Despite better knowledge of the pathogenesis of severe alcoholic hepatitis (AH), corticosteroids are still the treatment recommended by clinical guidelines, pentoxifylline being the second-line option for non-responders to corticosteriods and for patients with contraindications. Pentoxifylline is a phosphodiesterase inhibitor with an anti-TNF effect and has been reported to reduce mortality and the incidence of hepatorenal syndrome in severe AH.
After the first report, several studies, of distinct quality, have tested the efficacy of pentoxifylline in different scenarios. The conclusions of these studies are that pentoxifylline seems to improve survival in comparison to placebo but has lower efficacy than corticosteroids, with no improvement in survival when added to corticosteroids or in non-responders to steroid therapy. The role of pentoxifylline in severe alcoholic hepatitis is even more doubtful after the results of a very recent controlled study that showed no beneficial effect on survival at 1, 3 and 12 months of follow up, although a very recent network meta-analysis reported a beneficial effect of pentoxifylline alone or with corticosteroids on short-term survival.
In conclusion, pentoxifylline has no clear beneficial effects in severe AH but could perhaps be used in patients with a contraindication to corticosteroids. However, the recommendations of clinical guidelines should be reconsidered and it is essential to search for new therapeutic targets for this disease.
A pesar de los avances en el conocimiento de la fisiopatología de la hepatitis alcohólica (HA), desde hace casi 4 décadas los corticoides siguen siendo el tratamiento recomendado en las guías clínicas, siendo la pentoxifilina la segunda opción terapéutica para los pacientes que no responden a los corticoides o que presentan una contraindicación para su administración. La pentoxifilina es un inhibidor de la fosfodiesterasa con un efecto anti-TNF y su uso en la HA se propuso a raíz de un estudio que demostró una reducción de la mortalidad y de la incidencia de síndrome hepatorrenal. Desde entonces, se han efectuado varios estudios con una calidad variable para determinar la eficacia de la pentoxifilina en diferentes escenarios. El resumen de estos estudios es que la pentoxifilina parece mejorar la supervivencia de los pacientes en comparación a los que reciben placebo, pero su eficacia es inferior a la de los corticoides, sin mejorar tampoco los resultados cuando se asocia a los corticoides o en los pacientes no respondedores. El tratamiento de la HA grave con pentoxifilina ha sido puesto todavía más en cuestión a raíz de los resultados de un estudio controlado muy amplio, publicado hace unos meses, que no demostró ningún efecto beneficioso de la pentoxifilina en relación con la supervivencia al mes, a los 3 meses y al año, aunque una posterior revisión sistemática y metaanálisis en red sí que mostró una mejoría de la supervivencia a corto plazo con la administración de pentoxifilina sola o en combinación con corticoides, En conclusión, la eficacia de la pentoxifilina en la HA grave es cuanto menos dudosa; puede tenerse en cuenta en los casos en que estén contraindicados los corticoides, pero se debe reconsiderar su indicación en las guías clínicas y buscar nuevas alternativas terapéuticas para esta enfermedad.
Alcoholic hepatitis (AH) is the most severe form of alcoholic liver disease. It is characterised by sudden decompensation of liver function that can occur in any stage of the disease, often when there is already cirrhosis, in patients with active, high alcohol consumption. The clinical spectrum of AH ranges from asymptomatic to severe forms, with a 6-month mortality rate of up to 40%.1 Despite advances in the understanding of the pathogenesis of AH, corticosteroids–in addition to abstinence from alcohol, nutritional support and the treatment of complications–have been the preferred therapy for almost 4 decades, and continue to be recommended as a first option in recent guidelines published by the American and European Associations for the Study of the Liver.2,3 However, a significant proportion of patients do not respond to corticosteroids, while many others present contraindications, such as infections or gastrointestinal bleeding at the time of diagnosis. Furthermore, some clinicians are reluctant to prescribe corticosteroids due to the risk of infections, although the impact of these depends mainly on the degree of liver impairment and response to treatment.4 It is therefore important to establish the severity of the AH using one of the clinical5 and histological prognostic indices6 available, and above all, to stop treatment if a response is not observed in 1 week in accordance with the Lille score. For these reasons, clinical guidelines continue to recommend pentoxifylline (Ptx) as an alternative to corticosteroids in AH.
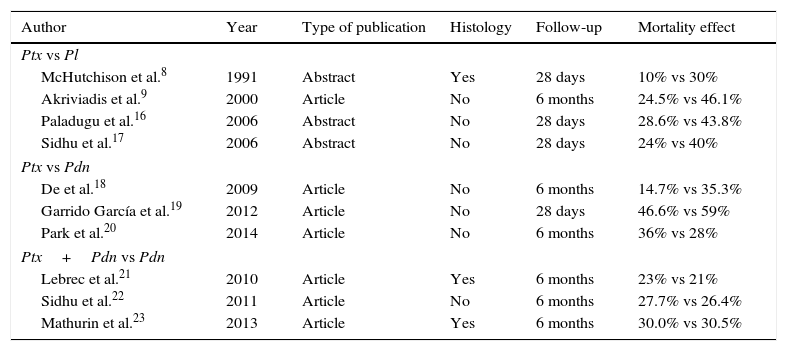
Ptx is a potent non-selective phosphodiesterase inhibitor that increases intracellular concentrations of cAMP and cGMP. The increase in cAMP modulates the cytokine inflammatory response, decreasing the concentration of the proinflammatory cytokine tumour necrosis factor (TNF), and increasing the concentration of the anti-inflammatory cytokine IL-10.7 Based on this mechanism of action and the positive results of the initial studies by McHutchison et al.8 and Akriviadis et al.,9 Ptx was proposed as an alternative treatment for AH. Since then, it has been used in different scenarios in the treatment of AH, comparing its efficacy vs placebo, vs prednisolone, together with prednisolone vs prednisolone alone or as rescue treatment when prednisolone fails (Table 1). The role of Ptx in AH has also been the object of several meta-analyses,10–12 editorials and comments,13–15 which are analysed below.
Summary of clinical trials evaluating the efficacy of pentoxifylline in severe alcoholic hepatitis.
| Author | Year | Type of publication | Histology | Follow-up | Mortality effect |
|---|---|---|---|---|---|
| Ptx vs Pl | |||||
| McHutchison et al.8 | 1991 | Abstract | Yes | 28 days | 10% vs 30% |
| Akriviadis et al.9 | 2000 | Article | No | 6 months | 24.5% vs 46.1% |
| Paladugu et al.16 | 2006 | Abstract | No | 28 days | 28.6% vs 43.8% |
| Sidhu et al.17 | 2006 | Abstract | No | 28 days | 24% vs 40% |
| Ptx vs Pdn | |||||
| De et al.18 | 2009 | Article | No | 6 months | 14.7% vs 35.3% |
| Garrido García et al.19 | 2012 | Article | No | 28 days | 46.6% vs 59% |
| Park et al.20 | 2014 | Article | No | 6 months | 36% vs 28% |
| Ptx+Pdn vs Pdn | |||||
| Lebrec et al.21 | 2010 | Article | Yes | 6 months | 23% vs 21% |
| Sidhu et al.22 | 2011 | Article | No | 6 months | 27.7% vs 26.4% |
| Mathurin et al.23 | 2013 | Article | Yes | 6 months | 30.0% vs 30.5% |
Pdn: prednisolone; Pl: placebo; Ptx: pentoxifylline.
Four clinical trials have been published comparing Ptx with placebo in AH, although 3 of these were in summarised form only.
In the first study published by McHutchison et al.,8 12 patients with a histological diagnosis of AH and Maddrey discriminant function score of over 32 treated with 1200mg/day of Ptx for 10 days were compared with 10 patients treated with placebo. One patient in the treated group and 3 in the control group died during the first month (p=ns); the trend towards lower mortality was attributed to less impairment of renal function.
The most complete study, and the main basis for justifying the administration of Ptx in AH, is the trial by Akriviadis et al.,9 which included 102 patients with severe AH, treated with 1200mg/day of Ptx or placebo for 28 days and followed up for 6 months. The most important finding of the study was a significant decrease in the 6-month mortality of patients treated with Ptx (12 of 49, 24.5%) compared to patients in the control group (24 of 52, 46.1%). This difference in mortality was attributed to a decrease in the risk of developing hepatorenal syndrome in patients treated with Ptx (12.2% vs 42.3%), while no differences were observed in serum TNF levels.
Paladugu et al.16 studied 30 patients treated with Ptx or placebo for 4 weeks, observing a mortality rate of 28.6% in the Ptx group compared to 43.8% in the control group (p=0.09), and reporting the incidence of hepatorenal syndrome only when it was the cause of death (85% in the Ptx group and 87.5% in the control group). In another study, Sidhu et al.17 included 25 patients treated with Ptx and 25 with placebo for 28 days; mortality was 24% and 40%, respectively, with hepatorenal syndrome the most common cause of death in the Ptx group.
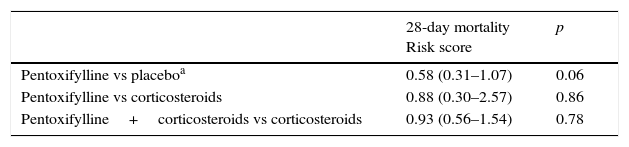
Jointly analysing studies evaluating 28-day mortality gives a relative risk of mortality and onset of hepatorenal syndrome in patients who received Ptx of 0.43 and 0.47, respectively (p=0.06 and p=0.01), which suggests a beneficial effect in relation to placebo (Table 2).
Risk score for mortality at 28 days of patients with severe alcoholic hepatitis treated with pentoxifylline.
| 28-day mortality Risk score | p | |
|---|---|---|
| Pentoxifylline vs placeboa | 0.58 (0.31–1.07) | 0.06 |
| Pentoxifylline vs corticosteroids | 0.88 (0.30–2.57) | 0.86 |
| Pentoxifylline+corticosteroids vs corticosteroids | 0.93 (0.56–1.54) | 0.78 |
Three studies have been published comparing Ptx with prednisolone. Two of these, while showing a trend towards lower 28-day mortality in patients treated with Ptx, have several methodological defects that make it difficult to interpret the results, and the third is a recently published non-inferiority study. In the first study, De et al.18 treated 70 patients with 1200mg of Ptx or 40mg of prednisolone for 28 days, continuing the study in an open phase with tapering doses of prednisolone, maintaining the same dose of Ptx. The 28-day mortality was 5.8% in the Ptx group and 20.5% in the prednisolone group, maintaining the differences at 6 months (14.7% vs 35.3%). In the other study conducted by Garrido García et al.19 in Mexico, no differences were observed in 28-day mortality.
Recently, Park et al.20 published the results of a non-inferiority study in 124 patients with severe AH, comparing short-term mortality in patients treated with Ptx with those treated with prednisolone at the recommended doses, 1200mg/day and 40mg/day, respectively, for 28 days. The 1-month survival rate, which was the primary endpoint, was 75.8% in the Ptx group and 88.1% in the prednisolone group, a difference that exceeded the margin of non-inferiority (15%) established in the methodology. The 6-month survival rate was 64% in the Ptx group and 72% in the prednisolone group, similar to the results of other studies. The authors concluded that the efficacy of Ptx is inferior to that of prednisolone, and that the latter should therefore be the drug of choice. There were no differences in the complications presented by both groups, including hepatorenal syndrome. This study included a high number of patients, but was not double-blind, did not include a placebo group, and there was no histological confirmation of the diagnosis.
Clinical studies comparing combined pentoxifylline and corticosteroid treatment vs corticosteroids aloneThree studies have been published comparing combined Ptx and prednisolone to prednisolone alone. In the first of these, Lebrec et al.21 compared treatment with Ptx vs placebo in 335 patients with alcoholic cirrhosis, Child Pugh C. Among these was a subgroup of 55 patients with biopsy-diagnosed AH and a Maddrey discriminant score of over 32, who were administered prednisolone plus Ptx or placebo. The probability of survival was similar in both groups at 2 months (84.6% and 86.2% in the Ptx and placebo groups, respectively) and at 6 months (76.9% vs 79.3%).
The second study was conducted by Sidhu et al.22 in 70 patients with severe AH, with no histological confirmation, randomised to receive prednisolone plus Ptx or prednisolone alone at the standard doses for 28 days. No differences were observed in mortality at either 28 days (10/36 in the combined treatment group and 9/34 in the prednisolone group) or at 6 months (25/36 and 26/34, respectively).
The most complete study is that conducted by Mathurin et al.,23 which included 270 patients with severe biopsy-proven AH, 137 of whom received combined treatment and 134 prednisolone alone. There were no differences in survival at 28 days (119/133 vs 120/137 patients) and 6 months (93/133 vs 95/137), and incidence of hepatorenal syndrome was similar in both groups (9.1% vs 10.3%).
The results of these studies suggest that adding Ptx to corticosteroids does not improve the efficacy of prednisolone.
Pentoxifylline as rescue treatment in non-responders to corticosteroidsLouvet et al.24 compared the efficacy of administration of Ptx in patients with no response to 7 days treatment with prednisolone. After withdrawing prednisolone, 29 non-responders were given 1200mg/day of Ptx and compared with a group of 58 non-responders with similar demographic and clinical characteristics. No differences in survival were observed at 2 months among patients who received Ptx after prednisolone and those who received prednisolone alone (35.5% vs 31%), showing that Ptx was not an effective rescue treatment.
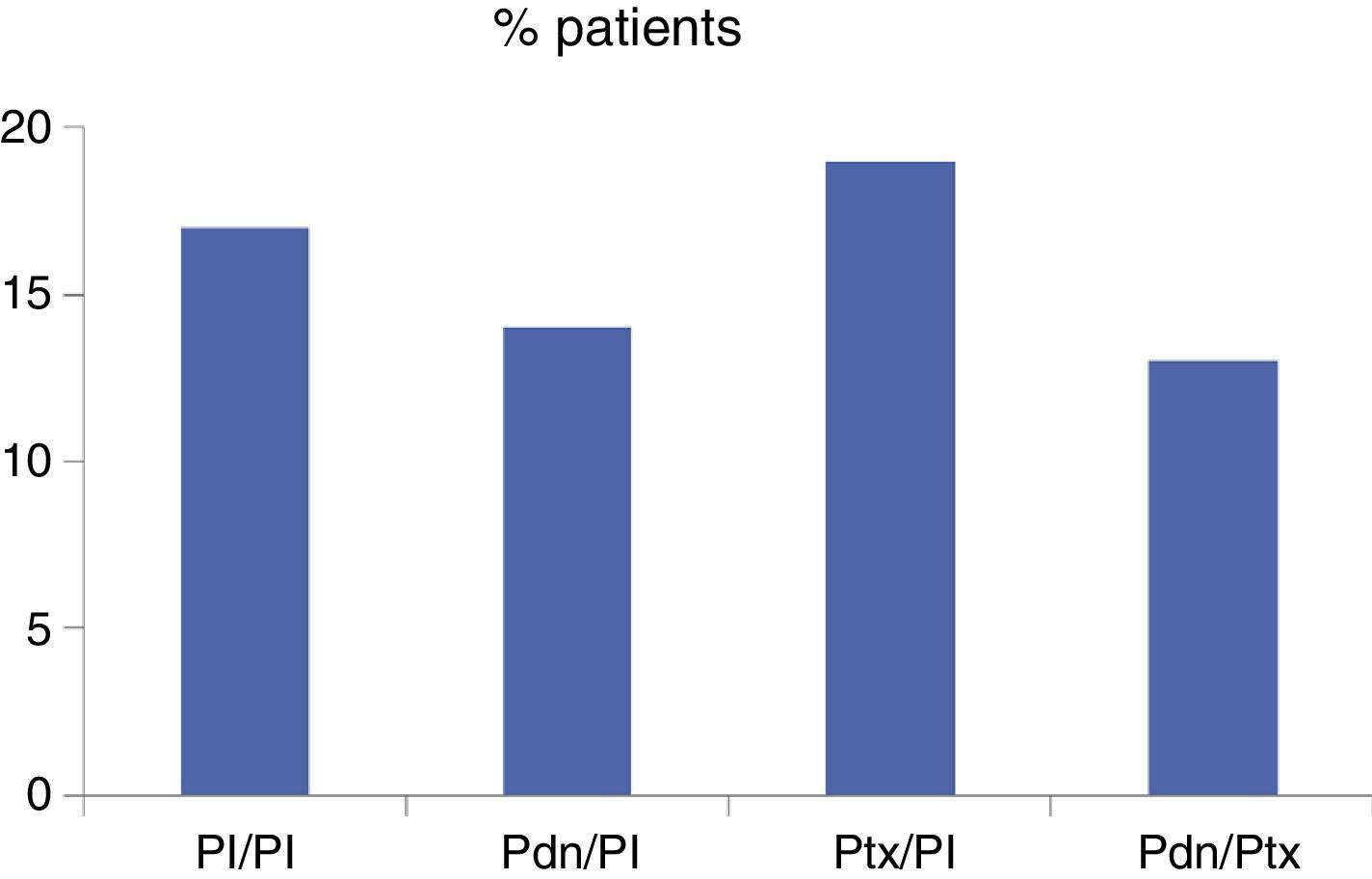
STOPAH studyIn April this year, data from the Steroids or Pentoxifylline for Alcoholic Hepatitis (STOPAH) trial were published.25 This is a placebo-controlled study conducted in 65 hospitals across the United Kingdom, in which 1103 patients were randomised to 4 groups: placebo/placebo (276 patients), prednisolone/placebo (277 patients), Ptx/placebo (276 patients) and prednisolone/Ptx (274 patients), and treated with standard doses of 40mg of prednisolone/day or 400mg of Ptx three times daily for 28 days. The primary endpoint of the study was mortality at 28 days; other endpoints were mortality at 90 days and at 1 year, as well as the incidence and type of complications. Patients were diagnosed with severe AH by clinical and biological criteria, but without histological confirmation. No effect on survival was observed in patients treated with Ptx (Fig. 1). Patients treated with prednisolone showed a trend towards increased survival at 28 days, which became statistically significant when adjusted for baseline prognostic factors, although this effect was not maintained in the medium- and long-term. The authors concluded that Ptx does not improve survival in severe AH, while prednisolone may have a beneficial effect on short-term mortality.
Singh et al.26 subsequently published the results of a systematic review and network meta-analysis comparing the effectiveness of different treatments available for severe AH (corticosteroids, Ptx and n-acetylcysteine, alone or in combination) with each other and with placebo, in terms of both short- and medium-term mortality. This methodology includes the simultaneous analysis of direct evidence comparing the treatments with each other, and indirect evidence comparing the treatments against a common denominator.27 The results suggest that both corticosteroids and Ptx alone or in combination improve short-term survival of AH, as does the combination of corticosteroids with acetylcysteine, but none of these treatments showed beneficial effects on long-term mortality, confirming the importance of abstinence and social support measures in the follow-up of these patients. The results of this analysis suggest that, despite the results of the STOPAH study, Ptx alone or in combination with corticosteroids could continue to be indicated in patients in whom corticosteroids are contraindicated.28
CommentsWith the exception of the earliest papers, the findings of studies and meta-analyses assessing the efficacy of Ptx in severe AH are contradictory and show no clear effects. These studies have a series of drawbacks that limit interpretation of the results and comparison between studies. In many of the studies analysed, including the STOPAH trial, no histological diagnosis was performed. Although biopsy is not essential for diagnosis, EASL guidelines recommend that liver biopsy be carried out in patients included in a study. Biopsy has unquestionable diagnostic and prognostic value,6 although a consensus regarding its indication in AH is needed. Another important aspect is the failure to describe how abstinence–the factor that most affects medium- and long-term mortality–was monitored. In addition, the primary endpoints of the studies are not homogeneous, as some assessed survival at 1 month, others at 2, and others at 6 months. Some of the studies that compared Ptx with prednisolone did not include a placebo group, and therefore cannot conclude that Ptx has no positive effect. Complications, especially the incidence of hepatorenal syndrome, were not well documented in many studies.
The most recent studies, which are also the largest and best designed, have shown Ptx to be less effective than prednisolone (Mathurin et al.,23 comparing Ptx with prednisolone and the non-inferiority study by Park et al.20), thus supporting the recommendations in clinical guidelines, while the STOPAH study has been unable to show a beneficial effect of Ptx on survival.24 Another interesting finding from the Park and STOPAH studies is the relatively poor efficacy of prednisolone on medium-term survival.
In conclusion, the role of Ptx in the treatment of AH is questionable, and future updates of clinical guidelines should change or refine their recommendation of this therapy. The results of the recent network meta-analysis suggest that its good tolerance may justify its use in patients with contraindications for corticosteroids, and in centres in which there are no ongoing clinical trials. This, together with the findings on corticosteroids in the latest studies, highlights the pressing need to seek therapeutic alternatives that include liver transplantation in selected patients,29 artificial liver support measures and, especially, drugs against new therapeutic targets.30
Conflict of interestsThe authors declare that they have no conflict of interests.
Please cite this article as: Caballeria J. ¿Tiene algún papel la pentoxifilina en el tratamiento de la hepatitis alcohólica? Gastroenterol Hepatol. 2016;39:560–565.