into two groups (USSBP ‘regular’ and USSBP ‘infrequent’) based on USSBP adherence, using minimum 20% adherence as the prespecified threshold. Multivariable logistic regression models were used to estimate the odds ratios (aOR) and 95% confidence intervals (CI) for the association between endoscopist groups and the likelihood of diagnosing CAG, GIM or AIG.
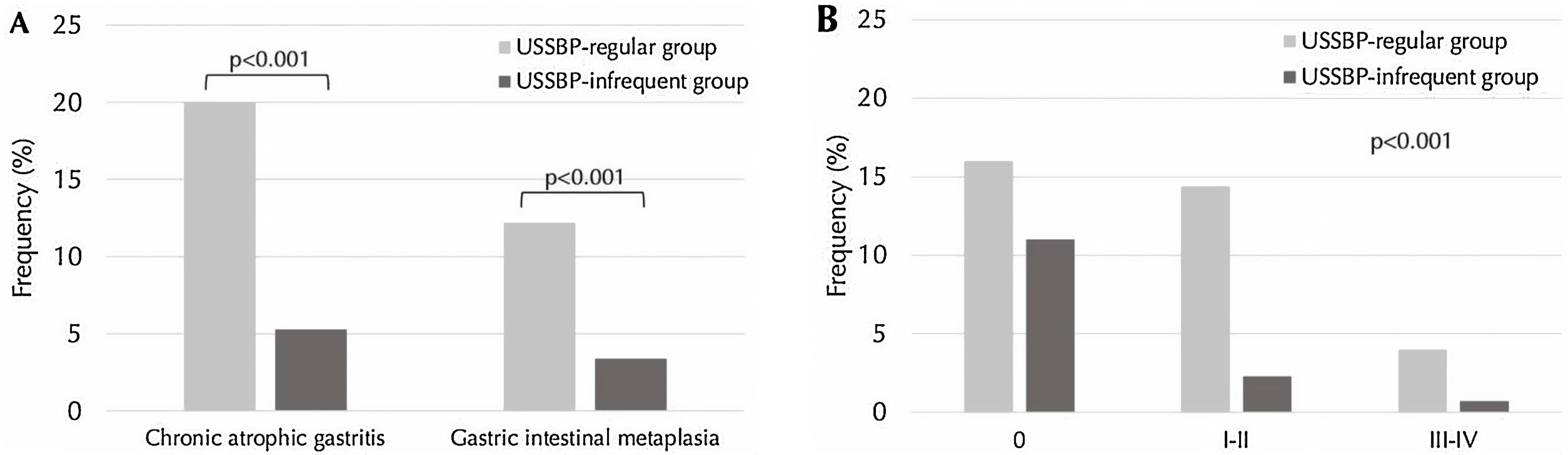
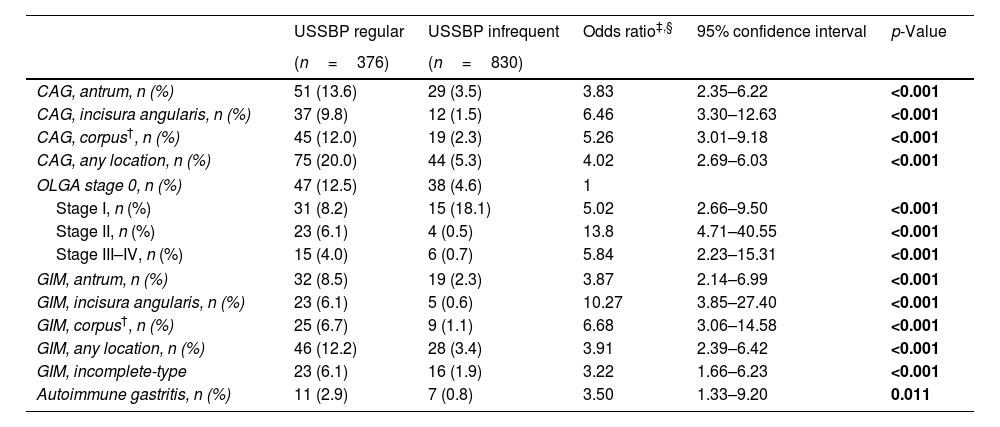
Results1206 patients were included in the study (mean age: 58.5; 65.3% female). The USSBP regular group demonstrated a higher likelihood of detecting CAG (20% vs. 5.3%; aOR 4.03, 95%CI: 2.69–6.03), GIM (12.2% vs. 3.4%; aOR 3.91, 95%CI: 2.39–6.42) and AIG (2.9% vs. 0.8%; aOR 6.52, 95%CI: 1.87–22.74) compared to infrequent group. Detection of advanced-stage CAG (Operative Link for Gastritis Assessment stage III/IV) was significantly higher in the USSBP regular vs. infrequent group (aOR 5.84, 95%CI: 2.23–15.31).
ConclusionsRoutine adherence to USSBP increases the detection rates of preneoplastic conditions, including CAG, GIM and AIG. Standardized implementation of USSBP should be considered in high gastric cancer risk populations.
El protocolo de biopsia del sistema de Sydney actualizado (Updated Sydney System biopsy protocol [USSBP]) estandariza la toma de muestras de biopsias gástricas para la detección de condiciones preneoplásicas (p. ej., la metaplasia intestinal gástrica (MIG)), pero el rendimiento diagnóstico en el mundo real no está bien descrito.
ObjetivoDeterminar si la aplicación regular del USSBP se asocia con una mayor detección de gastritis crónica atrófica (GCA), MIG y gastritis autoinmune (GAI).
MétodosEstudio retrospectivo del mundo real en un hospital terciario urbano académico en Chile. Revisamos manualmente los registros médicos de pacientes consecutivos sometidos a una endoscopía digestiva alta (EDA) desde enero hasta diciembre de 2017. Siete endoscopistas que realizaron EDA fueron categorizados en 2 grupos (USSBP «regular» y USSBP «infrecuente») según su adhesión al USSBP, utilizando un umbral predefinido de adhesión>20%. Se utilizaron modelos de regresión logística multivariable expresadas en odds ratio (OR) e intervalos de confianza del 95% (IC 95%) para la asociación entre los grupos de endoscopistas y la probabilidad de diagnosticar GCA, MIG o GAI.
ResultadosSe incluyeron 1.206 pacientes en el estudio (edad promedio: 58,5 años; 65,3% mujeres). El grupo USSBP «regular» demostró una mayor probabilidad de detectar GCA (20 vs. 5,3%; OR: 4,03; IC 95%: 2,69-6,03), MIG (12,2 vs. 3,4%; OR: 3,91; IC 95%: 2,39-6,42) y GAI (2,9 vs. 0,8%; OR: 6,52; IC 95%: 1,87-22,74) en comparación con el grupo USSBP «infrecuente». La detección de GCA en etapa avanzada (etapa III/IV de Operative Link for Gastritis Assessment [OLGA]) fue significativamente mayor en el grupo USSBP «regular» vs. USSBP «infrecuente» (OR: 5,84; IC 95%: 2,23-15,31).
ConclusionesLa adherencia rutinaria al USSBP aumenta las tasas de detección de condiciones preneoplásicas, incluyendo GCA, MIG y GAI. La implementación estandarizada del USSBP debería considerarse en poblaciones con alto riesgo de cáncer gástrico.