Colorectal adenomas are benign tumours with the potential to become malignant. Their incidence ranges from 2.9% to 11.5% depending on the series.1 Villous adenomas represent 10% of all colorectal adenomas and are normally asymptomatic, although 3% are hypersecretory.2 In 1954, McKittrick and Wheelock3 were the first to report hydroelectrolyte depletion secondary to severe diarrhoea caused by this type of tumour.
We present the case of a 72-year-old female patient with a history of hypertension, type 2 diabetes mellitus and hospitalisation two years prior due to pneumonia and hyponatraemia. She attend A&E following three days of epigastric pain together with melaena in the last 24h. The patient's relatives reported occasional vomiting and severe diarrhoea in the previous days. Although the patient presented bradylalia and bradyphrenia, she was awake and oriented during the physical examination. She was found to be haemodynamically stable with vital signs within normal range. The abdomen was rounded but soft and depressible with signs of peritoneal irritation. There were signs of skin and mucosa dehydration. During her stay in A&E, the patient presented a reduced level of consciousness, suffered tonic-clonic seizures and went into a coma. The complete blood count conducted in A&E revealed severe hyponatraemia with sodium levels of 101mEq/l; potassium 4.6mEq/l; plasma hypoosmolarity without metabolic acidosis and normal kidney function.
The patient was admitted to the intensive care unit after being intubated and put on mechanical ventilation. A cranial computed tomography was performed that found no acute lesions. Volume replacement with hypertonic saline was implemented, and hyponatraemia was gradually corrected until levels of 131mEq/l were reached. The patient regained consciousness as sodium levels were being corrected, coherently responding to verbal commands but with bradyphrenia.
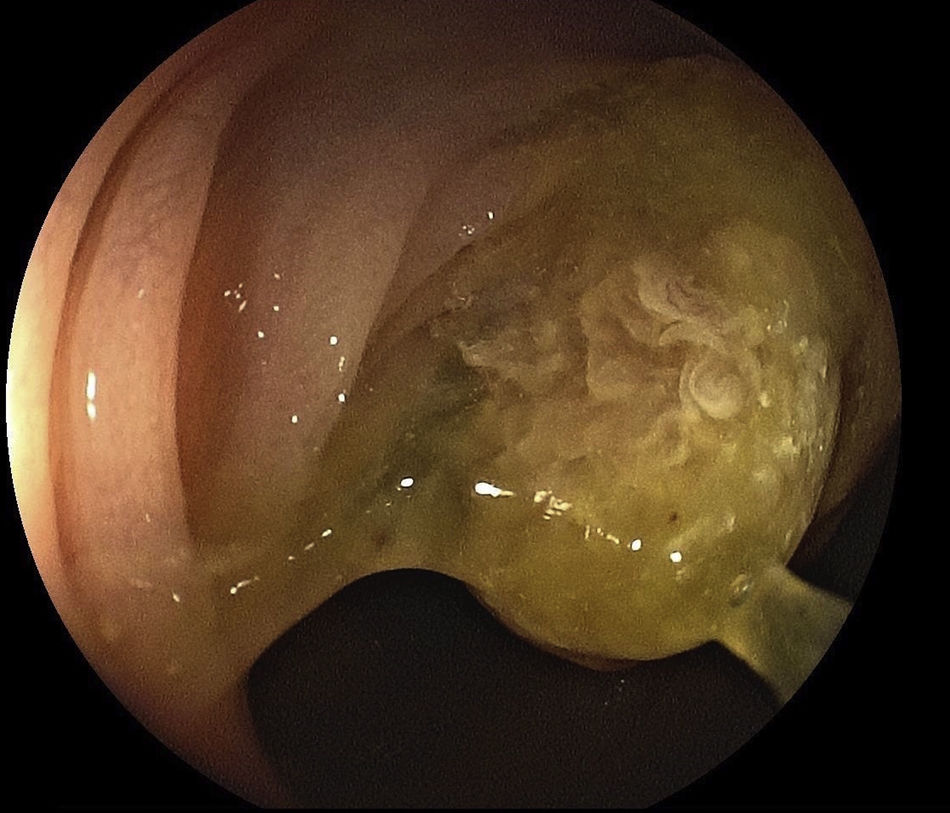
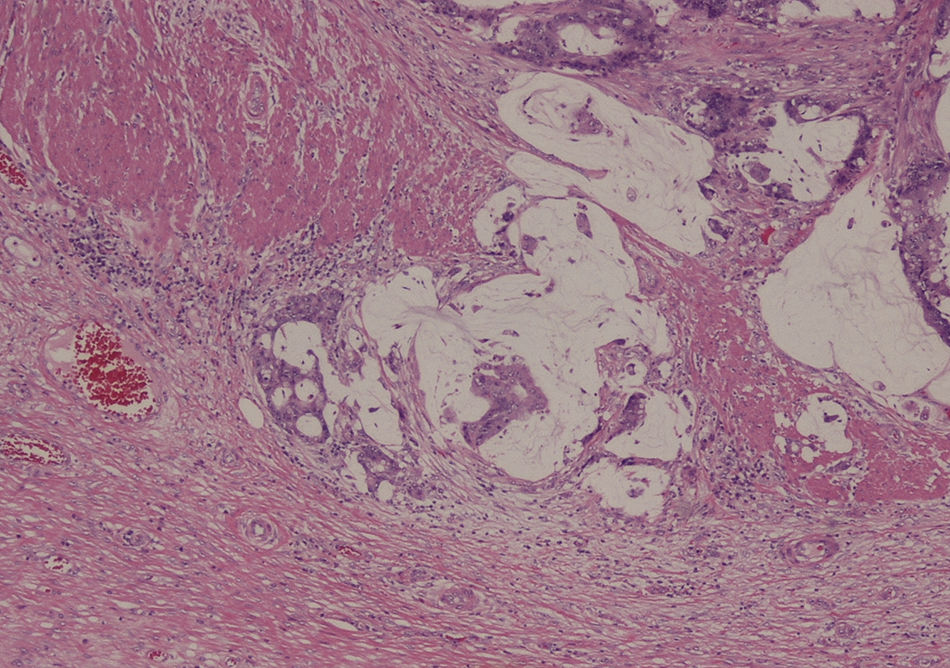
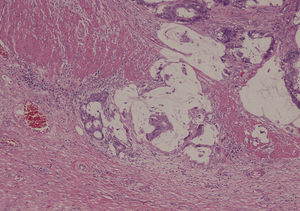
Given the patient's profuse diarrhoea, a colonoscopy was performed that revealed a villous polyp (0-IIa on the Paris classification) at the hepatic flexure measuring more than 3cm and endoscopically unresectable owing to its size, with no endoscopic signs of malignancy. The lesion showed abundant surface mucus and signs of recent bleeding (Fig. 1). The endoscopic biopsy revealed a fragment of villous adenoma in the large intestine with low grade dysplasia. Given that the polyp was secreting mucus, a laparoscopic right hemicolectomy was performed, subsequent to which the patient's condition improved and all symptoms abated. Sodium plasma levels after the surgery were 134mEq/l. The anatomopathological study of the surgical specimen revealed a villous adenoma measuring 4.5cm×3.5cm×1.2cm, in which a moderately-differentiated mucinous adenocarcinoma was found (low grade dysplasia) that measured 1.5cm microscopically (Fig. 2). The tumour invaded the muscle itself and just reached the subserosal fat, isolating 16 lymph nodes, all without histological features of malignancy (pT3N0).
McKittrick and Wheelock3 reported a syndrome characterised by mucous diarrhoea associated with hyponatraemia, hypokalaemia, severe dehydration and pre-renal azotaemia. Although our patient presented severe hyponatraemia and physical signs of dehydration, serum potassium and creatinine levels were normal at admission.
Colorectal villous adenomas are benign tumours that can histologically be divided into secretors and non-secretors. Secreting tumours produce a large amount of mucous and are composed of a greater number of mucus-secreting cells, resulting in higher levels of cyclic AMP and adenylyl cyclase. The mediator involved in hypersecretory diarrhoea is prostaglandin E2 (PGE2), levels of which can be up to three times higher in secretory adenomas than in non-secretory adenomas.4 This causes profuse diarrhoea resulting in severe hydroelectrolyte depletion, which is definitively treated by polyp resection. To alleviate symptoms while awaiting resection, 400mg/day of indomethacin has been proposed due to its inhibitory action on PGE2,5 which could reduce adenoma secretion levels.
This type of tumour is most commonly found in the sigmoid and the rectum. Tumour size, location and how villous the tumour is have been proposed as factors that could influence symptoms.1 Diarrhoea and mucosal secretion seem to be more common in large lesions and those located in the rectum, probably because the distal location inhibits the colon's ability to absorb liquids. Nevertheless, small lesions in the right colon, such as in our patient, may manifest with very acute symptoms. Although the known side effects of secretory diarrhoea include central nervous system dysfunction due to hyponatraemia, such extreme dysfunction as metabolic coma and seizures have not been reported in the literature.
Surgical resection of the lesion is considered to be the definitive treatment of choice.6 Depending on the location of the lesion, the most appropriate surgical resection technique is chosen based on the principles of surgical oncology.
Whenever the patient has a history of chronic or hypersecretory diarrhoea, McKittrick-Wheelock syndrome should be considered in the differential diagnosis of severe metabolic disorders associated with central nervous system dysfunction. For early diagnosis, a diagnostic colonoscopy should be performed in all patients with these symptoms. Although polyp size has been correlated to symptom severity, small villous adenomas located in the proximal colon may trigger extremely acute symptoms, as with our patient.
Please cite this article as: López-Fernández J, Fernández-San Millán D, Navarro-Sánchez A, Hernández Hernández JR. Síndrome de McKittrick-Wheelock: una causa infrecuente de coma metabólico. Gastroenterol Hepatol. 2017;40:349–351.